Chapter 13: Shock and Resuscitation
smartensmd and Jay Steuer
13.1 Introduction
Shock is a life-threatening medical condition characterized by a sudden and severe reduction in blood flow throughout the body. This leads to a lack of sufficient oxygen and nutrients reaching the vital organs and tissues, causing cellular damage and potentially organ failure. This is considered a process of dying and is essential that emergency medical responders understand, recognize, and treat these patients effectively.
Learning Objectives
- Define shock.
- Review anatomy and physiology.
- Identify disruptions that can cause shock.
- Differentiate the categories of shock.
- Describe shock due to fluid loss.
- Describe shock due to pump failure.
- Describe shock due to container failure.
- Discuss key components of patient assessment for shock.
- Describe and demonstrate the steps to follow in the emergency care of the patient with various types of shock.
- Identify age-related variations.
Definition of Perfusion and Shock
Perfusion is fundamentally defined as the physiological process by which blood, carrying oxygen, glucose, and other vital nutrients, is delivered to the body’s individual cells. This delivery system ensures that each cell has the necessary resources to perform its metabolic functions and maintain tissue viability. Simultaneously, the circulatory system plays a critical role in the removal of metabolic waste products, most notably carbon dioxide, from these same cells. This bidirectional exchange is necessary for cellular homeostasis and overall organ system function.
Shock, in the context of emergency medical services, represents an emergent state of systemic hypoperfusion. This occurs when the circulatory system fails to adequately deliver oxygenated blood to the body’s tissues, resulting in a mismatch between oxygen supply and metabolic demand. The consequences of this inadequate perfusion deprive the cells of essential nutrients and then waste products accumulate. This cellular dysfunction, if prolonged and uncorrected, initiates a cascade of detrimental physiological events.
The progression of hypoperfusion, if left untreated, inevitably leads to cellular injury and ultimately, cell death. Initially, the body may attempt to compensate for reduced perfusion through various physiological mechanisms, such as increasing heart rate and vasoconstriction. However, these compensatory mechanisms are often temporary and can eventually become overwhelmed. As hypoperfusion persists, vital organs begin to suffer irreversible damage due to prolonged oxygen and nutrient deprivation, ultimately leading to multi-organ failure and death.
Therefore, a fundamental understanding of perfusion and the recognition of shock as a state of hypoperfusion are important. Early identification of the underlying cause of hypoperfusion and the prompt initiation of appropriate interventions aimed at restoring adequate tissue perfusion are critical determinants of patient survival and long-term outcomes. EMS professionals must possess a thorough knowledge of the pathophysiology of shock to effectively assess patients, implement treatment strategies, and collaborate with other healthcare providers.
Anatomy and Physiology Review
The cardiovascular system, comprising the heart and blood vessels, forms the central component of perfusion. The heart, a muscular organ, acts as a dual pump. The right side receives deoxygenated blood from the body and propels it to the lungs for oxygenation (pulmonary circulation), while the left side receives oxygenated blood from the lungs and pumps it throughout the body (systemic circulation). Blood vessels, a network of arteries, capillaries, and veins, facilitate the transport of blood. Arteries, with their muscular walls, carry blood away from the heart, branching into smaller arterioles and then into the capillary beds, where the crucial exchange of gases and nutrients occurs at the tissue level. Veins, with thinner walls and lower pressure, return deoxygenated blood back to the heart.
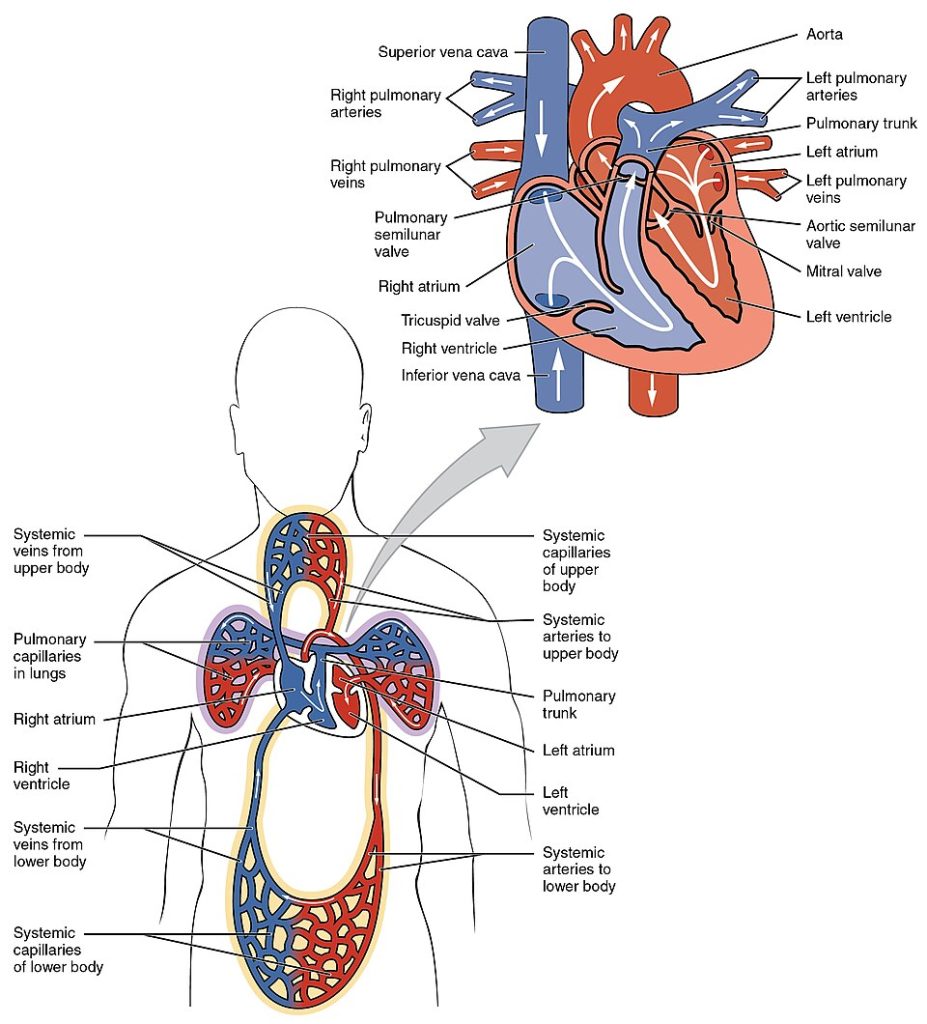
Respiration is the physiological process that enables gas exchange, vital for sustaining cellular life. At the alveolar level within the lungs, oxygen from inhaled air diffuses across the thin alveolar and capillary membranes into the bloodstream, binding to hemoglobin in red blood cells. Simultaneously, carbon dioxide, a waste product of cellular metabolism, diffuses from the blood into the alveoli to be exhaled. This newly oxygenated blood then enters the pulmonary circulation, returning to the left side of the heart to be pumped into the systemic circulation, delivering oxygen to all tissues and organs in the body.
Normal perfusion, the adequate delivery of oxygenated blood and removal of waste products at the cellular level, relies on three essential components: a functioning pump (the heart), an adequate blood volume, and an intact container (the blood vessels). The heart must generate sufficient pressure and cardiac output to circulate blood effectively.
The autonomic nervous system plays a critical role in regulating heart rate and contractility, particularly during states of stress or shock. Adequate blood volume ensures sufficient oxygen-carrying capacity and pressure within the vascular system. Blood consists of formed elements – red blood cells (carrying oxygen), white blood cells (involved in immunity), and platelets (essential for clotting) – suspended in plasma, the fluid component that also transports nutrients, hormones, and waste products. While platelets initiate clot formation to stop bleeding, these initial clots can be unstable and prone to rupture if underlying vessel damage is extensive.
The integrity and responsiveness of the blood vessels, the “container,” are equally critical for maintaining perfusion. Arteries and arterioles possess smooth muscle in their walls, allowing them to contract (vasoconstriction) and dilate (vasodilation) to regulate blood flow to different tissues based on their metabolic demands. Capillary beds, the primary sites of perfusion, have thin walls facilitating the exchange of substances. Veins, although low-pressure vessels, also contain smooth muscle and are influenced by the autonomic nervous system, aiding in the return of blood to the heart, sometimes against gravity. Sphincters at the entrance to capillary beds further regulate blood flow at the local tissue level, ensuring that oxygen and nutrients are delivered where they are most needed.
Ultimately, the control of blood flow and perfusion is linked to the metabolic demands of individual cells and tissues. Local factors, such as the concentration of oxygen, carbon dioxide, and other metabolic byproducts, influence the dilation or constriction of arterioles and precapillary sphincters, ensuring that each cell receives the necessary resources to function. This dynamic regulation, coupled with the systemic control exerted by the autonomic nervous system on the heart and blood vessels, maintains adequate perfusion throughout the body, supporting cellular health and overall organ function.
Disruptions Leading to Shock: A Foundational Overview
Shock, a life-threatening condition characterized by inadequate tissue perfusion and oxygenation, can arise from a variety of underlying disruptions within the circulatory system. The etiology of shock can be broadly categorized into issues affecting the circulating volume, the pumping capability of the heart, and the integrity of the vascular container. Each of these categories encompasses specific pathological processes that ultimately lead to a mismatch between oxygen supply and demand at the cellular level. Prompt identification of the primary disruption is crucial in guiding appropriate interventions and improving patient outcomes.
One primary cause of shock involves an absolute or relative deficiency in circulating fluid volume. This can manifest as inadequate fluid or blood, resulting from direct blood loss due to trauma, gastrointestinal hemorrhage, or surgical complications. Similarly, significant dehydration from vomiting, diarrhea, or inadequate fluid intake can lead to a reduction in intravascular volume. This decrease in preload directly impacts cardiac output, as there is insufficient fluid returning to the heart to be effectively pumped to the tissues. The body attempts to compensate through various mechanisms, but if the fluid loss is severe or prolonged, these compensatory mechanisms become overwhelmed, leading to hypovolemic shock.
Another critical category of shock-inducing disruptions centers on the failure of the heart to effectively function as a pump. This can occur due to direct damage to the cardiac muscle itself, such as in myocardial infarction (heart attack) or severe blunt cardiac trauma. Additionally, disruptions to the heart’s electrical conduction system, including severe bradycardia, tachycardia, or complete heart block, can impair the coordinated contraction necessary for adequate cardiac output. These conditions result in cardiogenic shock, where the heart is unable to pump sufficient blood to meet the metabolic demands of the body, despite potentially adequate circulating volume.
Finally, shock can result from issues affecting the vascular container, leading to a relative hypovolemia. This occurs when the blood vessels inappropriately dilate or become excessively permeable, increasing the capacity of the vascular system without a corresponding increase in circulating volume. Loss of nervous control over vascular tone, as seen in neurogenic shock following spinal cord injury, can lead to widespread vasodilation. Similarly, severe allergic reactions (anaphylaxis) trigger the release of potent vasodilators and increase capillary permeability, causing distributive shock. Massive infections (septic shock) and severe hypothermia can also disrupt vascular tone and lead to widespread vasodilation and maldistribution of blood flow, contributing to distributive shock and impaired tissue perfusion.
Stages of Shock
Shock, a critical condition characterized by inadequate tissue perfusion leading to cellular hypoxia, can be broadly categorized into progressive stages based on the body’s compensatory mechanisms and the severity of physiological imbalance. The initial phase, compensated shock, represents the body’s attempt to maintain homeostasis despite reduced perfusion. Clinically, this may manifest as normal pupils, an increased heart rate and respiratory rate as the body tries to circulate oxygen more efficiently, and a relatively normal blood pressure maintained by vasoconstriction. Subtle signs may include decreased gastrointestinal motility and mild anxiety or restlessness reflecting the body’s initial stress response. Recognizing these early signs is crucial for timely intervention to prevent progression to more severe stages.
If the underlying cause of shock persists or worsens, the body’s compensatory mechanisms begin to fail, leading to decompensated shock. This stage is characterized by more overt signs of hypoperfusion. Pupils may become dilated due to sympathetic nervous system activation and cerebral hypoxia. A hallmark of decompensated shock is a decreasing blood pressure as the body can no longer maintain adequate vascular tone. Furthermore, the patient’s level of consciousness will begin to diminish, ranging from lethargy to obtundation, reflecting inadequate oxygen delivery to the brain. Prompt and aggressive treatment is essential at this stage to reverse the downward trajectory and prevent irreversible organ damage.
The final and most critical stage is irreversible shock, where cellular and organ damage has become so profound that survival is unlikely despite medical intervention. Physiologically, this stage is marked by profound hypotension, often with a systolic blood pressure below 70 mmHg, indicating a severe failure of the cardiovascular system. Pupils will typically be fixed and dilated, reflecting significant neurological injury. Paradoxically, bradycardia may develop as the heart muscle becomes ischemic and loses its ability to effectively contract. The patient will be unresponsive to stimuli, signifying widespread organ failure and impending death. Recognizing the signs of irreversible shock helps guide appropriate treatment decisions and communication with the patient’s family.
Hypovolemic and Hemorrhagic Shock
Shock resulting from inadequate circulating blood volume is broadly categorized as hypovolemic shock. This occurs when the fluid component of blood is insufficient to maintain adequate perfusion of vital organs. Hypovolemic shock can arise from a variety of non-hemorrhagic causes, leading to a decrease in intravascular volume without the loss of red blood cells. Examples of non-hemorrhagic fluid loss include severe dehydration due to vomiting, diarrhea, or inadequate fluid intake; third-space fluid shifts as seen in conditions like severe burns or ascites; and excessive perspiration, particularly in hot environments or during strenuous activity. The signs and symptoms of hypovolemic shock are progressive and depend on the degree of fluid loss. Early signs may include tachycardia, mild anxiety, and cool, pale skin. As fluid loss worsens, patients may exhibit hypotension, altered mental status (restlessness, confusion), rapid and weak pulse, oliguria, and eventually, unresponsiveness. Recognizing the underlying cause and initiating prompt fluid resuscitation are critical in managing hypovolemic shock.
Hemorrhagic shock is a specific subtype of hypovolemic shock characterized by the loss of whole blood from the circulatory system. This loss of both fluid volume and oxygen-carrying capacity poses an immediate threat to tissue perfusion and oxygen delivery. Examples of hemorrhagic shock can be broadly categorized as either external or internal. External hemorrhage is readily apparent and can result from traumatic injuries such as lacerations, penetrating wounds, and fractures involving major blood vessels. Internal hemorrhage, however, can be more insidious and challenging to diagnose, occurring in locations such as the gastrointestinal tract (e.g., bleeding ulcers, ruptured esophageal varices), the thoracic cavity (e.g., hemothorax from trauma), the abdominal cavity (e.g., ruptured spleen, ectopic pregnancy), or the retroperitoneal space (e.g., pelvic fractures). The severity of hemorrhagic shock is directly related to the volume and rate of blood loss.
The signs and symptoms of hemorrhagic shock closely mirror those of general hypovolemic shock but often present more rapidly and may be more pronounced due to the combined loss of volume and red blood cells. Early signs may include a slightly elevated heart rate, narrowed pulse pressure, and subtle anxiety. As blood loss progresses, patients will develop more overt signs such as significant tachycardia, hypotension, tachypnea, cool and clammy skin, marked pallor, delayed capillary refill, and increasing agitation or confusion. In severe cases, the patient may become lethargic, unresponsive, and develop profound hypotension with a thready or absent pulse. The presence of external bleeding may be obvious, but a high index of suspicion is crucial for recognizing internal hemorrhage based on the mechanism of injury and clinical presentation.
Effective management of both hypovolemic and hemorrhagic shock hinges on rapid recognition, identification of the underlying cause, and prompt intervention. For hypovolemic shock, treatment focuses on patient positioning and facilitating the access to advanced life support who can address the fluid deficit through intravenous fluid administration, while simultaneously treating the underlying cause of fluid loss. In hemorrhagic shock, the primary goals are to stop the bleeding and restore circulating blood volume and oxygen-carrying capacity. This may involve direct pressure or a tourniquet to control external bleeding. Continuous monitoring of vital signs and level of consciousness help guide treatment and assess the patient’s response to interventions.
Pump Failure (Cardiogenic Shock)
Cardiogenic shock represents inadequate tissue perfusion resulting directly from the heart’s inability to pump blood effectively. This “pump failure” drastically reduces cardiac output, leading to insufficient oxygen and nutrient delivery to vital organs. Common examples of conditions that can precipitate cardiogenic shock include acute myocardial infarction (AMI), particularly large anterior wall infarctions or those involving significant left ventricular dysfunction; severe heart failure exacerbations; advanced valvular heart disease; and certain dysrhythmias that severely compromise cardiac contractility. Recognizing the underlying cause is essential for guiding appropriate management strategies aimed at improving cardiac function and restoring adequate perfusion.
The signs and symptoms of cardiogenic shock reflect both the reduced cardiac output and the body’s compensatory mechanisms. Patients typically present with hypotension (systolic blood pressure <90 mmHg or a decrease of >30 mmHg from baseline), a rapid and weak pulse, cool and clammy skin due to peripheral vasoconstriction, and altered mental status ranging from anxiety to unresponsiveness. Tachycardia is a common compensatory response as the heart attempts to maintain cardiac output despite reduced stroke volume. A key and often prominent feature unique to cardiogenic shock, especially when related to left ventricular failure, is the presence of pulmonary edema identified by wet breath sounds.
Pulmonary edema in cardiogenic shock arises from the failing left ventricle’s inability to effectively eject blood, leading to an increase in pressure within the left atrium and pulmonary veins. This elevated hydrostatic pressure forces fluid from the pulmonary capillaries into the interstitial spaces and alveoli of the lungs. Clinically, this manifests as dyspnea (shortness of breath), tachypnea (rapid breathing), and the presence of crackles or rales upon auscultation of the lungs. In severe cases, frothy, pink-tinged sputum may be expectorated. The presence of pulmonary edema, while not exclusive to cardiogenic shock, strongly suggests a primary cardiac etiology for the shock state and necessitates interventions focused on improving cardiac function and reducing pulmonary congestion.
Container Failure (Distributive Shock)
Distributive shock, also known as “container failure,” occurs when the intravascular volume is appropriately distributed but the capacity of the vascular system has increased dramatically, leading to a relative hypovolemia. This expansion of the vascular space results in a decrease in systemic vascular resistance (SVR) and inadequate tissue perfusion, despite potentially normal or even elevated cardiac output in the early stages. The underlying mechanisms for this vasodilation vary depending on the specific type of distributive shock. Recognizing the unique characteristics of each subtype is crucial for prompt and appropriate management in the prehospital setting. This section will explore three key categories of distributive shock: anaphylactic shock, neurogenic shock, and septic shock.
1. Anaphylaxis: Anaphylactic shock is a severe and potentially life-threatening systemic hypersensitivity reaction that occurs rapidly after exposure to an allergen in a sensitized individual. Common examples of triggers include insect stings (e.g., bees, wasps), food allergens (e.g., peanuts, shellfish), medications (e.g., penicillin), and latex.
The signs and symptoms of anaphylaxis are widespread and can involve multiple organ systems. These may include skin manifestations such as urticaria (hives), pruritus (itching), and angioedema (swelling of the lips, tongue, and face); respiratory compromise characterized by dyspnea (difficulty breathing), wheezing, and stridor (a high-pitched whistling sound during inhalation indicating upper airway obstruction); cardiovascular instability with hypotension (low blood pressure) and tachycardia (rapid heart rate); and gastrointestinal symptoms such as nausea, vomiting, and abdominal cramping.
What is unique to anaphylaxis is the frequent presence of dermatological signs like hives and the potential for upper airway obstruction manifested as stridor, neither of which are consistently present in other forms of distributive shock.
2. Neurogenic Shock: Neurogenic shock is a type of distributive shock resulting from the disruption of the autonomic nervous system’s control over vascular tone. This typically occurs after a significant injury to the spinal cord, particularly above the T6 level, which interrupts the sympathetic pathways responsible for maintaining vasoconstriction.
Examples of causes include traumatic spinal cord injuries, spinal anesthesia, and certain neurological conditions. The signs and symptoms of neurogenic shock reflect the loss of sympathetic tone. Patients often present with hypotension due to widespread vasodilation and a resultant decrease in SVR. Unlike other forms of shock that typically present with tachycardia as a compensatory mechanism, neurogenic shock is uniquely characterized by bradycardia (a slow heart rate). This occurs because the parasympathetic nervous system remains unopposed, leading to a decrease in heart rate despite the low blood pressure. Other findings may include warm, dry skin below the level of injury due to the vasodilation and loss of sympathetic innervation.
3. Sepsis: Septic shock is a life-threatening condition that arises from the body’s overwhelming and dysregulated response to an infection. A wide variety of microorganisms can cause sepsis, including bacteria (e.g., pneumonia, urinary tract infections), viruses (e.g., influenza), fungi, and parasites.
The initial signs and symptoms of sepsis can be subtle but often progress rapidly. These may include altered mental status, tachypnea (rapid breathing), and tachycardia. As sepsis progresses to septic shock, patients develop persistent hypotension despite adequate fluid resuscitation and signs of end-organ dysfunction.
What is unique about sepsis is the frequent presence of temperature dysregulation, often manifesting as either hyperthermia (fever, temperature > 100.4°F or 38°C) or hypothermia (low body temperature < 96.8°F or 36°C).
Given the high morbidity and mortality associated with sepsis, early recognition is paramount. EMS providers should be vigilant for obvious or suspected infection AND meeting two or more of the following criteria: Temperature < 96.8°F (36°C) or > 100.4°F (38°C), heart rate > 90 beats per minute, and respiratory rate > 20 breaths per minute. Identification of a potential sepsis should prompt timely and aggressive management.
View the following YouTube videos to learn more about the stages of shock:
Types of Shock Explained Simply | NREMT EMT Review
THE 4 STAGES OF SHOCK
Patient Assessment: A Systematic Approach
Effective patient assessment requires a systematic and thorough approach to identify and manage life-threatening conditions. The assessment process begins with a meticulous scene size-up, where the EMS provider evaluates the safety of the environment, determines the mechanism of injury or nature of illness, and identifies the number of patients. Following scene safety, the primary assessment focuses on the rapid identification and treatment of immediate life threats. This involves evaluating the patient’s airway, breathing, and circulation (ABCs), as well as assessing their level of consciousness and identifying any gross external hemorrhage. A rapid scan of the patient is crucial during this phase to detect critical issues requiring immediate intervention.
Once immediate life threats are addressed, obtaining a pertinent history and vital signs is the next critical step. This involves gathering information about the patient’s chief complaint, past medical history, medications, allergies, last oral intake, and events leading up to the incident (SAMPLE history). Concurrently, a comprehensive set of vital signs, including heart rate, respiratory rate, blood pressure, temperature, and pulse oximetry, provides essential physiological data to guide further assessment and treatment. For pediatric patients aged 1-10, understanding age-specific normal ranges for vital signs is paramount. A key “Pediatric Pearl” to remember for this age group is the formula for estimating normal systolic blood pressure (SBP): 90 + (2 x age in years). Similarly, hypotension in this age range is generally defined as an SBP less than 70 + (2 x age in years). Recognizing these age-related parameters is crucial for identifying early signs of decompensation in children.
The subsequent secondary assessment involves a more detailed head-to-toe examination to identify any additional injuries or medical conditions that may not have been apparent during the primary assessment. This may include palpation, auscultation, and visual inspection of various body systems. Finally, continuous reassessment is essential throughout patient care. This involves regularly repeating the primary assessment, reassessing vital signs, and monitoring the effectiveness of any interventions provided. Reassessment allows EMS providers to detect changes in the patient’s condition and adjust the treatment plan accordingly, ensuring the best possible outcome. Following your normal assessment process will assure you identify the signs and symptoms of shock as discussed.
Initial Management of the Trauma Patient
The immediate management of a trauma patient begins with a rapid primary survey to identify and address life-threatening conditions. Simultaneously, and as needed, manual in-line spinal stabilization should be initiated and maintained until the patient is appropriately secured to a long spine board or other spinal motion restriction device. This step aims to minimize potential secondary spinal cord injury in patients with suspected or confirmed spinal trauma. Throughout the initial assessment and management, the EMS provider should prioritize establishing and maintaining a calm and reassuring demeanor. Providing clear explanations and empathetic communication can significantly reduce patient anxiety and improve cooperation while awaiting the arrival of additional EMS resources or during transport.
Airway management is essential in the trauma patient. The provider must ensure a patent airway and be prepared to intervene with airway adjuncts such as oropharyngeal or nasopharyngeal airways, as indicated by the patient’s level of consciousness and gag reflex. Following airway assessment, the focus shifts to breathing. Oxygen administration should be initiated based on the patient’s respiratory status and oxygen saturation levels, utilizing high-flow and high-concentration oxygen delivery systems when indicated to address hypoxemia. If the patient exhibits inadequate respiratory effort or tidal volume, assisted ventilation with a bag-valve-mask (BVM) device or other appropriate ventilatory support should be promptly implemented to ensure adequate oxygenation and carbon dioxide removal.
Circulatory assessment and management are necessary in the trauma setting, as hemorrhage is a leading cause of preventable death. Any obvious uncontrolled external bleeding must be addressed immediately. Initial efforts should focus on direct pressure applied to the wound. If direct pressure is insufficient, the application of a tourniquet proximal to the bleeding site may be necessary for limb hemorrhage. Hemostatic agents, wound packing with specialized gauze, and skin clamps may also be utilized as adjunctive measures to control severe external bleeding, depending on the location and nature of the injury, resources available, as well as your training and authorization from your medical director.
Maintaining adequate perfusion also involves appropriate patient positioning. The optimal position will vary based on the patient’s age, injuries, and overall condition. For instance, the Trendelenburg position (head down) is generally no longer recommended for undifferentiated shock and may be contraindicated in certain situations. Regardless of the position, efforts to keep the patient warm are essential to prevent hypothermia, which can make clotting more difficult and worsen outcomes in trauma. Active warming measures, such as blankets and environmental control, should be implemented.
Given the time-sensitive nature of many traumatic injuries, transport to an appropriate medical facility should be facilitated at the earliest possible moment once critical life threats have been addressed and the patient is reasonably stabilized. While en route, ongoing assessment and management, including the treatment of any additional identified injuries, should continue. This comprehensive approach, from initial stabilization to definitive care, is crucial for optimizing outcomes in trauma patients.
Age-Related Variations in Shock
The presentation and management of shock in pediatric and geriatric populations present unique challenges for EMS providers. Understanding the physiological differences inherent in these age groups is paramount for accurate assessment and effective intervention. This section will delve into the specific considerations for recognizing and treating shock in children and older adults, emphasizing the deviations from typical adult presentations. Recognizing these nuances can significantly impact patient outcomes and underscores the need for age-appropriate assessment and treatment strategies.
Pediatrics
Shock in pediatric patients often stems from distinct etiologies compared to adults. Common causes include trauma, frequently due to accidental injury; fluid loss from vomiting, diarrhea, or dehydration; infection leading to septic shock; anaphylaxis triggered by allergens; congenital heart disease compromising circulatory function; and chest wall injury impairing respiration and cardiac output. Recognizing these potential causes in the pediatric context is crucial for guiding assessment and anticipating potential complications.
The presentation of shock in children manifests across multiple body systems. Cardiovascular signs may include tachycardia (although bradycardia can be a late and ominous sign), weak peripheral pulses, and delayed capillary refill. Skin signs often reveal pallor, mottling, and cool extremities. Central nervous system (CNS) changes can range from irritability and anxiety to lethargy and decreased responsiveness. Decreased fluid output, reflected in reduced urine production, is another key indicator. Vital sign interpretation in pediatrics requires age-specific norms, as what constitutes hypotension or tachycardia varies significantly with developmental stage.
Management of pediatric shock follows the general principles of shock resuscitation but with specific adaptations. Inline spinal stabilization should be implemented if there is suspicion of spinal injury. The airway should be assessed and maintained, with suction readily available to clear secretions. High-concentration oxygen should be administered as indicated to address hypoxemia. External bleeding must be controlled promptly. Positioning the patient supine with legs slightly elevated (Trendelenburg position is generally not recommended) can aid venous return. Maintaining body temperature is critical to prevent hypothermia, which can exacerbate shock. Rapid and safe transport to an appropriate medical facility is necessary for definitive care.
Geriatrics
Assessing shock in geriatric patients is complicated by age-related physiological changes that can mask or alter the typical signs and symptoms. Body system changes significantly affect the presentation of shock. CNS changes, such as altered mental status, may be pre-existing or subtle, making it difficult to attribute them solely to shock. Cardiovascular changes, including decreased cardiac reserve and arterial stiffness, can limit the body’s ability to compensate for hypoperfusion. Respiratory changes, such as decreased lung elasticity, can impair oxygenation. Skin changes, like decreased turgor, can make assessment of dehydration challenging. Renal and gastrointestinal (GI) changes can affect fluid balance and medication metabolism.
Vital sign changes in geriatric shock may be less pronounced or delayed. The CNS’s ability to trigger compensatory mechanisms may be blunted, and pre-existing conditions or medications can affect baseline vital signs. Hypoxia may be less readily apparent due to decreased respiratory reserve. Airway management in older adults requires careful consideration due to a decreased cough reflex, the potential for cervical arthritis limiting neck mobility, and the presence of loose dentures that can obstruct the airway. Breathing can be compromised by a higher resting respiratory rate, a lower tidal volume, and decreased elasticity and compliance of the chest wall, making them more susceptible to respiratory distress in the context of shock.
13.2 Resuscitation
Management of sudden cardiac or respiratory arrest, and further care during the immediate post-resuscitation period is core to EMS. As an EMR you may be the first trained person at the incident. You will be required to perform these skills quickly and correctly to support the best chance of survival for your patient.
Learning Objectives
- Anatomy and physiology review.
- Respiratory failure and arrest.
- Recognizing cardiac arrest.
- Interventions: CPR and AED.
- Consideration of special circumstances encountered in EMS.
- Identify the importance of effective chest compressions.
- Differentiate appropriate application of CPR and CCR.
- Identify reasons for cardiac arrest
Anatomy and Physiology Review
The Respiratory System
The respiratory system is necessary for life, serving as the interface between the external environment and the body’s internal location for gas exchange. The primary function of this system is to facilitate the intake of oxygen (O₂) from the atmosphere into the lungs, where it then diffuses across the alveolar-capillary membrane into the bloodstream. Simultaneously, carbon dioxide (CO₂), a metabolic waste product generated by cellular respiration, moves from the blood into the alveoli to be expelled from the body during exhalation. This continuous exchange of gases is essential for maintaining cellular function and overall homeostasis.
The Cardiovascular System
The cardiovascular system, comprising the heart and the vascular network, works in close coordination with the respiratory system to ensure the efficient transport of oxygen and nutrients throughout the body and the removal of metabolic wastes. The heart, a four-chambered muscular organ, acts as the central pump of this system. The right side of the heart receives deoxygenated blood from the body and pumps it to the lungs for oxygenation. The oxygenated blood then returns to the left side of the heart, which forcefully pumps it into the systemic circulation, delivering oxygen and vital nutrients to all tissues.
Systemic Circulation
As the oxygenated blood is ejected from the left ventricle, it enters the arterial system, a network of vessels that carries blood away from the heart towards the tissues. Conversely, the venous system, including veins, returns deoxygenated blood from the tissues back to the heart. The rhythmic contraction of the left ventricle generates a pressure wave that propagates through the arterial system, which can be palpated as a pulse at various locations where superficial arteries are accessible. Clinically significant pulse points include the carotid artery in the neck, the femoral artery in the groin, the radial artery in the wrist, and the brachial artery in the upper arm. Assessing these pulses provides critical information about the patient’s circulatory status.
Respiratory Failure and Respiratory Arrest
The ability to breathe and effectively exchange oxygen and carbon dioxide is essential to sustaining life. As an EMR, recognizing and responding rapidly to respiratory failure and arrest can be life-saving. These conditions are time-sensitive medical emergencies requiring prompt assessment and intervention to prevent cardiac arrest and death The support of airway and breathing is central to EMS interventions at all levels.
Respiratory Failure
Respiratory failure occurs when the respiratory system fails to provide adequate oxygenation of the blood or cannot remove carbon dioxide efficiently. This condition may develop slowly or suddenly, depending on the underlying cause. It is often a precursor to respiratory arrest if not treated quickly.
Causes of Respiratory Failure
Common causes include:
- Obstruction of the airway (e.g., foreign body, swelling from anaphylaxis, trauma).
- Respiratory diseases (e.g., asthma, chronic obstructive pulmonary disease [COPD], pneumonia).
- Neurological impairment (e.g., drug overdose, brain injury, spinal cord trauma).
- Chest trauma (e.g., flail chest, pneumothorax).
- Shock (e.g., sepsis, hypovolemia).
Signs and Symptoms
EMRs must remain alert for the following indicators of respiratory failure:
- Increased work of breathing (use of accessory muscles, tripod position).
- Abnormal respiratory rate (too fast or slow).
- Altered mental status (anxiety, confusion).
- Inability to speak in full sentences.
- Cyanosis.
- Diminished or abnormal breath sounds.
- Poor oxygen saturation (typically <90% on pulse oximetry).
EMR Interventions
Initial treatment focuses on supporting breathing and improving oxygenation:
- Allow to maintain a position of comfort if still alert.
- Administer oxygen via non-rebreather mask or nasal cannula depending on patient condition.
- Ensure airway patency using head-tilt/chin-lift or jaw-thrust maneuvers.
- Suction secretions if the airway is obstructed.
- Assist ventilations using a bag-valve mask (BVM) device if the patient is unable to breathe adequately on their own.
Activate advanced EMS response immediately.
Respiratory Arrest
Respiratory arrest is the complete cessation of breathing. It is a critical emergency that, if not treated immediately, will lead to cardiac arrest and death within minutes due to lack of oxygen to vital organs.
Causes of Respiratory Arrest
Many of the same factors that cause respiratory failure can progress to arrest.
Signs and Symptoms
When a patient is in respiratory arrest, EMRs may observe:
- Unresponsiveness.
- Cyanosis or pallor.
- Possible agonal gasps (ineffective, irregular breaths).
- No chest rise or breath sounds.
- Pulse may still be present initially but will deteriorate quickly.
EMR Interventions
Management of respiratory arrest must be immediate:
- Check for responsiveness and breathing.
- Open the airway using appropriate technique.
- Suction as needed.
- Evaluate for foreign body obstruction.
- Use airway adjuncts to maintain airway patency when indicated.
- Provide rescue breaths with a BVM connected to high-flow oxygen at 15 L/min (1 breath every 5-6 seconds in adults, every 3-5 seconds in children and infants).
- Reassess pulse every 2 minutes.
- If the patient becomes pulseless, begin CPR immediately and apply AED.
Summary
Understanding the difference between respiratory failure and arrest is crucial for effective emergency response. Early recognition of signs, coupled with timely and appropriate interventions, can prevent deterioration and improve patient outcomes. EMRs must maintain a high index of suspicion and act quickly using the tools and training within their scope of practice.
Cardiac Failure and Cardiac Arrest
When the heart cannot circulate blood with oxygen and nutrients throughout the body adequately or stops entirely, the result is a life-threatening emergency. As an EMR, understanding the difference between cardiac failure and cardiac arrest, along with their early signs and appropriate treatments, can make the difference between life and death.
Cardiac Failure
Cardiac failure, often referred to as congestive heart failure (CHF), is a condition where the heart is weakened and unable to pump blood efficiently. This leads to a backup of fluid in the lungs and other tissues. It may occur gradually or worsen suddenly, especially in patients with chronic heart disease.
Causes of Cardiac Failure
Cardiac failure can result from a variety of underlying conditions, including:
- Chronic hypertension (high blood pressure).
- Myocardial infarctioglon (heart attack).
- Valve disorders (e.g., mitral or aortic valve disease).
- Cardiomyopathy (disease of the heart muscle).
- Pulmonary hypertension.
- Kidney failure or fluid overload.
Signs and Symptoms
Key signs and symptoms of cardiac failure include:
- Shortness of breath, especially with walking or lying flat.
- Rapid or labored breathing (dyspnea).
- Fatigue and weakness.
- Swelling (edema), especially in the legs and ankles.
- Crackles or rales heard on lung auscultation.
- Rapid or irregular pulse.
- Cyanosis.
- Frothy or pink-tinged sputum (pulmonary edema).
EMR Interventions
While EMRs do not provide advanced cardiac care, they play a critical role in the early recognition and stabilization of patients with heart failure:
- Position the patient upright to ease breathing and reduce pulmonary congestion.
- Administer oxygen via non-rebreather mask or nasal cannula to maintain adequate oxygenation.
- Calm and reassure the patient to reduce anxiety and respiratory demand.
- Monitor vital signs and observe for worsening symptoms.
- Avoid physical exertion for the patient to prevent further cardiac strain.
Activate advanced EMS response for transport and advanced treatment.
Cardiac Arrest Management
More than 350,000 people per year suffer a cardiac arrest outside of a hospital every year in the United States. Cardiac arrest occurs when the heart stops beating correctly and blood stops flowing. Their only hope for survival is being found by someone quickly, and hopefully that person performing cardiopulmonary resuscitation, or CPR. The rate of this cardiac arrest survival in the United States remains low, overall less than 10%, despite advances in technology and medicine. A key factor is the initiation of bystander CPR. This doubles or even triples the rate of survival [**AHA]. As an EMR, you will be one of the earliest links in the chain of survival. You will provide high-quality CPR and defibrillation with an automatic external defibrillator (AED) when possible. Without this essential basic life support (BLS) treatment, the advanced life support (ALS) interventions and medications subsequently provided will not be effective. EMRs are required to be certified in CPR through a professional organization, such as the Red Cross or American Heart Association. The information provided here is no substitution for this healthcare provider level of training.
Signs of Cardiac Arrest
What does a cardiac arrest look like? Be very concerned for a cardiac arrest if someone:
- Suddenly passes out.
- Stops breathing or is only gasping (not breathing normally).
- Does not improve when you attempt to wake them by shouting their name or shaking their shoulders.
- Does not have a pulse on exam.
These are indications to activate the emergency response system if you are a bystander, and to start CPR.
View the following YouTube video to view an example of sudden cardiac arrest: Damar Hamlin Collapses After Hit vs Bengals
Causes of Cardiac Arrest
Cardiac arrest may be caused by:
- Heart attack.
- Abnormal heart rhythms.
- Congenital (from birth) abnormal heart or blood vessel development.
- Respiratory arrest,
- Drug overdose (e.g., opioids, sedatives).
- Medication side effects.
- Trauma.
- Drowning.
- Electrocution.
Disease of the heart itself is the most common cause of cardiac arrest in adults. Children often suffer from respiratory compromise and arrest before experiencing cardiac arrest. Unfortunately, cardiac arrest in children is just as deadly as in adults.
Basic Life Support Cardiopulmonary Resuscitation
When the heart stops, it loses 7-10% of its energy and ability to restart every minute. The goal of CPR is to prolong this time period by providing circulation to the heart and the brain.
An example of the effect of high-quality CPR and the chain of survival was a successful resuscitation with normal neurologic function happened in Minnesota in January 2011 when a 54-year-old man with no known heart disease, who had just finished his daily workout, stopped in a local store to pick up propane. He collapsed just outside the store. A resident initiated bystander CPR and a local first responder joined. They were quickly supported by other local first responders. CPR continued and six AED defibrillations were administered. This continued for over 30 minutes as no pulse was felt. The resuscitation was also moved into the nearby fire station due to the outside temperature. Upon arrival of the ALS helicopter crew, CPR was continued and the patient was moved onto their equipment. The presence of perfusion was detected with capnography, so the resuscitation was continued. During the next 45 minutes, multiple medications were administered as well as six additional defibrillations with intermittent return of pulses. Finally, a sustained rhythm and pulse were achieved. The patient was flown 20 minutes to a cardiac center for further interventions, including cardiac catheterization and balloon pump support. He woke up in the ICU days later with no memory of the event, but also no neurological impairment. He went home on day 10. A total of 96 minutes of manual CPR had been performed. This was believed to be the longest manual CPR resuscitation reported at the time. The quality of CPR and frequent exchanges between rescuers to avoid fatigue were noted as contributions to this patient’s survival. Since then, multiple longer out-of-hospital resuscitations have been reported, all utilizing mechanical CPR devices to supplement manual CPR.
What is High-Quality CPR and How Does it Work?
Note: This overview and explanation is not a substitute for a healthcare provider-level CPR course. These courses will train you in the correct technique and provide additional information.
Chest compressions use the chest as a closed compartment to force the movement of blood through arteries to deliver oxygen and nutrients to organs and tissues. The focus organs in CPR are the heart and brain. Both compression and decompression, or recoil, are important in CPR. Compression should be ⅓ the depth of the chest. Incomplete chest recoil, which often occurs when the rescuer becomes tired and leans on the chest, decreases the blood flow.
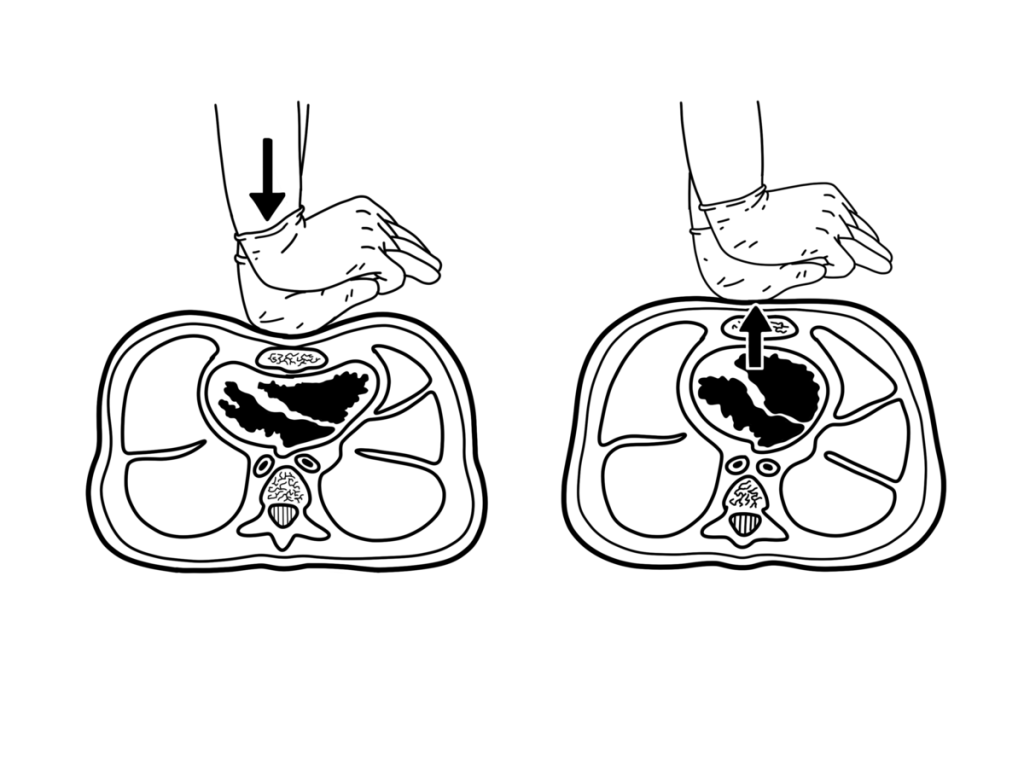
There is also essential timing of lung ventilation, as these breaths increase the lung size or volume and take up space in the chest, which can decrease the flow of blood. Controlling ventilations becomes easier and more effective when an advanced airway is able to be placed. When this is accomplished, continuous compressions are used. However, advanced airways are not associated with improved survival.*** This option must be balanced with the time and training required to perform it correctly. Cardiac arrest research has shown that the optimal rate of chest compression is 100-120 per minute. Use of a metronome device or program is optimal. Recognize that CPR only provides about ⅓ of the blood flow as a beating heart under the best circumstances, and you must work diligently to do this. Change compressors at least every 2 minutes, sooner as you progress through the resuscitation and are more quickly fatigued. Always be aware of who will be the next compressor. Manual compressions on a firm flat surface are optimal. As soon as rescuers are fatigued or must move the patient, a mechanical device is preferred. Compression interruptions are ideally kept to less than 10 seconds per the American Heart Association guidelines; and under 30 seconds if moving the patient. This is difficult. Every time you stop, it takes multiple compressions to restart blood flow.
Mechanical chest compression devices are becoming more available in EMS; however, they remain expensive and require additional training.
View the following YouTube videos to see some examples in use:
Compressions Without Ventilations
There are adaptations of CPR that do not use ventilations. The first is bystander hands-only CPR. It has been recognized that people are hesitant to perform mouth-to-mouth ventilations, especially if the person is not a family member. Compression-only CPR is now the preferred method when bystanders call 911 and report that someone is not responsive and not breathing normally. Trained 911 communicators can rapidly provide chest compression instructions and guidance. This has increased the participation of bystanders in performing CPR and you can expect to see this when you arrive as an EMR.
The EMS technique of continuous compressions-first CPR, also known as cardio cerebral resuscitation or CCR, has been known for years. The research to support this is based on the level of oxygen in the blood at the time of collapse. This supply is adequate for the first 6-8 minutes of compressions and is supplemented by passive oxygenation by placing a high-flow oxygen mask on the patient. There are important differences when the cause of collapse is respiratory in nature, such as drowning or overdose, or in children. In these cases, standard CPR should be performed. The difference between CCR and CPR has decreased since CPR techniques moved chest compressions before ventilations.
Incorporating the Automatic External Defibrillator (AED)
It is apparent that chest compressions are the first essential step in cardiac arrest survival. The next one is the automatic external defibrillator. As soon as this device arrives it should be applied and activated. AEDs have voice prompts to assist both trained rescuers and civilians, as well as diagrams on the pads to assist with correct placement. In your community, one of the best outreach programs in which you can participate is citizen CPR training and public access defibrillator availability. The highest rates of survival in a shockable rhythm are when bystander CPR is initiated immediately and bystander AED use is applied within 3-5 minutes. *** This is a challenging goal to achieve.

A common statement is that the AED “jump-starts” the heart. You should recognize that It actually jump-stops, or reboots, the heart by turning off the abnormal signals generated by damaged cardiac tissue or other overactive areas. Once this happens, the goal is to have a normal cardiac signal take over. If a shockable rhythm is present and treated, the chances of resuscitation are higher.***
Age-Specific CPR Considerations
Most cardiopulmonary arrest events involve adult patients, and this is the typical training scenario. Recognize that you must be able to treat all persons of all ages. There are differences in assessment of a pulse in infants, and the ratio of compressions to breaths in children and infants when two rescuers are present. The size of the mask and the ventilatory bag must be considered. Infants and early-school-age children benefit from placing a towel roll under their shoulders to help align their airway. The smaller AED pads are used when available. This can be confusing, especially when under stress. Remember that any CPR performed improves the survival rate, so just get it started. When you recognize the need to change your technique, communicate with your partner and do so. Also be ready to accept coaching and suggestions from your partner when they realize a change is required.
View the following YouTube video showing how to use an AED: How to Use an AED on All Ages
Special Circumstances Pertaining to CPR
Hypothermia
More details and the pathophysiology of hypothermia will be covered elsewhere. Mild hypothermia (core temperature below 95°F or 35°C) is very common in emergency illness and injury situations. That will not impact CPR performance. Moderate (below 90°F or 32°C) to severe (below 82.5°F or 28°C) hypothermia can affect the heart, causing very slow or unstable rhythms. When the heart is too cold, below 86°F or 30°C, it does not respond to standard interventions. Rewarming is the primary treatment.
Most of the time you will not know the patient’s actual temperature. If someone is unresponsive, not shivering, and feels cold when you place the back of your ungloved hand (just peel back your glove) against the skin of their chest, presume that they are significantly hypothermic.
The first difference for an adult hypothermic patient is to assess for a pulse for up to 1 minute before starting chest compressions. Hypothermic patients may have a very slow heart beat, but if present your focus should be on airway, breathing and rewarming. If you cannot detect a pulse, begin chest compressions.*** Note that essentially standard CPR assessment and treatment is performed for children and infants if hypothermia is suspected.
Rewarming begins with removing the victim from the cold environment. Next remove any wet or cold clothing and apply blankets. If available, hot packs should be placed at pulse points.
The next consideration is continuing CPR longer than typically considered effective as moderate hypothermia may be neuro-protective. This is the basis of Targeted Temperature Management in Advanced Cardiac Life Support. Depending on the circumstances, always remember that your safety comes first. Scene safety and situational awareness are primary in uncontrolled, remote or extreme environments.
Hyperthermia
As opposed to hypothermia, hyperthermia is always detrimental. Again, it is unlikely that you will know the actual temperature of your patient. Hyperthermia-associated cardiac arrest is often preceded by other signs or symptoms, such as infection, exertion in a hot environment, a change in routine with a hot environment, or stimulant ingestion. Dangerous hyperthermia is typically a core body temperature above 104°F (40°C), but actually more in the 106-107°F (41°C) range. This is outside of your body’s ability to regulate cardiovascular, endocrine and protein metabolism.
Cardiac arrest with severe hyperthermia is very difficult to treat, as it is challenging to perform CPR in an ice bath. Cold packs may be applied at pulse points, but this is much less effective. Another circumstance where prevention is much more beneficial than treatment.
Visit Outdoor Auction’s website to learn more about heat loss, injury, and emergency response: Outdoor Action Guide to Hypothermia And Cold Weather Injuries
Drowning
Unless you are a trained lifeguard or water rescue provider, you will not be performing CPR in the water. Your interventions will start when the victim is brought to land or another solid surface. There are various stages of submersion and drowning. The worse the person’s mental status coming out of the water, the worse their prognosis for survival. CPR is provided as usual. Do not attempt to turn the person over to “drain” their lungs of water. This is not effective and delays resuscitation.
CDC Fast Facts
- Every year in the United States there are an estimated:
- 4,000 fatal unintentional drownings – that is an average of 11 drowning deaths per day.
- 8,000 nonfatal drownings – that is an average of 22 nonfatal drownings per day.
- In the United States:
- More children ages 1–4 die from drowning than any other cause of death.
- For children ages 5–14, drowning is the second leading cause of unintentional injury death after motor vehicle crashes.
Of note, routine stabilization of the cervical spine in the absence of circumstances that suggest a spinal injury is not recommended.
Lightning Strike and Electrocution
These circumstances are challenging and often involve multiple victims. Unlike other environmental situations, these patients have a good survival rate, as their cardiopulmonary arrest is temporary. There is a complex cascade of events after the electrical strike, causing unconsciousness and possible respiratory muscle paralysis. The heart continues to beat until it is depleted of oxygen. Standard CPR can save these victims.
Industrial voltage exposure, versus household current, is more damaging. In both electrocution and lightning strike, secondary trauma and burns indicate worse survival.
Pregnancy
Cardiac arrest during pregnancy involves two patients. There are multiple circumstances that lead up to this event, but the survival of the mother supports the survival of the fetus. That is your focus. The change in technique for CPR in a pregnant patient is avoiding supine positioning if the pregnancy is visible on abdominal examination, usually after 20 weeks of gestation. If you can see the woman is pregnant, you must move the enlarged uterus off of the central blood vessels to allow blood flow during CPR. This is accomplished by either having a partner push the uterus to the left or placing the patient on a backboard and tipping it 30 degrees to the left-side down. If you cannot remember to tilt your patient to the right or left, just remember to tilt her either way. Avoid her laying flat.
View the following YouTube video for an overview of moving the enlarged uterus, or left uterine displacement: CPR in Pregnant Women
Trauma
Cardiac arrest in trauma is usually fatal. The distinction is a minor trauma mechanism of injury, like a car rolling into a shallow ditch. This indicates a medical cause for the crash and the need for medical interventions.
The primary cause for cardiac arrest in a traumatic MOI is hemorrhage. This is not amenable or responsive to standard CPR interventions. When performing CPR on a trauma victim, look for medical causes. If these are not apparent, your interventions are unlikely to improve the outcome. The fatal injury has already been done.
Do Not Resuscitate Orders
A person may have previously decided to forgo invasive or heroic efforts in the event that their heart stops. This often has to do with their degree of illness or previous heart damage. In these cases you may find a DNR bracelet or tag, or be presented with paperwork.
In states such as Wisconsin, there is a standard DNR bracelet that acts as a standing order for EMS to limit resuscitation efforts in cardiac arrest. Visit the Wisconsin Department of Health Services webpage to see examples of plastic and metal bracelets:
Encounters with other forms of directives, such as hospital bracelets, advanced directives, living wills, or physician orders for life sustaining treatment (POLST) require specific training and are managed differently in each system. Your agency will inform you on these procedures.
When you are called to the scene of a person with a DNR order, you might wonder why. Often the family or caregivers are not prepared for this event, even if it is expected. They may simply be looking for confirmation that the person has died. They may be in denial of the event. More will be discussed in the next section on Termination of Resuscitation. However, always bear in mind that a DNR order only applies to resuscitation. A patient with a DNR order still receives standard EMS treatment if ill or injured.
Termination of Resuscitation
Patients suffer terminal illness, injuries and events while in EMS care. There are some circumstances that no amount of medical care will reverse. In these situations, recognizing the futility of further interventions allows you to inform family or caregivers, and then provide support for them.
Depending on your local treatment guidelines, there are some medically accepted signs of death that indicate you are not required to initiate resuscitation, or may cease when they are discovered. The 2015 American Heart Association (AHA) guidelines recommend that EMS providers do not initiate resuscitation of any patient in the following scenarios:
- Situations where attempts to perform CPR would place the rescuer at risk of serious injury or mortal peril.
- Overt clinical signs of irreversible death (e.g., rigor mortis, dependent lividity, decapitation, transection, decomposition).
- A valid advanced directive, a Physician Orders for Life-Sustaining Treatment (POLST) form indicating that resuscitation is not desired, or a valid Do Not Attempt Resuscitation (DNAR) order.
The National Association of EMS Physicians has long supported the field termination of resuscitation when futility is recognized. This is more challenging when in a rural area with longer ambulance and ALS response and transport times. Research supports decisions to stop resuscitation under certain circumstances, such as:
- The arrest was not witnessed by an EMS provider.
- There is no shockable rhythm identified by an automated external defibrillator (AED) or other electronic monitor.
- There is no return of spontaneous circulation prior to EMS transport.
The time associated with termination indicators continues to be researched, but is often limited to 20-30 minutes. This is defined by local treatment guidelines. ALS providers have additional equipment, resources and training in making this determination. When available, this decision is often left to their judgment.
Transitioning the family, caregivers or bystanders to the termination of resuscitation can be a difficult situation. EMS training and education on this has been brief or nonexistent for decades. In recognition of this deficit, some EMS-focused support and education has been developed. An example of a good resource is:
View the following YouTube video for an overview of death notifications by EMRs: Death Notifications by EMS Providers
If you think this is not an important topic, it is:
The Association of Death Notification and Related Training with Burnout among Emergency Medical Services Professionals
Summary
As an emergency medical responder, you need to be able to immediately recognize and start treatment in the event of sudden collapse with cardiopulmonary arrest. You must be certified in CPR for healthcare providers and practice these skills regularly to provide high quality care. You are a major link in the out-of-hospital cardiac arrest chain of survival.

As emergency personnel, you may encounter resuscitation situations that are challenging or unusual. You must be familiar with your local protocols and resources to guide you in these decisions.
Glossary
AED automated external defibrillator
CCR cardiocerebral resuscitation
CPR cardiopulmonary resuscitation
ROSC return of spontaneous circulation
Cardiac arrest the heart stops beating normally and there is no pulse
Aerobic – with oxygen
Ischemic – lack of oxygen
Agonal respirations ineffective, irregular breaths
Bradypnea – slow breathing
Hypoxemia – low oxygen in the body
Tachypnea – fast breathing
Hypofusion – low perfusion
References
American Academy of Pediatrics. (2021). Pediatric education for prehospital professionals (PEPP): Course manual (4th ed.). Jones & Bartlett Learning.
American College of Surgeons. (2018). ATLS: Advanced trauma life support student manual (10th ed.).
American Heart Association. (2010). Part 3: Adult basic and advanced life support. https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines/adult-basic-and-advanced-life-support#10.1
American Heart Association. (2020). BLS for healthcare providers.
American Heart Association. (2020a). Basic life support provider manual.
American Heart Association. (2023). Causes of cardiac arrest. https://www.heart.org/en/health-topics/cardiac-arrest/causes-of-cardiac-arrest
American Heart Association CPR & First Aid Emergency Cardiovascular Care. (n.d.). Cardiac emergency response plan (CERP). https://cpr.heart.org/en/training-programs/cardiac-emergency-response-plan-cerp
Campos, A., Ernest, E. V., Cash, R. E., Rivard, M. K., Panchal, A. R., Clemency, B. M., Swor, R. A., & Crowe, R. P. (2021). The association of death notification and related training with burnout among emergency medical services professionals. Prehospital Emergency Care, 25(4), 539–548. https://doi.org/10.1080/10903127.2020.1785599
Carney, N., Cheney, T., Totten, A. M., Jungbauer, R., Neth, M. R., Weeks, C., Davis-O’Reilly, C., Fu, R., Yu, Y., Chou, R., & Daya, M. (2021). Prehospital airway management. Agency for Healthcare Research and Quality. https://effectivehealthcare.ahrq.gov/products/prehospital-airway-management/research
Centers for Disease Control and Prevention. (2024). Chronic respiratory disease data and statistics. https://www.cdc.gov/nchs/fastats/copd.htm
Centers for Disease Control and Prevention. (2024a). Heart disease facts. https://www.cdc.gov/heart-disease/data-research/facts-stats/index.html
Centers for Disease Control and Prevention. (2024b). Drowning facts. https://www.cdc.gov/drowning/data-research/facts/index.html
Ewy G. A. (2005). Cardiocerebral resuscitation: The new cardiopulmonary resuscitation. Circulation, 111(16), 2134–2142. https://doi.org/10.1161/01.CIR.0000162503.57657.FA
Franciosi, S., Abrams, D. J., Ingles, J., & Sanatani, S. (2022). Sudden cardiac arrest in the paediatric population. CJC Pediatric and Congenital Heart Disease, 1(2), 45–59. https://doi.org/10.1016/j.cjcpc.2022.02.001
Kashef, M. A., & Lotfi, A. S. (2021). Evidence-based approach to out-of-hospital cardiac arrest. Current Treatment Options in Cardiovascular Medicine, 23(6), 43. https://doi.org/10.1007/s11936-021-00924-3
Mancini, M. E., Diekema, D. S., Hoadley, T. A., Kadlec, K. D., Leveille, M. H., McGowan, J. E., Munkwitz, M. M., Panchal, A. R., Sayre, M. R., & Sinz, E. H. (2015). Part 3: Ethical issues: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation, 132(18 Suppl 2), S383–S396. https://doi.org/10.1161/CIR.0000000000000254
Martini, F. H., Nath, J. L., & Bartholomew, E. F. (2018). Fundamentals of anatomy & physiology (11th ed.). Pearson.
Marx, J. A., Hockberger, R. S., Walls, R. M., Rosen, P., Gausche-Hill, M., & Harris, J. L. (Eds.). (2022). Rosen’s emergency medicine: Concepts and clinical practice (10th ed.). Elsevier.
Mohamed B. A. (2022). Airway management during cardiopulmonary resuscitation. Current Anesthesiology Reports, 12(3), 363–372. https://doi.org/10.1007/s40140-022-00527-z
National Association of EMS Physicians. (2011). Termination of resuscitation in nontraumatic cardiopulmonary arrest. Prehospital Emergency Care, 15(4), 542. https://doi.org/10.3109/10903127.2011.598621
National Highway Traffic Safety Administration. (2009). National emergency medical services education standards [PDF]. EMS.gov. https://boards.bsd.dli.mt.gov/_docs/med/ecp/generic-guide.pdf
National Registry of Emergency Medical Technicians. (2025). The new EMR and EMT certification examinations. NREMT.org. https://www.nremt.org/Pages/Examinations/EMR-and-EMT-Certification-Examinations
National Registry of Emergency Medical Technicians. (2016). Emergency medical technician psychomotor examination users guide [PDF]. NREMT.org. https://content.nremt.org/static/documents/2016%20EMT%20User’s%20Guide%20v1.1.pdf
O’Keefe, K. P. (2023). Electrical injuries and lightning strikes: Evaluation and management. UpToDate. https://www.uptodate.com/contents/electrical-injuries-and-lightning-strikes-evaluation-and-management/print
Porter, R. S., Kaplan, J. L., & Homeier, B. P. (Eds.). (2023). Merck manual professional version. Merck Sharp & Dohme Corp.
Tintinalli, J. E., Stapczynski, J. S., Ma, O. J., Yealy, D. M., Meckler, G. D., Cline, D. M., & Thomas, S. H. (Eds.). (2020). Tintinalli’s emergency medicine: A comprehensive study guide (9th ed.). McGraw-Hill Education.
U.S. National Library of Medicine. (n.d.). Anaphylaxis. MedlinePlus [Internet]. https://medlineplus.gov/anaphylaxis.html
White, R. D., Goodman, B. W., & Svoboda, M. A. (2011). Neurologic recovery following prolonged out-of-hospital cardiac arrest with resuscitation guided by continuous capnography. Mayo Clinic proceedings, 86(6), 544–548. https://doi.org/10.4065/mcp.2011.0229
Wisconsin Department of Health Services. (2023). EMS: Do not resuscitate information. https://www.dhs.wisconsin.gov/ems/dnr.htm
Images:
Figure 13.1: ”2003_Dual_System_of_Human_Circulation” by OpenStax College is licensed under CC BY 3.0
Figure 13.2: “CPR-heart-compression” by Baedr-9439 is licensed under CC0, Public Domain
Figure 13.3: “AED_-_Automated_external_defibrillator_in_compartment_with_sign_above” by Infrogmation is licensed under CC BY-SA 4.0
Figure 13.4: “Chain_of_Survival” by unknown author is licensed under CC0, Public Domain
Videos:
The Paramedic Coach. (2021, April 22). Types of Shock Explained Simply | NREMT EMT Review [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=1KAPfQQweM4
Neural Academy. (2023, April 25). The 4 stages of shock [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=M9BQdJAUP5U
WCTCFire&EMS. (2012, December 25). EMT 4-1: Overview of shock [Video]. YouTube. CC BY 4.0. https://www.youtube.com/watch?v=YWRRITkjm48
Swift Highlights. (2023, January 3). Damar Hamlin collapses after hit vs Bengals [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=r1Z9Vd53yhI&t=24s
zollmedical. (2016, January 18). AutoPulse basic deployment (4:02) [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=UmMsikaEH9A
MFI Medical. (2018, September 21). Physio-control Lucas 3 chest compression system – prehospital use [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=bIE-sj45DlY
Michigan Instruments. (2012, October 8). Life-Stat® a proven life saver [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=K2HEfezFqZA
Children’s Hospital of Philadelphia. (2023, January 6). How to use an AED on all ages [Video]. All rights reserved. https://www.youtube.com/watch?v=zHe9TEn5sno
EM Note. (2024, September 11). CPR in pregnant women [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=S_84fl1SEUI
Gary Heigel. (2021, April 6). Death notifications by EMS providers [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=Ak_f9MVQw6Y

