Chapter 11: Medicine Part 02
Jamie Howell
11.1 Introduction
(needs to be written to keep consistency with other chapters)
Learning Objectives
- Genitourinary/Renal 6.11
- Hematology 6.12
- Immunology 6.4
- Infectious Diseases 6.5
- Neurology 6.2
11.2 Altered Mental Status and Neurological Emergencies
Causes of Altered Mental Status
Altered mental status can be caused by a variety of factors, often reflecting underlying neurological or systemic issues. Some of the key causes include:
- Fever
- Infection
- Poisoning or overdose, including substance abuse or misuse
- Blood sugar or endocrine emergencies
- Head injury or trauma
- Inadequate oxygenation or ventilation
- Conditions leading to decreased blood flow or oxygen to the brain
- Cardiac emergencies
- Stroke
- Shock
- Behavioral health conditions
- Metabolic or nutritional imbalances
- Neurological conditions (e.g., brain injuries, infections, or tumors)
Critical Facts
Altered mental status refers to any significant change in a person’s usual level of consciousness or cognitive function. These changes may present as confusion, drowsiness, disorientation, or complete loss of consciousness.
Altered mental status is a common manifestation of a wide range of medical emergencies, often requiring immediate intervention and transport to medical facilities for further evaluation and care.
Signs and Symptoms of Altered Mental Status
Altered mental status can vary widely depending on the underlying cause. Patients may experience sudden or gradual changes in their ability to think clearly, interact with others, or maintain awareness of their surroundings. Common signs and symptoms include:
- Confusion or disorientation
- Drowsiness or excessive sleepiness
- Difficulty speaking or understanding language
- Changes in behavior, such as agitation or combativeness
- Memory loss or inability to recall recent events
- Decreased responsiveness
- Loss of consciousness
Providing Care for Altered Mental Status
When responding to altered mental status, your priority is to identify the underlying cause and provide supportive care. Start by performing a primary assessment, ensuring the airway is clear, and checking for adequate breathing and circulation.
- Airway and Breathing: Always ensure the patient’s airway is open and that they are breathing adequately. If the patient is unconscious, position them appropriately, either in the recovery position (if there are no head, neck, or spinal injuries) or in a supine position if you suspect trauma.
- Ongoing Assessment: Keep performing secondary assessments to check vital signs, such as heart rate, blood pressure, and respiratory rate. Assess for any visible injuries or signs of head trauma. Document the patient’s condition and any relevant history or events leading up to the altered mental status.
- Monitor for Decline: Altered mental status can deteriorate rapidly. If the patient’s condition worsens, be prepared to provide advanced interventions like CPR, oxygen, or suctioning if necessary.
- Gather Information: Attempt to obtain information from the patient, bystanders, or family members to understand the possible cause of the altered mental status. This information is crucial, as it can guide further treatment decisions. For example, signs of recent head trauma or fever may point to neurological issues, while a history of substance abuse may suggest an overdose.
Syncope (Fainting)
Sometimes, a temporary decrease in blood flow to the brain causes a brief altered mental status, known as syncope or fainting. This condition is often triggered by factors such as:
- Standing up too quickly
- Pain or emotional shock
- Low blood pressure or dehydration
- Cardiac irregularities
Signs of presyncope (the feeling of impending fainting) include:
- Dizziness or lightheadedness
- Nausea
- Blurred vision
- Sweating or clamminess
Patients who faint typically recover quickly after lying down and restoring normal blood flow to the brain. However, the underlying cause of the syncope should always be investigated to ensure there are no serious health conditions contributing to the episode.
Care for Syncope
- Place the patient in a lying down position to help restore normal blood flow to the brain.
- Monitor vital signs and level of consciousness.
- If the patient regains consciousness, allow them to rest before standing up again. Do not allow them to walk immediately, as fainting may recur.
In cases where syncope is associated with head injury, cardiac symptoms, or a known medical condition (like diabetes), seek more advanced medical care.
Stroke (Cerebrovascular Accident)
A stroke is a critical neurological emergency that can lead to altered mental status. It occurs when there is a disruption of blood flow to part of the brain, which can cause irreversible damage to brain tissue. Strokes can be caused by:
- Blockage of blood vessels (ischemic stroke)
- Ruptured blood vessels (hemorrhagic stroke)
Signs of a stroke include:
- Sudden weakness or numbness, particularly on one side of the body
- Sudden confusion, trouble speaking, or understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden difficulty walking, dizziness, or loss of balance
Care for a Suspected Stroke
If a stroke is suspected, immediate medical attention is critical. Call emergency services immediately. You can use the FAST acronym to quickly assess:
- Face: Ask the patient to smile. Is one side drooping?
- Arms: Ask the patient to raise both arms. Does one arm drift downward?
- Speech: Ask the patient to repeat a simple sentence. Is their speech slurred or strange?
- Time: If any of these symptoms are present, get help immediately.
Do not attempt to give the patient anything to eat or drink, as this can complicate treatment. Keep the patient in a comfortable position and monitor vital signs until help arrives.
11.3 Neurological Conditions Causing Altered Mental Status
Several neurological conditions can contribute to altered mental status, including:
- Traumatic Brain Injury (TBI): Caused by a blow or jolt to the head, leading to swelling or bleeding in the brain.
- Brain Infections (e.g., Meningitis, Encephalitis): Infections of the brain or its coverings can cause confusion, fever, and other neurological symptoms.
- Brain Tumors: Growths in the brain may disrupt normal brain function and lead to changes in mental status, ranging from confusion to loss of consciousness.
Traumatic Brain Injury (TBI)
When a person sustains a head injury, it’s important to assess for signs of a TBI. Symptoms may include:
- Loss of consciousness
- Amnesia or memory loss
- Confusion
- Severe headache
If a TBI is suspected, keep the patient still and avoid moving their neck or spine, especially if there is a concern for spinal injury.
Care for Neurological Emergencies
For any neurological emergency that causes altered mental status, the following priorities should be observed:
- Protect the Airway: Ensure the patient’s airway is open. If they are unconscious, place them in the recovery position or supine position if spinal injury is suspected.
- Monitor Vital Signs: Continue to assess the patient’s breathing, pulse, and level of consciousness. Watch for signs of rapid deterioration.
- Get Information: Collect relevant history from the patient or bystanders to determine the cause of the altered mental status, including any potential history of head injury, medical conditions, or substance use.
- Activate EMS: In many cases, neurological emergencies require urgent care and transportation to a medical facility for advanced diagnostic evaluation and treatment.
Recognizing and Responding to Seizures
Types of Seizures
- Generalized Seizures:
- Involve both brain hemispheres.
- Tonic-clonic phases: Muscle rigidity followed by rhythmic contractions.
- Often lasts 1–3 minutes.
- Partial Seizures:
- Limited to one brain area.
- Simple: Awareness retained, localized movements or sensations.
- Complex: Awareness impaired, repetitive movements, or confusion.
- Absence Seizures:
- Brief, sudden loss of awareness.
- Common in children; may resemble daydreaming.
- Febrile Seizures:
- Triggered by high fevers in children under five.
Signs and Symptoms of Seizures:
- Sudden collapse
- Jerking movements
- Temporary loss of consciousness
- Post-ictal phase: Confusion or fatigue after a seizure
Providing Care for Seizures:
- During the Seizure:
- Protect the patient from injury by moving objects away.
- Do not restrain the patient or place anything in their mouth.
- If safe, position the patient on their side to allow fluids to drain.
- After the Seizure:
- Monitor breathing and check for injuries.
- Comfort and reassure the patient.
- Avoid offering food or drink until they are fully alert.
- When to Call Advanced Medical Personnel:
- First-time seizure.
- Seizure lasts longer than 5 minutes.
- Multiple seizures without regaining consciousness (status epilepticus).
- Patient is pregnant, diabetic, or injured.
Pediatric Considerations
Children with altered mental status may show changes in behavior or responsiveness. Common causes include hypoxemia, infections, or febrile seizures. Address breathing emergencies and other injuries promptly, and ensure advanced care when needed.
Case Scenario: A Seizure in a Teenager
The Incident:
A 14-year-old boy, Ethan, is at his school’s basketball game when he suddenly collapses. His body stiffens, and rhythmic jerking movements begin. The crowd panics, and a bystander calls 911.
Discuss the appropriate management techniques, picking out appropriate and inappropriate actions:
- Potential Response:
The EMS team arrives promptly, they start moving nearby objects and positioning Ethan on his side. They monitor his airway without placing anything in his mouth and observe the seizure’s duration, which lasts about two minutes. After the seizure, they comfort Ethan, assess for injuries, and reassure him as he regains awareness. The responders gather medical history from bystanders, learning Ethan has epilepsy. EMS transports him to the hospital for evaluation. - Potential Response:
The responders panic upon arrival. One attempts to hold Ethan down during the seizure. Another places a wallet in his mouth. They fail to document the seizure’s duration or assess for injuries. Post-seizure, they give Ethan water while he is still disoriented. They do not obtain crucial medical history from the bystanders and transport Ethan to the hospital for evaluation.
Discussion Points:
- Why was the first response effective?
- What risks did the second response create?
- How could errors in the second scenario have been avoided?
Conclusion
Recognizing and responding appropriately to seizures can prevent further complications and ensure patient safety. The case study demonstrates the importance of proper training and highlights areas for improvement in emergency responses. By analyzing real-life scenarios, students can better prepare for neurological emergencies in their practice.
When to Call for More Advanced Medical Help
Altered mental status due to neurological issues often requires advanced medical care. Call for help if:
- The patient’s condition worsens or does not improve.
- You are unsure of the cause of the altered mental status.
- The patient is unconscious or has a diminished level of consciousness.
- The patient experiences a sudden, severe headache or signs of a stroke.
- The patient has a history of neurological conditions or trauma.
Neurological emergencies, especially those related to brain function, require immediate medical evaluation. Always err on the side of caution and seek professional help as soon as possible.
11.4 Renal and Genitourinary Emergencies
The genitourinary system, which includes the urinary system, plays a critical role in filtering and removing waste products from the body, maintaining fluid and electrolyte balance, and regulating blood pressure. Emergencies in this system can range from urinary tract infections (UTIs) to complications in patients undergoing dialysis. Understanding the anatomy and function of this system is essential for recognizing and managing these conditions.
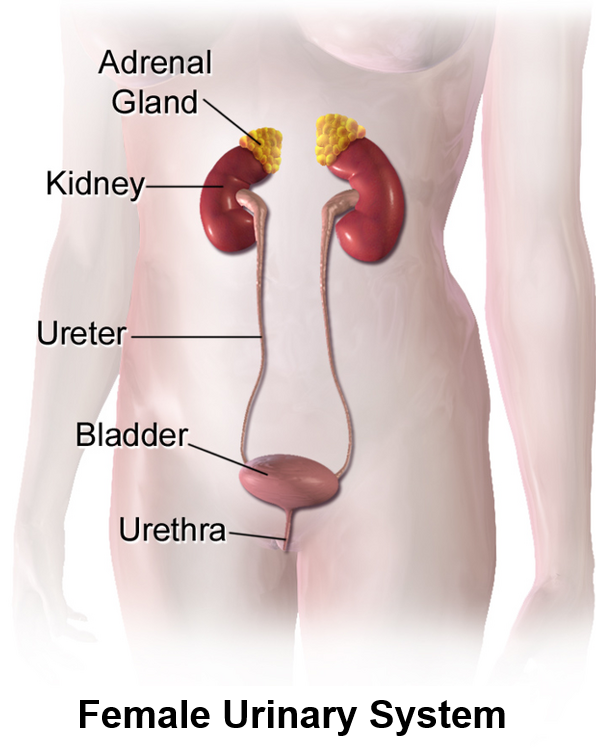
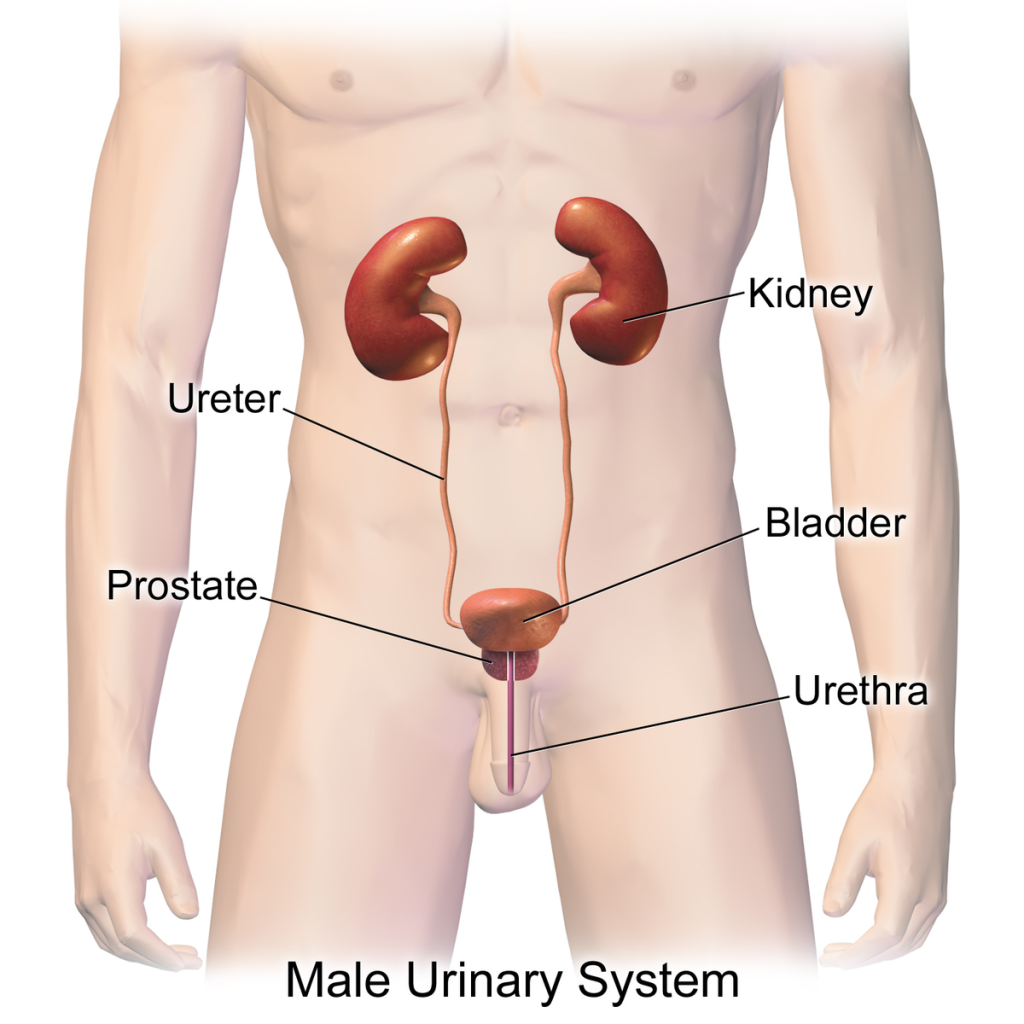
The urinary system is composed of four primary components:
- Kidneys: These bean-shaped organs are located in the lumbar region of the body, just below the rib cage. They filter blood to remove waste products and produce urine.
- Ureters: Narrow tubes that transport urine from the kidneys to the bladder.
- Bladder: A muscular sac that stores urine until it is ready to be expelled.
- Urethra: A small tube that carries urine from the bladder to the outside of the body.
This system not only eliminates waste but also plays a vital role in maintaining the body’s pH balance and regulating fluid levels.
Common Genitourinary Emergencies
Urinary Tract Infections (UTIs)
Definition and Causes:
UTIs occur when bacteria, commonly Escherichia coli, enter the urinary tract. They are more prevalent in women due to the shorter urethra but can affect anyone, including men, children, and the elderly.
Signs and Symptoms:
- Burning sensation during urination
- Frequent urge to urinate with little output
- Cloudy or foul-smelling urine
- Lower abdominal pain or discomfort
- Fever and chills in more severe cases
Elderly Considerations:
In older adults, UTIs can lead to urosepsis, a life-threatening condition where the infection spreads to the bloodstream. Symptoms may be vague and include confusion, lethargy, or sudden changes in behavior.
Patient Example:
Mrs. Thompson, an 82-year-old woman, is brought to the emergency department by her daughter, who noticed sudden confusion and weakness. On assessment, Mrs. Thompson has a fever and cloudy urine. After a urinalysis confirms a UTI, she is started on antibiotics and monitored for signs of sepsis.
Acute Kidney Injury (AKI) and Chronic Kidney Disease (CKD)
Acute Kidney Injury (AKI): A sudden decline in kidney function due to conditions like dehydration, infections, or medication toxicity. Symptoms include reduced urine output, swelling, and confusion.
Chronic Kidney Disease (CKD): A gradual loss of kidney function over time, often caused by diabetes or hypertension. Long-term complications include anemia, bone disease, and cardiovascular problems.
Emergency Situations:
- Hyperkalemia (High Potassium Levels): Can lead to life-threatening arrhythmias.
- Fluid Overload: Causes shortness of breath, hypertension, and edema.
- Uremia: Accumulation of waste in the blood, leading to confusion and nausea.
Dialysis and its Complications
Dialysis is a life-saving treatment for patients with kidney failure. It artificially filters waste and excess fluids from the blood. There are two primary types of dialysis:
- Hemodialysis: Blood is filtered using a machine through a vascular access point, such as an arteriovenous (AV) fistula.
- Peritoneal Dialysis: A dialysis solution is introduced into the peritoneal cavity through a catheter and later drained.
Visit the following webpages and YouTube video for more information:
National Institute of Diabetes and Digestive and Kidney Disease: Hemodialysis
National Institute of Diabetes and Digestive and Kidney Disease: Peritoneal Dialysis
Common Complications:
- Hypotension: Low blood pressure during or after hemodialysis.
- Disequilibrium Syndrome: Neurological symptoms caused by rapid changes in blood chemistry.
- Infections: At the dialysis site or throughout the body.
- Fluid Imbalances: Hypervolemia (fluid overload) or hypovolemia (fluid deficit).
Patient Example:
Mr. Patel, a 64-year-old man with end-stage renal disease, arrives at the clinic for his routine hemodialysis. During the session, he becomes lightheaded and hypotensive. Staff quickly recline him, administer fluids, and monitor his vitals, stabilizing his condition.
11.5 Hematology: Anticoagulants and Bleeding Disorders
Bleeding Disorders
Bleeding disorders occur when the blood does not clot properly, increasing the risk of excessive bleeding. Common conditions include:
- Hemophilia: A genetic disorder where the blood lacks clotting factors.
- Von Willebrand Disease: A condition caused by a deficiency of von Willebrand factor, a protein essential for blood clotting.
Patients with these disorders may present with:
- Uncontrolled bleeding after minor injuries
- Easy bruising
- Joint-swelling caused by internal bleeding
Anticoagulant Therapy
Patients on anticoagulants such as warfarin, heparin, or newer agents like rivaroxaban or apixaban are at heightened risk of bleeding. These medications are often prescribed for conditions such as:
- Atrial fibrillation
- Deep vein thrombosis (DVT)
- Pulmonary embolism
Special Considerations:
- Minor injuries may lead to significant bleeding.
- Patients with head injuries are at increased risk for rapid deterioration due to intracranial bleeding.
- Common signs include headache, confusion, or neurological changes.
Patient Example:
Mr. Taylor, a 68-year-old man on warfarin for atrial fibrillation, fell while walking his dog and struck his head. Initially, he reported only mild pain but later became confused. When the EMR team arrived, they recognized the potential for intracranial bleeding and had him transported immediately to the hospital. Quick action likely saved his life.
EMR Actions:
- Recognize Risk Factors:
- Note any history of anticoagulant use or bleeding disorders during the patient assessment.
- Control Bleeding:
- Apply direct pressure to bleeding wounds. Use hemostatic dressings if available.
- Monitor Neurological Status:
- Watch for signs of deterioration in patients with head injuries.
- Transport Promptly:
- Ensure rapid transport to a higher level of care for further evaluation.
11.6 Cancer and Emergency Care
Cancer involves the abnormal growth of cells that can invade and destroy normal tissues. Tumors can be benign (non-cancerous) or malignant (cancerous). Malignant tumors have the potential to spread (metastasize) to other areas of the body.
Common Cancer Treatments
- Surgery: Removal of tumors or affected tissues.
- Chemotherapy: Use of drugs to kill cancer cells or stop their growth. Common side effects include:
- Nausea and vomiting
- Fatigue
- Hair loss
- Radiation Therapy: Targets cancer cells with high-energy rays. Side effects may include:
- Skin burns or irritation
- Fatigue
Considerations for Cancer Patients
- Immunocompromised Status:
- Cancer treatments weaken the immune system, making patients more susceptible to infections.
- Follow strict hand hygiene and standard precautions.
- Fatigue:
- Patients often experience severe fatigue from treatment. This should be considered when assisting or transporting them.
- Skin Sensitivity:
- Be mindful of rashes or burns from radiation therapy. Avoid rough handling and use soft, non-abrasive materials during care.
- Pain Management:
- Many cancer patients suffer from chronic pain. Document any complaints and notify higher-level providers.
Patient Story:
Ms. Rivera, a 45-year-old woman undergoing chemotherapy for breast cancer, called 911 after experiencing severe weakness and fever. Upon arrival, the EMR team observed she was pale and tachycardic. Suspecting neutropenic fever (a life-threatening complication of chemotherapy), they ensured immediate transport to the emergency department. The team’s awareness of her immunocompromised state prevented delays in care.
Key Points for EMRs
- Understand that anticoagulants and bleeding disorders require extra vigilance in emergencies, especially after trauma.
- Recognize the unique challenges faced by cancer patients, including their increased risk for infection and the side effects of treatment.
- Always prioritize safety, rapid assessment, and transport for these vulnerable populations.
By preparing for these scenarios, EMRs can provide compassionate and effective care during critical moments.
11.7 Infectious Diseases for Emergency Medical Responders
CDC Educational Scenario:
Common Infectious Diseases Encountered by EMRs
- Hepatitis B and C: Bloodborne viruses affecting the liver.
- HIV/AIDS: Bloodborne virus that weakens the immune system.
- Tuberculosis (TB): Airborne bacterial infection primarily affecting the lungs.
- Influenza and COVID-19: Airborne viral infections causing respiratory illness.
Standard Precautions for EMRs
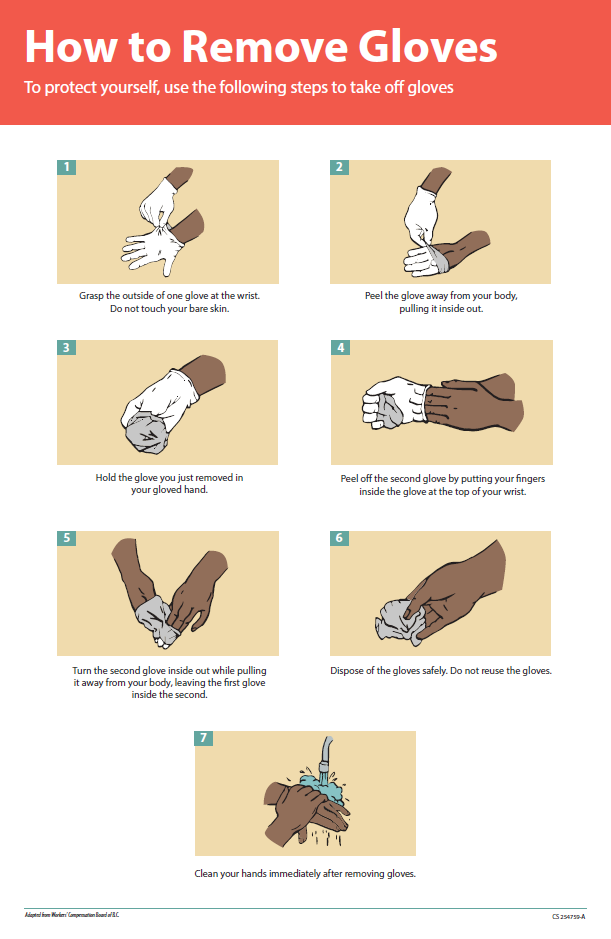
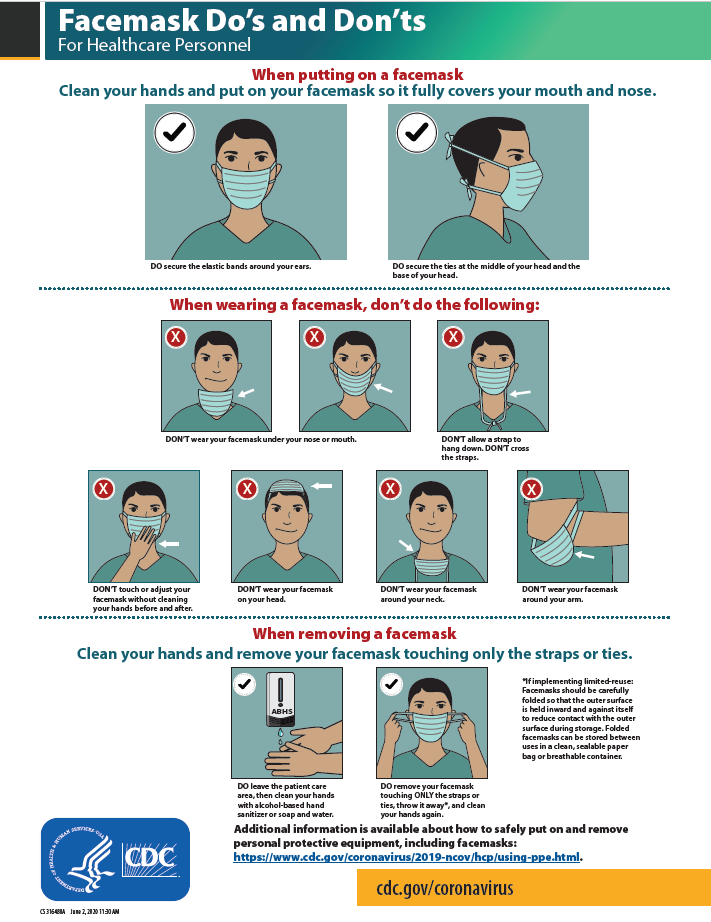
Since it is impossible to determine if a patient has an infectious disease, EMRs must always follow Standard Precautions to reduce risk:
- Hand Hygiene: Wash hands thoroughly before and after patient contact. Use alcohol-based hand sanitizer if soap and water are unavailable.
- Personal Protective Equipment (PPE):
- Gloves: Wear gloves for all patient contact.
- Masks: Use surgical masks or N95 respirators when there is a risk of airborne exposure.
- Eye Protection: Wear goggles or face shields to protect against splashes.
- Proper Disposal: Dispose of gloves, masks, and other materials in biohazard containers after use.
- Avoid Needle Sticks: Be cautious when handling sharp objects. Never recap needles.

Infectious Disease Emergencies
Bloodborne Infections
Bloodborne pathogens like hepatitis B, hepatitis C, and HIV are common concerns during emergency calls. These can be transmitted through exposure to blood or other infectious bodily fluids.
EMR Actions:
- Treat all blood as potentially infectious.
- Cover cuts or open wounds on your hands before donning gloves.
- Immediately wash the area with soap and water if exposed.
Airborne Infections
Diseases like tuberculosis and COVID-19 can be transmitted through respiratory droplets. EMRs are particularly at risk in enclosed spaces or when patients are coughing.
EMR Actions:
- Use an N95 mask if a patient has a known or suspected airborne illness.
- Ensure the patient wears a surgical mask, if possible.
- Ventilate the area during transport or care.
Sepsis
Sepsis is a life-threatening response to infection, often originating from bacterial infections. It requires immediate recognition and intervention.
Signs of Sepsis:
- Fever, chills, or low body temperature
- Rapid breathing or shortness of breath
- Confusion or altered mental status
- Low blood pressure
EMR Actions:
- Monitor the patient’s vital signs closely.
- Provide oxygen if needed and prioritize rapid transport.
Preventing Infection Exposure
- Vaccination: Stay up-to-date on recommended vaccines, such as hepatitis B and influenza.
- Exposure Follow-Up: If exposed, immediately report the incident and follow protocols for testing and treatment.
- Clean and Disinfect: Decontaminate equipment and vehicles after every call.
Key Takeaways for EMRs
- Assume All Bodily Fluids are Infectious: Always use PPE and maintain good hygiene.
- Recognize Signs of Infection: Be vigilant for symptoms of sepsis or communicable diseases.
- Protect Yourself and Others: Follow protocols to reduce the spread of infection and ensure safety.
By consistently applying these precautions and practices, EMRs can minimize risks to themselves, their patients, and others during emergency calls involving infectious diseases.
Blood-borne Pathogens Standard
Part of OSHA’s “Blood-borne Pathogens Standard” is to complete a postexposure assessment to determine if additional medical treatment is required. It is extremely important that this assessment occurs immediately after your exposure. The standard also requires your employer to offer the vaccine series for hepatitis B and hepatitis C at no cost to you if you have not previously received them.
To read more information on OSHA’s Blood-borne Pathogens Standard, visit OSHA’s Fact Sheet PDF.
Handwashing with Soap
Proper hand hygiene includes handwashing with soap and water or the use of alcohol-based hand rub. Both procedures are described in the following sections.
Handwashing With Soap and Water
Handwashing involves the use of soap and water to physically remove microorganisms from one’s hands. Certain health care situations require handwashing with soap and water instead of using alcohol-based hand rub (ABHR). For example, hands must be washed with soap and water if they are visibly soiled, have been exposed to blood or body fluids, or have been exposed to norovirus, C. difficile, or Bacillus anthracis. The mechanical action of lathering and scrubbing with soap for a minimum of 20 seconds is vital for removing these types of microorganisms.
Soap is required during handwashing to dissolve fatty materials and facilitate their subsequent flushing and rinsing with water. Soap must be rubbed on all surfaces of both hands followed by thorough rinsing and drying. Water alone is not suitable for cleaning soiled hands. The entire procedure should last 40 to 60 seconds, and soap approved by the health agency should be used.
When washing with soap and water, the Centers for Disease Control and Prevention (CDC) recommends the following steps:
-
- Wet hands with warm or cold running water and apply facility-approved soap.
- Lather hands by rubbing them together with the soap. Use the same technique as the hand rub process to clean the palms and fingers, between the fingers, the backs of the hands and fingers, the fingertips, and the thumbs.
- Scrub thoroughly for at least 20 seconds.
- Rinse hands well under clean, running water.
- Dry the hands, using a clean towel or disposable toweling, from fingers to wrists.
- Use a clean paper towel to shut off the faucet.
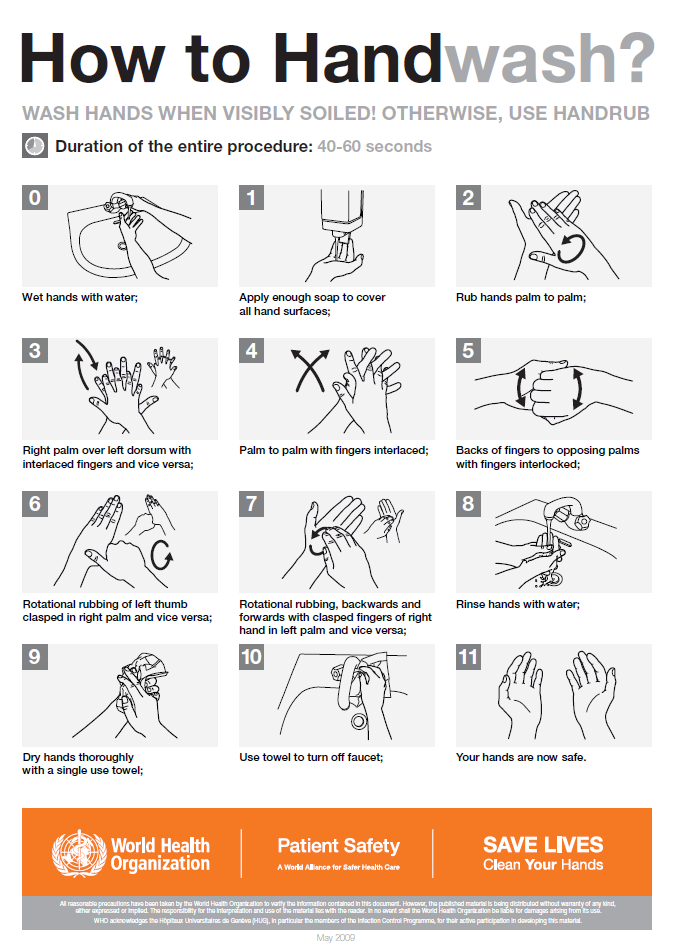
11.8 Immunology for Emergency Medical Responders
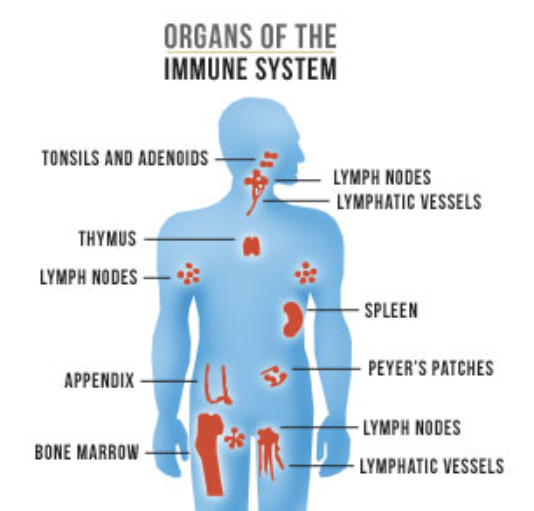
The immune system is the body’s defense mechanism against harmful invaders like bacteria, viruses, and other pathogens. It includes specialized cells, tissues, and organs working together to detect and neutralize these threats. For EMRs, understanding basic immunology helps identify and respond appropriately to emergencies involving immune system dysfunction.
The Immune System: A Brief Overview
Key Components
- White Blood Cells (WBCs): Also known as leukocytes, these are the primary defenders against infection.
- Neutrophils: Respond quickly to infections.
- Lymphocytes: Includes B-cells (produce antibodies) and T-cells (destroy infected cells).
- Lymphatic System: A network of vessels and lymph nodes that transport and filter immune cells and pathogens.
- Organs: The spleen, thymus, and bone marrow play roles in producing and supporting immune cells.
- Antibodies: Proteins that recognize and neutralize specific pathogens.
Immune Responses
- Innate Immunity: The body’s first line of defense, providing immediate but nonspecific protection.
- Adaptive Immunity: A targeted response where the body creates specific antibodies against a pathogen.
Immune Disorders
When the immune system becomes unbalanced or incorrectly reacts to “self” tissues, immune disorders can develop.These are some examples:
| Diagnosis | Definition |
|---|---|
| Asthma | Airways become swollen and narrowed in response to an environmental trigger, making it difficult to breathe. Severe asthma attacks can be life-threatening. |
| Type 1 Diabetes | The immune system attacks the pancreas and reduces the production of insulin. |
| Leukemia, Lymphoma, and Other Immune System Cancers | Ineffective white blood cells elevate the risk for life-threatening infection. |
| Human Immunodeficiency Virus (HIV) | The virus attacks white blood cells that identify pathogens in the body, and they are no longer able to fight infection. |
| Thyroid Disorders | As the thyroid is attacked by the immune system, the regulation of hormones that control metabolism, energy levels, body temperature, heart rate, and appetite are affected. |
| Multiple Sclerosis (MS) | The immune system attacks the protective sheath around the spinal cord, causing disruption of signals from the brain to body parts. Functioning can vary from day-to-day. |
Immune System Dysfunctions in Emergencies
Allergic Reactions
An allergic reaction occurs when the immune system overreacts to a harmless substance, like pollen or food. Severe allergic reactions, known as anaphylaxis, can be life-threatening.
Signs of Anaphylaxis:
- Difficulty breathing or wheezing
- Swelling of the face, lips, or throat
- Hives or itching
- Drop in blood pressure (shock)

EMR Actions:
- Epinephrine: Administer an epinephrine auto-injector (e.g., EpiPen) if available and trained to do so.
- Oxygen: Provide oxygen to support breathing.
- Transport: Rapid transport to the hospital for further treatment.

Autoimmune Disorders
These conditions occur when the immune system mistakenly attacks the body’s own tissues. Common examples include rheumatoid arthritis, lupus, and multiple sclerosis.
Patient Considerations:
- Patients may present with chronic pain, fatigue, or difficulty moving.
- Be cautious when handling patients with fragile joints or skin.
- Understand that these conditions can complicate treatment for other illnesses or injuries.
Immunocompromised Patients
Patients with weakened immune systems are more susceptible to infections and may not show typical signs of illness. Causes of immunosuppression include:
- Chemotherapy for cancer
- HIV/AIDS
- Organ transplant medications
- Congenital immune deficiencies
EMR Actions:
- Use strict infection control measures (e.g., gloves, masks) to prevent introducing pathogens to the patient.
- Monitor for subtle signs of infection, such as confusion or low-grade fever.
11.9 Immunological Emergencies
Sepsis in Immunocompromised Patients
Patients with a weakened immune system are at higher risk for sepsis, a life-threatening condition caused by a severe infection.
Signs of Sepsis:
- Fever or hypothermia
- Rapid heart rate and breathing
- Confusion or lethargy
EMR Actions:
- Monitor vital signs and provide oxygen.
- Transport promptly for advanced care.
Vaccine-Preventable Diseases
Vaccines protect against diseases like measles, mumps, and influenza. However, unvaccinated individuals or those with weakened immunity may still be at risk.
EMR Actions:
- Be aware of potential outbreaks in the community.
- Use proper PPE during suspected cases of contagious diseases.
Key Takeaways for EMRs
- Be Prepared for Allergies: Recognize anaphylaxis and know how to administer epinephrine.
- Support Vulnerable Patients: Understand the unique challenges faced by immunocompromised individuals and those with autoimmune disorders.
- Infection Control is Vital: Protect yourself and the patient through proper use of PPE and hygiene protocols.
- Act Quickly: Early recognition of immunological emergencies like anaphylaxis or sepsis can save lives.
By understanding these basics, EMRs can provide effective and compassionate care to patients with immunological concerns during medical calls.
References
American Red Cross. (2017). Emergency medical response.
Le Baudour, C., Laurélle, K., Wesley, K., & Bergeron, J. D. (2024). Emergency medical responder: First on scene (12th ed.). Pearson.
Occupational Safety and Health Administration. (2011). OSHA fact sheet: OSHA’s bloodborne pathogens standard [PDF]. https://www.osha.gov/sites/default/files/publications/bbfact01.pdf
Sandquist-Reuter, M. (2023). Nursing assistant. Open RN. https://wtcs.pressbooks.pub/nurseassist/
Images:
Figure 11.1: This image is derived from ”Urinary_System_(Female)” by BruceBlaus is licensed under CC BY-SA 4.0
Figure 11.2: ”Urinary_System_(Male)” by BruceBlaus is licensed under CC BY-SA 4.0
Figure 11.3: “poster-how-to-remove-gloves.pdf” by Centers for Disease Control and Prevention is in the Public Domain. Access for free at https://www.cdc.gov/vhf/ebola/resources/posters.html
Figure 11.4: “Screen-Shot-2021-05-05-at-3.57.19-PM” and “Screen-Shot-2021-05-05-at-3.57.41-PM” by unknown author are licensed under CC BY-NC 4.0. Access for free at https://ecampusontario.pressbooks.pub/introductiontoipcp/chapter/masks/
Figure 11.5: “fs-facemask-dos-donts.pdf” by Centers for Disease Control and Prevention is in the Public Domain. Access for free at https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html
Figure 11.6: “How_To_HandWash_Poster.pdf” by World Health Organization is licensed under CC BY-NC-SA 3.0 IGO. Access for free at https://www.who.int/infection-prevention/campaigns/clean-hands/5moments/en/
Figure 11.7: “Organs_of_the_Immune_System_by_AIDS.gov” by AIDS.gov is in the Public Domain.
Figure 11.8: “1lisinopril” by Adebayo PB, Alebiosu OC is licensed under CC BY 3.0
Figure 11.9: “Adrenalina_autoinyector10” by AngelHM is licensed under CC BY-SA 4.0
Videos:
7activestudion. (2016, November 27). Procedure of DIALYSIS [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=EU2skU3bgS8&t=19s

