Chapter 15: Trauma Part 2
Jamie Howell, MSN, RN-EMT, CHSE
15.1 Introduction
(needs to be written to be consistent with other chapters)
Learning Objectives
Missing from chapter
15.2 Multi-System Trauma
Multi-system trauma refers to injuries involving multiple organ systems within the body as a result of significant external forces. These injuries often present unique challenges for emergency responders due to their complexity and potential for rapid deterioration. Patients with multisystem trauma are at a higher risk of developing complications such as shock, making timely assessment and intervention critical.

Mechanism of Injury
Multi-system trauma is commonly seen in:
- Motor Vehicle Collisions: High-speed crashes may result in blunt force trauma to the head, chest, abdomen, and extremities.
- Falls from Height: Injuries often include fractures, internal bleeding, and spinal injuries.
- Violence: Gunshot wounds and stabbings frequently damage multiple organ systems.
- Industrial Accidents: Crush injuries may lead to musculoskeletal, respiratory, and circulatory compromise.
The severity of injuries often depends on the mechanism of injury, energy transfer, and the patient’s pre-existing health conditions.
Commonly Affected Systems
- Skeletal System: Fractures and dislocations, which may complicate mobility and lead to hemorrhage.
- Respiratory System: Rib fractures, pulmonary contusions, or airway compromise can impair breathing.
- Cardiovascular System: Blood vessel damage and internal bleeding contribute to hypovolemic shock.
- Neurological System: Head and spinal cord injuries may result in altered mental status or paralysis.
- Abdominal Organs: Liver lacerations, spleen ruptures, or bowel perforations may cause internal bleeding and infection.
Patient Presentation
Patients with multisystem trauma often display:
- Altered mental status or unconsciousness.
- Respiratory distress or abnormal lung sounds.
- Signs of shock (pale, cool, clammy skin; rapid pulse; hypotension).
- Visible deformities or open fractures.
- Abdominal tenderness or rigidity.
Management Principles
- Scene Safety and Size-Up: Ensure the area is safe for responders and assess the mechanism of injury.
- Primary Assessment: Follow the ABCDE approach:
- Airway: Ensure the airway is open and protected.
- Breathing: Administer oxygen and ventilate if necessary.
- Circulation: Control external bleeding and assess perfusion.
- Disability: Evaluate neurological status using the Glasgow Coma Scale.
- Exposure: Fully expose the patient to identify hidden injuries while preventing hypothermia.
- Rapid Transport: Multi-system trauma patients require prompt transport to a trauma center for definitive care.
- Ongoing Monitoring: Continuously reassess vital signs, pain levels, and response to interventions.
Example Scenario
A 34-year-old male is involved in a high-speed motorcycle collision.

Upon arrival:
- He is lying supine on the roadway with visible deformities to both legs.
- His helmet is intact but removed by bystanders.
- He is conscious but disoriented and complains of chest pain and difficulty breathing.
Findings:
- Unequal chest rise, diminished lung sounds on the right side (possible pneumothorax).
- Bilateral femur fractures with visible bleeding.
- Pale, cool skin with a weak, rapid pulse (signs of shock).
Interventions:
- Secure the airway and provide oxygen via a non-rebreather mask.
- Apply a chest seal if an open wound is present; prepare for needle decompression if trained.
- Control external bleeding with direct pressure and bandages.
- Immobilize fractures with splints or traction devices.
- Initiate rapid transport with continuous monitoring.
Case Study
Scenario
You are dispatched to the scene of a three-vehicle collision. One of the drivers, a 45-year-old female, was ejected from her car and was found 15 feet away on the pavement. On assessment, you observe:
- Unresponsiveness with shallow breathing.
- Bruising and deformity to the left chest.
- A distended abdomen with bruising.
- An open fracture of the right femur with active bleeding.
Questions for Consideration:
- What are the immediate life threats in this patient?
- How will you prioritize your assessment and interventions?
- What complications might you anticipate during transport?
Response Plan
- Primary Assessment:
- Airway: Perform a jaw thrust maneuver to protect the cervical spine and ensure airway patency.
- Breathing: Administer high-flow oxygen and monitor for signs of a pneumothorax.
- Circulation: Control femoral bleeding with a tourniquet and initiate fluid resuscitation if protocols allow.
- Disability: Assess for pupil response and level of consciousness.
- Exposure: Inspect the patient for additional injuries and cover with a thermal blanket.
- Transport Decision: Initiate rapid transport to the nearest trauma center with pre-arrival notification.
- Ongoing Monitoring: Continuously reassess airway, breathing, circulation, and neurological status.
Soft tissue injuries are common and affect people of all ages. These injuries can range from minor scrapes to serious, life-threatening wounds, and they can occur in almost any environment—at home, in the workplace, or during recreational activities. Soft tissues include the skin, fat, muscles, tendons, and ligaments. When these tissues are damaged, the resulting injury is categorized as a soft tissue injury. Examples are numerous and can be seen in everyday situations: an infant might bruise an arm while learning to walk, a child might need stitches after falling on the playground, a teenager could get a sunburn while at the beach, or an adult might cut their hand while working in the kitchen. All of these represent different types of soft tissue injuries.
15.3 Trauma and the Nervous System: An EMR’s Guide
The nervous system is integral to the body’s ability to function. It controls everything from basic survival functions, like breathing and heart rate, to complex processes like thinking, reasoning, and coordinating movement. The system consists of the central nervous system (CNS), which includes the brain and spinal cord, and the peripheral nervous system (PNS), which connects the CNS to the rest of the body. Trauma to the nervous system, whether from blunt force, penetration, or compression, can disrupt these vital functions, leading to a wide array of clinical signs and requiring urgent medical care.
For EMRs, understanding the impact of trauma on the nervous system is essential. A prompt and accurate assessment can significantly affect patient outcomes by preventing further injury, ensuring appropriate intervention, and facilitating timely transportation to advanced care facilities. This section provides an overview of the nervous system, how trauma can affect it, and the response required in such situations.
Nervous System Overview
The nervous system consists of two primary components:
- Central Nervous System (CNS): The brain and spinal cord, responsible for processing and transmitting information throughout the body. The brain controls cognitive functions such as memory, learning, decision-making, and emotional regulation, while the spinal cord connects the brain to peripheral nerves that extend throughout the body.
- Peripheral Nervous System (PNS): Composed of sensory and motor neurons, the PNS transmits signals between the body’s extremities and the CNS. It plays a crucial role in movement, sensation, and autonomic functions (like digestion and heart rate regulation).
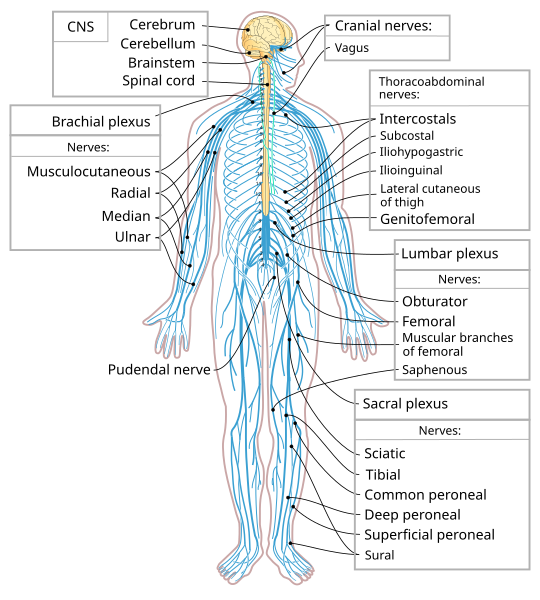
The brain itself is further divided into several regions, each responsible for specific tasks:
- The cerebrum controls higher-level functions like thinking, problem-solving, and voluntary movements.
- The cerebellum is responsible for coordination and balance.
- The brainstem regulates vital functions like heart rate, breathing, and swallowing.
The spinal cord, extending from the brainstem down through the vertebral column, transmits motor and sensory signals between the brain and the rest of the body.
Trauma to the Nervous System
Trauma to the nervous system can occur in many forms, each with unique challenges for the EMR. The severity of the injury often depends on the force, location, and type of trauma. Some injuries may result in temporary dysfunction, while others can lead to permanent damage, disability, or even death.
Types of Nervous System Trauma:
- Concussions and Brain Injuries
Concussions are mild forms of traumatic brain injury (TBI) caused by a blow to the head, which leads to temporary brain dysfunction. While many concussions resolve without permanent damage, repeated concussions or a severe blow can result in lasting effects, such as cognitive decline, memory loss, and difficulty concentrating.
Signs and Symptoms:- Confusion, dizziness, or disorientation.
- Nausea or vomiting.
- Memory loss or difficulty remembering the event.
- Headache or visual disturbances.
- Sleep disturbances.
EMR Response:
If a concussion is suspected, the primary concern is preventing further injury, especially if the patient has lost consciousness. Keep the patient still, monitor their neurological status, and transport them to a medical facility for evaluation. Additionally, in cases of repeated head trauma, the risk of post-concussion syndrome or more severe brain injury (such as a contusion) increases.
- Spinal Cord Injuries (SCI)
A traumatic injury to the spinal cord can disrupt the communication between the brain and the body, leading to paralysis or loss of sensation. Spinal cord injuries are classified as either complete (loss of all sensation and movement below the level of injury) or incomplete (partial loss of function).
Signs and Symptoms:- Loss of sensation or motor function below the injury site.
- Spinal pain, tenderness, or deformity.
- Difficulty breathing (if the injury occurs higher in the cervical spine).
- Loss of bowel or bladder control.
EMR Response:
Immediate stabilization of the spine is critical to prevent further damage. This involves maintaining the patient in a neutral, supine position, minimizing movement, and securing the neck with a cervical collar. Rapid transport to a trauma center is necessary for further evaluation and treatment.
- Peripheral Nerve Injuries
The PNS can be injured by trauma that compresses or cuts peripheral nerves. These injuries can result from fractures, dislocations, or severe blunt trauma. For example, a motor vehicle accident (MVA) or a severe fall could damage nerves in the limbs, leading to motor dysfunction or sensory deficits.
Signs and Symptoms:- Numbness or tingling in the affected area.
- Loss of muscle strength or coordination.
- Inability to move the affected body part.
- Pain or burning sensation along the nerve pathway.
EMR Response:
In cases of suspected peripheral nerve injury, immobilize the affected limb and transport the patient for evaluation. Although peripheral nerve injuries are generally less life-threatening than spinal cord or brain injuries, prompt treatment is important for recovery and function.
- Intracranial Hemorrhages
Trauma to the brain can cause bleeding within the brain or its surrounding structures. Intracranial hemorrhages (bleeding within the skull) are particularly dangerous as they can lead to increased intracranial pressure (ICP), which can cause brain damage or death.
Types of Intracranial Hemorrhages:- Epidural Hematoma (EDH): Bleeding between the skull and the dura mater (outer layer of the meninges), often caused by a blow to the head. This type of bleeding may present with a brief loss of consciousness, followed by a lucid interval and then rapid deterioration.
- Subdural Hematoma (SDH): Bleeding between the dura mater and the brain, often caused by a rapid deceleration or impact. Symptoms may develop slowly and worsen over time.
- Intracerebral Hematoma (ICH): Bleeding within the brain tissue itself, which can occur in severe trauma cases.
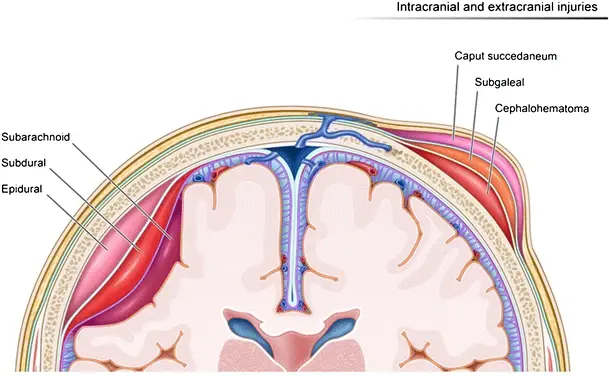
Signs and Symptoms:
- Severe headache or dizziness.
- Altered mental status or confusion.
- Slurred speech or difficulty concentrating.
- Seizures.
- Unilateral weakness or paralysis.
EMR Response:
In suspected cases of intracranial hemorrhage, airway management and oxygenation are the first priorities. If there is evidence of deterioration in mental status or worsening neurological function, immediate transport to a facility capable of performing CT scans or MRIs is critical.
15.4 Orthopedic Traumas and Emergencies for Emergency Medical Responders
Orthopedic injuries, including those affecting muscles, bones, and joints, are common emergencies encountered by first responders. These injuries can range from simple strains and sprains to severe fractures, dislocations, and multiple trauma situations. Effective care requires a clear understanding of the mechanisms of injury, signs and symptoms, and appropriate interventions to stabilize the patient while preventing further harm.
For EMRs, ensuring the patient’s comfort, maintaining immobilization, and providing reassurance are critical components of care. Orthopedic trauma can often cause significant pain, fear, and distress for the patient, emphasizing the importance of a calm and reassuring approach. This chapter builds on the foundational principles of RICE (rest, immobilization, cold, elevation) while introducing detailed case studies and practical applications.
General Guidelines for Orthopedic Trauma Care
Assessment and Immediate Response:
- Scene Safety and Standard Precautions: Always ensure the scene is safe for both the responder and the patient. Use appropriate personal protective equipment (PPE).
- Primary Survey: Assess airway, breathing, and circulation (ABCs). Ensure the patient is breathing effectively and administer supplemental oxygen if indicated.
- Control Bleeding: Apply direct pressure to external wounds. For open fractures, cover the wound with a sterile dressing before applying a splint.
- Immobilize the Injured Area: Stabilize the injured limb in the position found. Avoid unnecessary movement, which can worsen pain or cause further damage.
Critical Signs and Symptoms of Orthopedic Injuries
- Snapping Sound: Often associated with fractures or ligament tears.
- Deformity or Angulation: Visible irregularities in the shape or alignment of the limb.
- Pain and Tenderness: Frequently severe, localized to the injured area.
- Crepitus: A grinding or popping sensation at the injury site, indicating broken bones.
- Swelling and Bruising: Common due to soft tissue damage.
- Restricted Movement: Affected range of motion in the injured area.
- Loss of Circulation or Sensation: Indicates potential vascular or nerve compromise.
Examples
Case Study: Open Fracture Management

Scenario:
While responding to a car accident, you find a 27-year-old male with an open fracture to his lower leg. The bone is visibly protruding through the skin, and there is significant bleeding. The patient is pale and in visible distress.
Action Plan:
- Control the bleeding using a sterile dressing, avoiding direct pressure over the bone.
- Immobilize the leg in the position found using padded rigid splints on both sides. Secure the splints with cravats.
- Check for distal pulses, skin temperature, and capillary refill before and after splinting.
- Monitor the patient for signs of shock and provide reassurance. Arrange for rapid transport to the nearest trauma center.
Key Takeaway: Always prioritize bleeding control and immobilization in open fractures while being cautious not to manipulate the exposed bone.
Splinting Techniques for Common Orthopedic Injuries
- Dislocated Shoulder:
A dislocated shoulder will appear deformed, often with a visible hollow beneath the shoulder joint. Use a sling and binder to immobilize the arm in the most comfortable position. Place padding between the arm and chest to prevent further nerve or vascular damage.
Example: A 35-year-old basketball player dislocates their shoulder during a game. Upon arrival, you find the patient supporting their arm in a bent position. Apply a sling and binder and transport for further evaluation. - Knee Injuries:
Knee injuries may occur in a bent or straight position. Do not attempt to change the position. Use appropriate splints and padding to immobilize the knee as found. For a straight knee, apply padded rigid splints on both sides. For a bent knee, support it with a pillow or folded blanket and stabilize with shorter splints.
Example: During a hiking accident, a 50-year-old male twists his knee and cannot straighten it. You pad the bent knee and immobilize it with splints, providing stability and comfort during transport. - Ankle and Foot Injuries:
Stabilize the ankle and foot in a neutral position. Use a padded splint, such as a SAM splint or rigid boards, to immobilize the area. Ensure footwear is removed to check for swelling or circulation compromise.
Application of Cold Therapy
Cold therapy helps reduce swelling and alleviate pain. Use a commercial cold pack or a homemade ice pack, wrapped in cloth, and apply it for 10–20 minutes. Avoid applying cold directly over open wounds or fractures to prevent further discomfort.
Example: A 16-year-old soccer player sustains a sprained ankle. After immobilization, you apply a cold pack to the injury and elevate the leg while reassuring the patient.
Advanced Considerations for EMRs
- Multiple Trauma Situations: Orthopedic injuries may coexist with life-threatening conditions, such as head or spinal injuries. Always follow the primary survey and address life-threatening issues before focusing on fractures or joint injuries.
- Pediatric Considerations: Children’s bones are more flexible, making fractures less obvious. Look for swelling, deformity, and pain. Use pediatric-specific immobilization tools when available.
- Elderly Patients: Bone density loss in older adults increases fracture risk. Gentle handling is crucial, as these patients are prone to additional injuries or complications such as shock.
Examples
Case Study: Managing a Pelvic Fracture
![Google. (2025) Gemini. [Artificial intelligence system]. https://gemini.google.com/app An older woman is laying an icy surface outdoors, a look of pain on her face.](https://wtcs.pressbooks.pub/app/uploads/sites/68/2025/04/Gemini_Generated_Image_jn433rjn433rjn43.png)

Scenario:
You respond to a fall incident involving a 72-year-old female who slipped on ice. She complains of severe pain in her pelvis and is unable to move her legs. There is no visible bleeding, but the patient’s vital signs suggest possible shock.
Action Plan:
- Avoid moving the patient unnecessarily. Use a pelvic binder if available to stabilize the area.
- Check for signs of internal bleeding, such as bruising or distension in the abdomen.
- Monitor vital signs and prepare for rapid transport to a trauma facility.
Key Takeaway: Pelvic fractures often indicate internal bleeding. Stabilization and immediate transport are critical.
15.5 Understanding Soft Tissue Injuries
Soft tissue injuries involve damage to the skin, fat, muscles, tendons, and ligaments beneath the skin. The skin itself is the body’s largest organ, providing protection against pathogens, helping to regulate body temperature, and containing nerves that inform us about temperature, pain, and pressure. Beneath the skin, fat plays an important role in insulating the body and storing energy. Muscles and tendons allow movement and flexibility, while ligaments connect bones to other bones, contributing to the body’s stability.
Soft tissue injuries can occur due to trauma, repetitive use, or overexertion. While the skin is the most obvious layer that can be injured, more severe cases involve deeper structures like muscles, tendons, and ligaments, leading to swelling, internal bleeding, and loss of function. For example, a fall from a bicycle might cause a scraped knee (an abrasion), but more serious falls can cause deep muscle or tendon tears that require more extensive medical intervention.
Types of Soft Tissue Injuries
Soft tissue injuries can be classified into two main categories: closed wounds and open wounds. Both types can vary in severity depending on the extent of the injury.
Closed Wounds
Closed wounds occur when the skin remains intact but underlying tissue is damaged. These are often caused by blunt force trauma, such as being struck by an object or falling onto a hard surface. The injury does not break the skin, but internal bleeding or bruising can occur as blood vessels under the skin rupture.
Common Types of Closed Wounds:
- Contusion (Bruise): A bruise happens when small blood vessels beneath the skin are broken by impact. The blood leaks into the tissue, causing a blue or purple discoloration. For example, a child who falls on a playground might develop a bruise on their arm. While painful, bruises typically heal on their own.
- Hematoma: This is a more severe form of internal bleeding, where blood collects in a pocket or mass beneath the skin. A person who falls from a height and lands on their back, for example, might experience a hematoma. The area becomes swollen, red, or purple, and may require medical evaluation to rule out fractures or other complications.
Treatment for Closed Wounds:
- Apply cold compresses to reduce swelling and alleviate pain.
- Elevate the injured area if possible to reduce swelling.
- In cases of significant pain or swelling, or when a deeper injury is suspected, seek medical care.
Open Wounds
Open wounds occur when the skin is broken, exposing underlying tissues. These types of injuries can vary widely in severity, from minor scrapes to deep, life-threatening wounds that cause significant blood loss and potential infection.
Common Types of Open Wounds:
- Abrasion: A scraped area of skin caused by friction against a rough surface, such as when a child scrapes their knee while playing outside. Abrasions often bleed minimally but can be painful.
- Laceration: A deep cut or tear in the skin, typically caused by sharp objects such as knives, glass, or metal. Lacerations may involve both the skin and deeper tissues such as muscles or nerves. For instance, a person might sustain a laceration to the hand while using a sharp tool, requiring stitches or surgical repair.
- Puncture Wound: A puncture occurs when a sharp object, like a nail, bullet, or piece of glass, pierces the skin. These wounds can be dangerous because they can introduce bacteria deep into the tissues, leading to infection. For example, stepping on a nail can cause a puncture wound that requires prompt medical care to clean the wound and prevent complications like tetanus.
Treatment for Open Wounds:
- Clean the wound with soap and water to reduce the risk of infection.
- Apply pressure to stop any bleeding.
- Use sterile dressings or bandages to cover the wound.
- Seek professional medical care if the wound is deep, large, or shows signs of infection (redness, warmth, swelling).
Burns and Crush Injuries
Two other common types of soft tissue injuries are burns and crush injuries. Both can be severe and require immediate medical attention.
- Burns can be caused by heat (thermal burns), chemicals (chemical burns), electricity (electrical burns), or radiation (radiation burns). The severity of a burn depends on its depth and the extent of the affected area. For example, a person who touches a hot stove might suffer a superficial burn that affects only the outer layer of skin, while someone exposed to high heat for longer periods might experience a deep burn requiring specialized treatment.
- Crush injuries occur when a part of the body is compressed by a heavy object. These injuries can lead to serious soft tissue damage, including muscle necrosis and internal bleeding. For instance, if someone is trapped under rubble in a building collapse, their limbs might suffer crushing injuries, which can cause severe tissue damage and require surgery to repair.
Treatment for Burns and Crush Injuries:
- For burns, cool the area with water (not ice) and cover with a sterile bandage. Do not remove burned clothing or skin.
- For crush injuries, immobilize the area and seek emergency care immediately to manage shock, bleeding, and organ damage.
Examples
Case Study: Trauma from a Playground Fall
![Aitubo. (2025). Flux (v1.0). [Artificial intelligence system]. https://aitubo.ai/ A small child is lying on the ground crying, with playground equipment in the background. The child is bleeding from the chin.](https://wtcs.pressbooks.pub/app/uploads/sites/68/2025/04/aitubo-1748881138228.png)
Imagine a child falling from a set of monkey bars at the playground and sustaining a chin laceration. The wound may appear superficial, but a deeper inspection reveals that it involves the muscle beneath the skin. After controlling the bleeding by applying gentle pressure, the wound is cleaned with antiseptic and covered with a sterile dressing. In some cases, sutures may be necessary to close the wound, and tetanus vaccination may be required if the injury is contaminated. Aftercare involves monitoring for signs of infection and ensuring the wound heals properly.
15.6 Trauma in Special Populations: Pregnancy and Pediatrics
Special populations, such as pregnant women and children, present unique challenges in trauma care. EMRs must understand the physiological differences, potential complications, and tailored approaches needed to manage trauma in these groups effectively. This section provides practical guidance, case studies, and examples to enhance understanding.
Trauma during pregnancy can result from motor-vehicle collisions, falls, assaults, or penetrating injuries. Unique to pregnancy are risks such as abruptio placentae, where the placenta prematurely separates from the uterine wall, and uterine rupture, which may occur with severe trauma. These conditions pose life-threatening risks to both the mother and the fetus.
Key Considerations:
- Two Patients in One: Always assess and manage both the mother and fetus simultaneously. Maternal stabilization is the first priority, as fetal well-being depends on the mother’s condition.
- Physiological Changes in Pregnancy: Increased blood volume, decreased blood pressure, and changes in organ positioning can mask the severity of injuries or alter typical presentations.
- Positioning: Pregnant patients in their third trimester should be positioned on their left side to prevent compression of the inferior vena cava, ensuring proper blood flow.
General Guidelines for Trauma in Pregnant Patients
- Airway and Breathing: Ensure an open airway. Administer supplemental oxygen per protocol to maintain oxygenation for both mother and fetus.
- Circulation and Hemorrhage Control: Control external bleeding immediately. Be alert to internal bleeding, especially with signs of shock such as pallor, hypotension, or altered mental status.
- Spinal Precautions: If spinal injury is suspected, secure the patient on a backboard and tilt it slightly to the left to minimize vena cava compression.
- Fetal Monitoring: When available, fetal heart rate monitoring can help identify fetal distress.
Examples
Case Study: Motor-Vehicle Collision in the Third Trimester
![Aitubo. (2025). Flux (v1.0). [Artificial intelligence system]. https://aitubo.ai/ A pregnant woman sits on the side of a road, cellphone to ear. A wrecked vehicle can be seen in the background.](https://wtcs.pressbooks.pub/app/uploads/sites/68/2025/04/aitubo-5.jpg)
![Chat GPT. Open AI. [Artificial intelligence system]. https://openai.com/ Bruising on the upper area of a pregnant woman's abdomen](https://wtcs.pressbooks.pub/app/uploads/sites/68/2025/04/ChatGPT-Image-Jun-2-2025-10_27_40-AM.png)
Scenario:
A 28-year-old pregnant woman in her 34th week is involved in a motor-vehicle collision. Upon arrival, she is conscious but complains of abdominal pain and dizziness. Examination reveals mild vaginal bleeding and bruising over the abdomen.Action Plan:
- Position the patient on her left side to prevent vena cava compression.
- Administer high-flow oxygen to optimize maternal and fetal oxygenation.
- Control external bleeding and monitor for signs of shock.
- Prepare for rapid transport to a trauma center with obstetric capabilities.
Key Takeaway: Abdominal trauma in late pregnancy requires urgent evaluation for abruptio placentae or uterine rupture, even in seemingly minor cases.
Pediatric Trauma
Injuries are the leading cause of death in children in the United States, with motor-vehicle collisions, falls, and blunt trauma being the most common causes. Children’s unique anatomy and physiology can affect injury patterns and outcomes.
Key Considerations:
- Proportionate Vulnerabilities: Children have proportionally larger heads, softer ribs, and smaller total blood volume, making them more susceptible to head injuries, internal bleeding, and rapid deterioration from blood loss.
- Emotional Response: Children may be frightened, uncooperative, or unable to articulate their symptoms. A calm, reassuring demeanor is critical to gaining trust.
- Special Equipment: Use appropriately sized equipment for immobilization and airway management. If unavailable, adapt adult equipment with extra padding.
General Guidelines for Pediatric Trauma
- Airway and Breathing: Always ensure an open airway. Monitor closely for respiratory distress, as children’s airways are smaller and more easily obstructed.
- Bleeding Control: Even small amounts of blood loss can lead to hypovolemic shock. Control external bleeding quickly and monitor vital signs frequently.
- Immobilization: Stabilize suspected fractures and spinal injuries with appropriately sized splints or padding. Avoid moving the child unless necessary.
- Observation: Look for signs of internal injury, such as abdominal distention, tenderness, or changes in mental status.
Examples
Case Study: Child Involved in a Car Crash
![Aitubo. (2025). Flux (v1.0). [Artificial intelligence system]. https://aitubo.ai/ A young child is sitting in a car seat looking flushed and near tears](https://wtcs.pressbooks.pub/app/uploads/sites/68/2025/04/aitubo-6.jpg)
Scenario:
A 6-year-old boy involved in a car crash is found strapped into his safety seat. He is alert but crying and complains of pain in his abdomen and chest. There are no external injuries.Action Plan:
- Keep the child in the safety seat if it is undamaged to avoid unnecessary movement.
- Assess airway and breathing. Provide supplemental oxygen as needed.
- Immobilize the child while in the seat, padding gaps to minimize movement during transport.
- Monitor for signs of internal bleeding or shock, such as increased heart rate, pale skin, or lethargy.
Key Takeaway: Children in car crashes may sustain serious internal injuries even without visible external trauma. Early recognition and stabilization are crucial.
Special Considerations for Pediatric Chest and Abdominal Injuries
- Soft Rib Cage: Children’s ribs are flexible, so trauma may not result in rib fractures but can still cause significant underlying organ damage.
- Abdominal Injuries: Since children have less abdominal fat and muscle, organs like the liver and spleen are more exposed to blunt trauma.
Communication with Families
Trauma in special populations often involves family members who may be distressed or anxious. Reassuring family members while keeping them informed about the patient’s condition and care can help alleviate tension and improve cooperation.
Example: During the care of a 3-year-old injured in a fall, a parent expresses anxiety about the treatment process. Explaining each step calmly and involving them where possible (e.g., holding the child’s hand during splinting) can build trust and cooperation.
References
American Red Cross. (2017). Emergency medical response.
Le Baudour, C., Wesley, K., & Bergeron, J. D. (2019). Emergency medical responder: First on scene (11th ed.). Pearson.
Le Baudour, C., Laurélle, K., & Wesley, K. (2024). Emergency medical responder: First on scene (12th ed.). Pearson.
Newgard, C. D., Fischer, P. E., Gestring, M., Michaels, H. N., Jurkovich, G. J., Lerner, E. B., Fallat, M. E., Delbridge, T. R., Brown, J. B., Bulger, E. M., & Writing Group for the 2021 National Expert Panel on Field Triage (2022). National guideline for the field triage of injured patients: Recommendations of the national expert panel on field triage, 2021. The Journal of Trauma and Acute Care Surgery, 93(2), e49–e60. https://doi.org/10.1097/TA.0000000000003627
Images:
Figure 15.1: ”Paramedics_extract_a_patient_in_a_car_accident” by Hillelfrei is licensed under CC BY-SA 4.0
Figure 15.2: “Fatal accident near Rickenbacker Air National Guard Base” by SMSgt Ralph Branson is in the Public Domain
Figure 15.3: “Nervous_system_diagram-en” by Medium69, Jmarchn is licensed under CC BY-SA 4.0
Figure 15.4: “Illustration_depicting_hemorrhages_by_location_within_the_different_layers_of_the_meninges_(left_of_image)_and_scalp_(right_of_image)” by Nadezdha D. Kiriyak is licensed under CC BY 4.0
Figure 15.5: “Open_fracture_01” by Saltanat is licensed under CC0, Public Domain.
Figure 15.6: Google. (2025) Gemini. [Artificial intelligence system]. https://gemini.google.com/app
Figure 15.7: “Neck_of_Femur_fracture_Right_side_in_a_80_years_old_female_patient” by Drvaram is licensed under CC BY-SA 4.0
Figure 15.8: Aitubo. (2025). Flux (v1.0). [Artificial intelligence system]. https://aitubo.ai/
Figure 15.9: Aitubo. (2025). Flux (v1.0). [Artificial intelligence system]. https://aitubo.ai/
Figure 15.10: Chat GPT. Open AI. [Artificial intelligence system]. https://openai.com/
Figure 15.11: Aitubo. (2025). Flux (v1.0). [Artificial intelligence system]. https://aitubo.ai/

