Chapter 1: Preparatory Part 1
Brian Litza, EdD, NRP
1.1 Introduction
Learning Objectives
- Identify the components of Emergency Medical Services (EMS) systems.
- Identify roles and responsibilities of the emergency medical responder (EMR) from other out-of-hospital care providers.
- Identify forms of medical oversight and discuss the EMR’s role in the process.
- Identify types of medical oversight that may affect the medical care provided by an EMR.
- Identify specific statutes and regulations in your state regarding the EMS system.
EMS Systems
Modern health care has grown into an interconnected network known as a community of care. This is a system where hospitals, clinics, public health services, and emergency responders work together to support the well-being of every individual. You are about to join this healthcare team as an emergency medical responder (EMR).
The emergency medical services (EMS) system is integrated with emergency management, public health, healthcare, and public safety. Emergency management is tasked with responding to emergencies that impact the community. As part of this system, we respond to the needs of citizens and responders within a declared public emergency. We are also an arm of the public health system as we help patients through improved awareness and management of their illnesses. We go into places that many cannot and, based on our calls for help, can indicate through data trends in public health emergencies such as tuberculosis outbreaks, COVID outbreaks, or other medical syndromes. Our primary interactions are typically related to healthcare and public safety. We respond to calls for assistance and utilize medical direction to better care for our patients when we need medical advice. We respond as part of public safety to medical calls where law enforcement or the fire service may be on the scene, indicating our need for our services.

EMS Systems Overview
Today’s EMS system comprises different delivery entities depending on the community’s needs and resources. The organizational structure of EMS, as well as who provides and finances the services, varies significantly from community to community. The most common types are volunteer, governmental, private, and hospital-based agencies.
EMS Delivery Models
In a volunteer system, community members provide the manpower to respond to calls. Operational funding may be through local taxes, donations, grants, and, in some cases, insurance reimbursement.
In a governmental system, the local or county EMS system is run by a governmental entity and typically funded by them. This is traditionally run through the fire service as part of the community public safety program. There can be a “third service” model where a governmental entity contracts with an agency to provide service to the community for a cost.
Next is the private ambulance service, which can be non-profit or for-profit. Traditionally, this type of company provides EMS at a cost to the end user. The end user pays for the service directly or through insurance.
Finally, there are hospital-based services which, as the name implies, are owned and operated by the local hospital. Generally, these services are paid for directly by the patient or their insurance.
Regardless of the delivery model, EMS has become a service that most communities provide in some manner. As an EMR, you will most likely work in a volunteer system or, in some cases, as an industrial safety responder working for a manufacturing company.
EMS System Regulation
EMS systems are regulated by national, state, and local service oversight. The National Highway Transportation Safety Administration (NHTSA) provides guidelines and leadership for the EMS system, and supports research and innovation. The national model for a sound EMS system focuses on regulation and policy, resource management, human resources and training, transportation, facilities, communications, public information and education, medical direction, trauma systems, evaluation, and preparedness. While this text will not detail this model, it is important to understand that, as a provider, you will be operating within these areas and will be educated in them through your training.
An intermediary between NHTSA and the state EMS office is the National Association of State EMS Officials (NASEMSO). This organization brings all the state EMS offices together and assists NHTSA and other national partners in attaining initiatives to manage and improve EMS.
The next level of oversight comes from your state EMS agency. In Wisconsin, it is the Department of Health Services, Office of Preparedness and Emergency Health Care, Emergency Medical Services Section. Administrative statutes and rules dictate how EMS will operate within the state. In Wisconsin, there are State Statute 256 and Administrative Rule 110 (in other states, this will be different). They identify who oversees the system and how providers and practitioners are licensed and required to operate.
As an EMS provider, you must be familiar with your personal requirements to maintain your license and operate lawfully in your state. As with the state, you must also follow local policies and procedures. Your service director and medical director will educate you on local operating policies and treatment protocols that dictate how you will treat your patients.
ACCESSING THE EMERGENCY MEDICAL SYSTEM
We use public safety access points (PSAP) in the United States. This is a central location where all calls for help arrive. These PSAPs coordinate resources and can dispatch various services such as police, fire, and EMS. In many cases, they can also transfer calls to private police, fire, or EMS agencies.
When an emergency arises, the public accesses the system using the 9-1-1 telephone number. The 9-1-1 system is available in almost every community. There are two types of systems: regular and enhanced. The regular system will dial an emergency operator who will ask about your emergency and your location. The enhanced 9-1-1 system can automatically tell the operator your location and, in many cases, accept 9-1-1 text message requests.
EMR Education
Each state controls emergency medical services education. In Wisconsin, it is a cooperative process between the education system and the state EMS office as outlined in administrative rule DHS 110. Educational content is derived from the National EMS Scope of Practice Model and the National EMS Education Standards.
The National EMS Scope of Practice describes each level of EMS provider and outlines the skills and treatments that are recognized for each level of EMS provider. The states utilize this information as a base for their own scope of practice to direct providers in their state.
The National EMS Education Standards match the scope of practice but identify the educational content for each level of EMS provider. The document provides learning objectives that each new provider should learn. Again, these are guideline documents that each state uses to incorporate into its own educational standards.
Certification versus Licensure
Upon successful completion of this course you will be eligible for EMR certification, or recognition of specific training and performance standards. Many levels of EMS practitioners complete their certification through testing with the National Registry of Emergency Medical Technicians (NREMT); however this is no longer a State requirement in Wisconsin. The Wisconsin EMS Section may provide EMR certification upon successful EMR course completion.
Licensure is legal authority granted by a State for a person to practice within a defined scope. Certification is typically the precursor to licensure. However, if you do obtain NREMT certification, realize it is not authorization to practice. You must also obtain State certification or licensure. This is a surprisingly common error made by EMS practitioners.
Authorization to Practice
Each state manages its EMS system differently. Most of the time, EMS providers are authorized to perform their duties. This comes in different forms at different levels. The state will usually license a provider and determine the scope of practice. All EMS agencies must have a physician medical director, and there may be more than one depending on the size and complexity of the EMS system. Physicians medically oversee the ability to practice and treat patients. These medical directors manage protocols and guidelines for patient care. They also manage the quality improvement process to ensure any deficiencies in care are addressed, and there is a continual process to ensure good quality care. In Wisconsin, there is a process of local credentialing with a service. This assures the local service that the provider is authorized to practice under their medical director. Additionally, the local service will have policies and procedures that help manage and direct the operations of the service.
Roles and Responsibilities
As an EMR, you are part of a profession that protects the public. As such, there are responsibilities and professional standards to which you will be held. The first responsibility is ensuring you have the proper equipment to respond and that it’s in working order. Next is the responsibility for safety. You are responsible for your personal safety, that of your patient, and others on scene. You should always use appropriate safety equipment in all situations. You are responsible for ensuring your patient is kept safe, whether it is protecting from hazards, weather, or other dangers. You should help protect others by controlling the scene and being aware of hazards.
Along with maintaining safety, you will evaluate the scene for personnel and equipment needs and be able to summon additional resources. This is all critical as you assess needs for accessing the patient (as in extrication from a crashed vehicle), performing a patient assessment, and being able to administer emergency medical care until additional resources arrive.
Another key responsibility is providing emotional support to patients, their families, and fellow responders. It is essential to offer compassion and understanding as they process the events they’ve experienced.
One of the most important roles is to maintain the continuity of care for your patient. Continuity in care means that your patient will continue to get the same or better care as they progress through their medical emergency. You, as an EMR, are the first level of care a patient will encounter. It is your responsibility to ensure that you hand off care to someone equal to or greater than your training. An example would be handing your patient over to the emergency medical technicians on the ambulance or the nurse at the hospital. We have a duty to do no harm and to care for our patients to the best of our abilities. Legally, we have a responsibility to keep all medical information confidential. Our patients share very personal information about their health and well-being. We are mandated under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) to keep this information private and only share it with those that are qualified to receive this information. This includes any medical provider directly involved in their medical care. Further details on the requirements for continuity of care will be covered in the discussion of legal issues.
Finally, we are responsible for community relations. We have public health responsibilities. We assist in providing health information to the public. We do this in many ways, and some examples include blood pressure screenings, helping with health fairs, standing by at events to protect the public, and helping to educate our patients with advice to help manage their medical issues.
Professionalism
Merriam-Webster defines professionalism as “1: the conduct, aims, or qualities that characterize or mark a profession or a professional person and 2: the following of a profession (such as athletics) for gain or livelihood.” Why is this important to us as an emergency responder? The easy answer is the public has significant trust in our ability to respond to their needs and expects to be treated with dignity and respect. To conduct ourselves in a manner that meets this expectation, we must be professional in our actions. This is such an integral part of our profession you can find the Code of Ethics published by the National Registry of Emergency Medical Technicians and the National Association of Emergency Medical Technicians.
There are many characteristics of professionalism, which include integrity, empathy, self-motivation, appearance and hygiene, self-confidence, knowledge of limitations, time management, communication, teamwork, respect, tact, patient advocacy, and careful delivery of care. Let’s explore these a little more.
Integrity is doing the right thing even if no one is watching. This is a high standard of always doing what is best.
Empathy is understanding from another perspective. In EMS, it’s understanding how the patient is feeling and how they are perceiving the situation. To you, it may be routine, but to the patient, this could be a life-altering experience. We need to understand this and work from this perspective.
Self-motivation is precisely what it says. However, it’s a personal decision to be present and have something deep inside of you to want to do this job. This motivation could be an early childhood experience, it could be a need to help people, or even to emulate a hero. Regardless of the motivation, we should strive to do our best.
Most responders wear a uniform that distinguishes them from others. This is an important part of being a responder. Why? Because first impressions matter. A neat and clean appearance instills confidence in your patient to trust you and know you are there to help. When you are wearing dingy clothes or have poor personal hygiene, it can put doubt in your patient’s mind about your abilities.
Hand-in-hand with appearance is your ability to have self-confidence. This is not arrogance, but the ability to know what you know and to apply it with the confidence that you are doing the right thing. An important balance to self-confidence is knowing your limitations. We need to know when we are out of our element and don’t know what to do. This is not a weakness; it is a responsible action. We have many resources at our disposal when we hit our limits. These resources include our partners and other responders, pocket references, and of course, on-line medical control. It is better to ask and be safe and responsible than to take a guess at what to do.
The next item is time management. In the end, our patients benefit most by definitive care provided in hospitals by medical professionals. Our goal is to stabilize our patients and facilitate an efficient transfer of care so the patient can get to the hospital in the timeliest manner possible. This is why we have a structured and efficient process for evaluation and treatment of our patients. When we discuss efficiency of time, we also need to focus on communication. A professional has the ability to communicate efficiently. This is essential as we try to understand our patients’ complaints and manage the care team to manage patient care.
This coincides with the next characteristic which is teamwork. Working in emergency medical services means we work within a care team that is made of more than just medical providers. We work with law enforcement and fire departments, and therefore we must work as a team when we respond to calls for help.
Working within a team, it is important to respect your coworkers and fellow responders. Showing respect acknowledges expertise and forges a solid working relationship with other providers. Utilizing tact allows us to better communicate and show that we are respectful of their profession.
Probably one of the more important aspects is that of patient advocacy. Regardless of the circumstances, we, as providers, should always be advocates of our patients and their needs. This can be difficult in many circumstances as family or other providers may not agree with the direction of care. We must honor our patient’s wishes regardless of whether we agree.
The final characteristic is the careful delivery of care, which complements our role as patient advocates. We must ensure that we are providing care thoughtfully and attentively. This involves following the standard of care, adhering to treatment protocols, and seeking guidance when we are uncertain about the appropriate course of action.
When we discuss being professional, we incorporate all of these characteristics. The Merriam-Webster definition is truly simple, but the elements that demonstrate being professional encompass many things. We, as responders to the call of the public, must be professional. We are seen as trusted individuals who will help when the need arises. Our reputation precedes us and sets the tone when we arrive to assist a patient. We must always be professional whether on or off duty.
Maintaining Certification
An essential professional responsibility is to maintain your certification. There is nobody else responsible for your certification other than you. You will need to know when your certification expires, what you need to do to maintain it, and what you need to do to renew. This is your personal responsibility.
Generally, maintaining your certification is straight-forward. Every state has their own requirements, and you need to be familiar with those. In Wisconsin, your maintenance is outlined in DHS 110. You will have continuing education that will be required for every certification period. This is education based on the curriculum that allows providers to expand on their knowledge with new and emerging information or be refreshed on information learned but seldom used.
Along with state requirements for recertification, your service may require skill-competency verification. These are typically done one-on-one with the service director, education coordinator, or medical director for the service. This can be an important process to assure the service that your skills are current, and you are capable.
In conjunction with state and local requirements, are the assurances that you keep your professional standard. This is partially measured by your compliance with the general laws of the land. Those with criminal events can have their certification affected. Your state will determine if your crime is substantially related to your practice.
Finally, there may be a fee associated with maintaining your certification. In Wisconsin, there are no certification fees unless you are late with your renewal.
It is important to remember that your certification is your responsibility. It is your responsibility to attain the required continuing education, keep yourself free from criminal history, and maintain your competency of skill.
Quality Improvement
As a medical provider, we are focused on providing life-saving medical care. In many instances we provide nothing more than support and assurance to our patients. All services work in conjunction with their medical directors to monitor and improve the care provided. This process is called quality improvement. There are many ways this may be implemented but it is a dynamic system for continually evaluating and improving care. It is dynamic in the way it really never stops and changes based on the call and the needs of the patient. The number-one focus of quality improvement is patient safety.
It is important to understand that feedback regarding your care and your adherence to treatment protocols are a learning experience. The process is not designed to be punitive, but rather educational. If there is one area that is lacking in the EMS system, it is the monitoring of quality service. We run our calls, hand over or deliver our patient and then we don’t look back. If we want to be a good provider, we need to review what we did and see if there is a way we can improve for the next encounter. Most systems utilize a review process that takes run information and compares it to protocols or guidelines to see if the care was appropriate. Let’s dig a little deeper into this process.
There are typically three reasons why care may have fallen short or outside the guidelines: a skill-based failure, a rules-based failure, or a knowledge-based failure. Skills-based failure occurs when an individual’s or team’s lack of specific skills impairs their ability to effectively implement and sustain quality improvement initiatives. This might involve technical skills, analytical skills, leadership abilities, or other competencies. In EMS this refers to skills such as patient assessment or application of a piece of equipment.
Rules-based failure refers to errors or failures that occur when individuals follow existing rules, protocols, or guidelines that are either flawed or inappropriate for a particular situation. These failures occur not because the rules were ignored, but because the rules themselves were inadequate or incorrectly applied. This occurs when protocols are not properly reviewed, or policies or procedures prevent proper care.
Knowledge-based failure refers to errors that occur due to a lack of knowledge or expertise, leading to incorrect decisions or actions. This type of failure happens when individuals are faced with situations that require them to apply their knowledge to solve a problem, but they either lack the necessary information or misinterpret the information they do have. Much of this comes with experience but can be prevented by training and education.
Knowing the types of failures can help us put into context any suggestions for improvement that we might receive. However, as a general response we can start participating in the process before we obtain any feedback. There are four things we can do: debrief our calls, constantly question our assumptions, use decision aids when treating our patients, and ask for help.
When we complete a call, we can discuss the call with our partner or our peers. This debriefing helps us understand what we found and how we treated the patient. We can discuss the signs and symptoms, the protocol used to treat, and how the patient was treated. This helps us learn and understand for the next patient and assure we are practicing according to our protocols or guidelines.
Constantly questioning our assumptions is a critical inquiry where we review what we did, and consider what others would have done. We question if the patient was really presenting with the signs and symptoms for what we treated. It helps us be critical of ourselves and assure we are striving for excellence.
Along with the retrospective analysis, we also need to be critical of ourselves in the moment. When we question ourselves or are unsure of what to do or how to do it, we can and should rely on decision aids. These come in the form of pocket-sized protocols, an application on our phones, or an algorithm to help us decide the right path of treatment for our patient.
We must remember to ask for assistance as needed. When we are on scene, we are looked at as medical experts; be assured we are not. If we get stumped or don’t know what to do, we need to rely on our team for help or to answer questions. You are part of a care team even if you are the only one on scene. You can ask fellow responders for their advice but don’t forget you always have medical control either a radio call or phone call away. Do not hesitate to use your resources if you just can’t figure it out. It is safer for the patient and you if you ask the question.
Your service will educate you on the process within the service for quality improvement. Your goal is to be the best provider you can be and take an active role in the process. This can be done through the four tactics above. The quality improvement process is educational and helps to assure our patients get the best care in the safest manner.
1.2 Safety and Wellness
Learning Objectives
- Identify emotional reactions that the EMR may experience when faced with trauma, illness, death, and dying.
- Identify reactions that a patient’s loved ones may exhibit when confronted with death and dying.
- Identify steps in the EMR’s approach to the patient’s loved ones confronted with death and dying.
- Identify possible reactions that the loved ones of the EMR may exhibit.
- Identify signs and symptoms of critical incident stress.
- Identify steps that the EMR may take to help reduce/alleviate stress.
- Identify components of scene safety.
- Identify the importance of body substance isolation (BSI).
- Identify the steps the EMR should take for personal protection from airborne and blood borne pathogens.
- Identify the personal protective equipment necessary for each of the following situations:
- Hazardous materials
- Rescue operations
- Violent scenes
- Crime scenes
- Electricity
- Water and ice
- Exposure to bloodborne pathogens
- Exposure to airborne pathogens
- Identify legal requirements of operating emergency vehicles in Wisconsin.
- Identify the importance of careful and prudent vehicle operation both in responding to the scene or to the station.
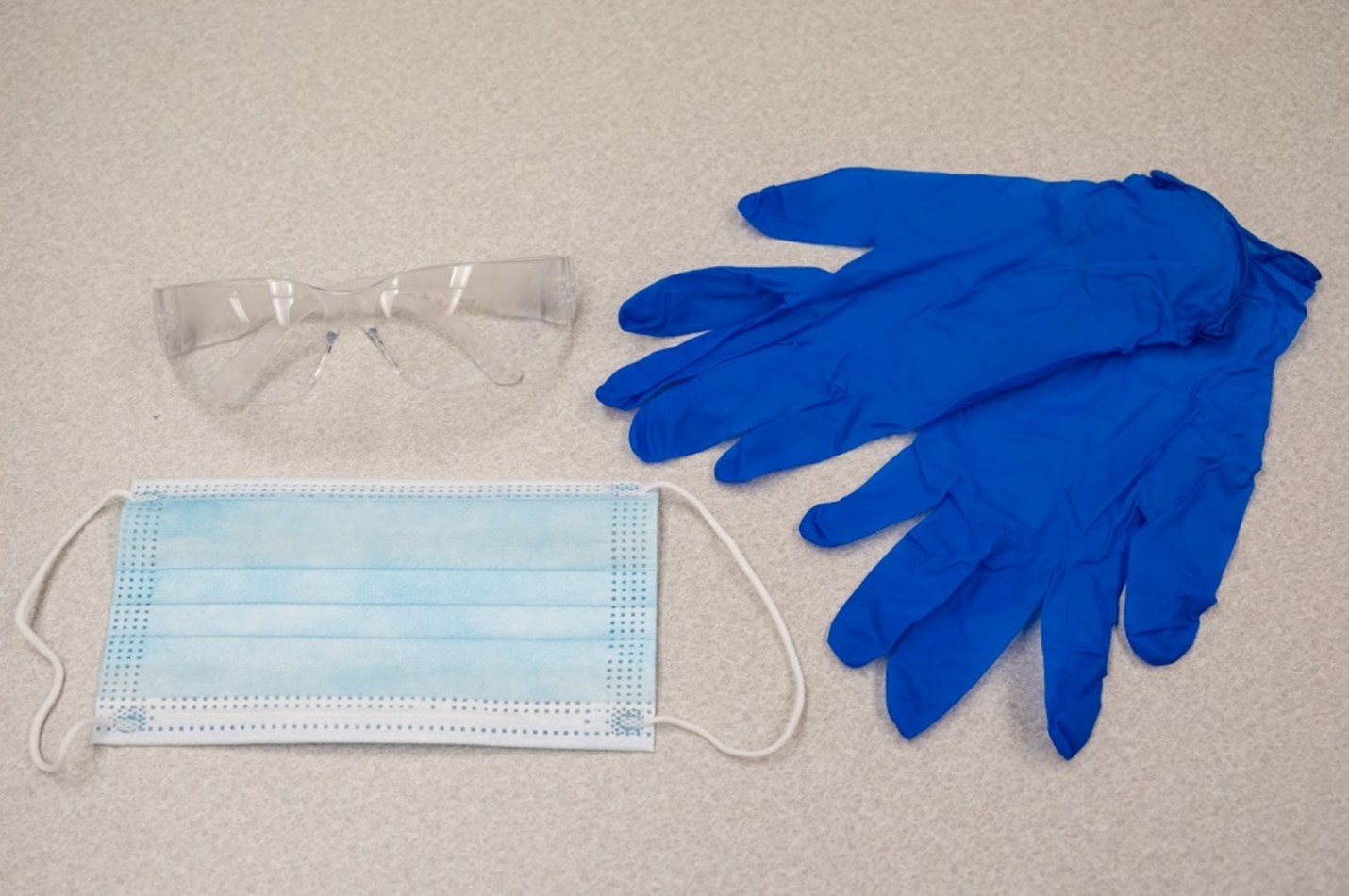
- Demonstrate appropriate use and disposal of personal protective equipment.
- Demonstrate appropriate disinfection/cleaning and all reporting documentation.
Emergency medical services can be a very demanding profession. There are many physical and psychological demands that can put stress on the body. It is very important that we understand those demands and know how to deal with their effects on our bodies and minds. In this section we will explore emotional aspects of being a responder. We will learn about stress on the job and things to help us manage that stress. We will understand how to keep ourselves healthy and ready for our response. Finally, we will discuss how to prevent us and our patients from becoming ill. It is important to remember that if we are not well enough to respond, we cannot effectively help those who need us.
Emotional Aspects
As a health care provider, we need to understand there will be considerable emotional stress on us. To be able to manage this emotional stress, we must first understand it from the patient and family perspective. Interestingly enough, we as providers can experience the same stress process when we respond to a call where we were not able to save the patient.
When a patient is diagnosed with a terminal illness they typically go through a grieving process. This is the same process a family member will go through with the patient, or after there is a sudden death of a loved one. The stages of grief are denial, anger, bargaining, depression, and acceptance. Each person must navigate these steps in their own way and on their own timetable.
- The first stage is denial. In this stage the patient or loved ones are in denial of the diagnosis or death. They experience thoughts such as “this can’t be real,”” they were too young,” or “this can’t be that bad.” When someone gets news such as this, it is a shock to the mind. It can be overwhelming as they now have to deal with their potential mortality.
- The second phase of this process is that of anger. The person starts getting angry at their higher power, themselves, or even others. This comes from the uncertainty of the situation and the lack of control over their diagnosis or death of a loved one.
- The third stage is bargaining. Again, this is an internal conversation where the individual starts to bargain for a cure or different diagnosis. Thoughts include “if you give me more time, I will be a better person,” or “if I survive this heart attack, I will be healthy and exercise.” Basically, they try to make a deal to get out of the situation.
- When the bargaining does not work its way out, they can move into depression. In this stage they start to realize the futility of their situation. They experience little reason to live and fall into depression. They start to understand the futility of trying to change the situation.
- Finally, after they move through all of these stages, they come to acceptance. They recognize the diagnosis or death of the loved one. They start to accept their situation and deal with the new reality.
The emotional stages of grief have no time limit. There is no standard to how each person moves through their emotional journey. This can be difficult for many to accept. Some people can go through these phases quickly in hours or days, yet others could take days, weeks, or even years. It is important to be aware of this emotional journey and try to provide them with emotional support.
So, how do we meet the needs of those on the emotional journey of death and dying? We will focus on two aspects: the needs of the patients and the needs of the family, friends, and bystanders. We need to assure we provide dignity to the patient, including ensuring they are covered from the neck down and they are not improperly exposed. We also need to respect the environment in which they are found and secure the scene in case the coroner needs to assess the scene and patient.
After securing the scene and providing dignity to our patient, we should turn our attention to the others present. Loved ones will be experiencing the emotions of death and dying. You will find they may express anger, rage, or despair. We need to remember that in many cases this may be unexpected and loved ones can experience a great deal of emotions which are expressed in many different ways. We need to respond by listening empathetically and supporting them as they process what has just happened to them.
When dealing with both a patient that is dying or a loved one experiencing the process, we need to let them know everything we can do will be done. We should not give false hope and promises. A potential way to console a patient or loved one would be to hold a hand, or touch an arm to reassure them. This personal touch may be awkward and needs to be communicated between the provider and the person. However, this action could be very comforting and reassuring. Many patients will offer their hand toward you or show their need in other ways. The best advice is to be present with them in the moment and attend to their needs both medically and emotionally.

Dealing with the loved ones present can also be uncomfortable. If the patient’s death is imminent, it is important to include these people in the process as much as possible. Provide updates on what you are doing and why. Engage them with questions, and if possible, allow them to be with the patient as they die.
The most important skill you can develop is supporting others. This is the emotional side of being a provider. You must be empathetic and supportive of people who may be experiencing one of the most stressful situations of their life. This can cause people to act in unpredictable and unexpected ways. We need to be professional, calm, and engaging to the needs of the patient and their loved ones.
Responder Stress
Identifying, understanding, and managing stress is an important aspect of keeping healthy. As members of public safety and healthcare, we experience stressful situations that most people may only see once or twice in a lifetime. In this section we will discuss the different types of stress and how to manage them in a healthy manner.
The types of stresses to responders are many and varied. We could respond to a mass casualty incident where there are more patients that need assistance than we can provide. We may encounter the traumatic experience of caring for a severely injured or dying child. We may observe disfiguring trauma such as amputations or grotesque injuries from which would cause the average person to turn their head away. We may also encounter infants, children, teenagers, or adults being abused. We could experience the death or severe injury of a fellow co-worker or responder. These are real. Throughout your career, you will likely experience many or all of these situations.
Understanding Stress
The first step in stress management is understanding stress. There are three reactions to stress, and they are identified as acute, delayed, and cumulative stress reactions. Acute stress reaction (ASR) is the body and mind’s immediate response to a traumatic or highly stressful event. This could be something like witnessing an accident, experiencing a natural disaster, or any situation that overwhelms a person’s normal coping mechanisms.
The symptoms of ASR can vary widely but commonly include psychological signs like intense anxiety, confusion, and emotional numbness. Physically, someone might experience symptoms such as palpitations, sweating, and hypervigilance, where they are constantly on edge and alert.
The onset of these symptoms is usually rapid, occurring within minutes to hours after the event. The good news is that ASR is generally short-lived, often resolving within a few days, although it can last up to a month. If symptoms persist beyond that, it could be indicative of a more severe condition like post-traumatic stress disorder (PTSD).
Delayed stress reaction, also known as delayed-onset PTSD, is a condition where an individual begins to experience symptoms related to a traumatic event long after the event has occurred. This delay can be quite confusing and distressing because the individual might have believed they had already processed and moved on from the trauma, only to have symptoms resurface unexpectedly. The symptoms can include flashbacks, nightmares, intrusive thoughts, avoidance behaviors, emotional numbing, hypervigilance, irritability and anger, depression, and anxiety.
The delayed onset of symptoms is one of the key characteristics of this condition. Unlike acute stress reaction, where symptoms appear immediately or within days of the traumatic event, delayed stress reaction might take weeks, months, or even years to manifest. This can happen for a variety of reasons, including the individual initially coping well, or the trauma being suppressed and only resurfacing later, often triggered by a reminder of the event or another stressor in the person’s life.
Cumulative stress reaction, sometimes referred to as chronic stress or burnout, occurs when a person is exposed to prolonged stressors over time without adequate recovery. Unlike a single traumatic event, this type of stress builds up gradually, and its effects can sneak up on a person, often going unnoticed until it becomes overwhelming.
The symptoms can include chronic fatigue, irritability, depression and anxiety, sleep disturbances, physical symptoms, and, over time, burnout. Cumulative stress is like filling a cup drop by drop. At first, it doesn’t seem like much, but over time, if nothing is done to empty that cup, it will eventually overflow. This type of stress is common in high-pressure environments, such as healthcare, emergency services, teaching, or any job that involves high demands and low control. It’s not just about big, traumatic events—minor, everyday stressors can accumulate if they’re not properly managed.
Stress responses are common and usually temporary, lasting hours to days. A stress response transitions into a stress disorder when the symptoms are persistent, are not diminishing, and significantly impact work, social interactions, or functions of daily life.
Managing Stress
Understanding the types of stress are just the first step toward management. There are five main ways we can manage our stress. These include changing our lifestyle, gaining balance in our life, understanding our responses to family and friends, managing our work environment, and seeking assistance in management.
Changing your lifestyle can be a significant way to manage stress.
- Exercise is a powerful stress-reliever. Engaging in regular physical activity helps reduce levels of stress hormones like cortisol and triggers the release of endorphins, which are natural mood-boosters. It doesn’t have to be intense. Even moderate activities like walking, cycling, or swimming can make a big difference. The goal is to get moving regularly, at least 30 minutes most days of the week. Exercise also improves sleep, reduces anxiety, and enhances overall mood, making it a cornerstone of stress management.
- Eating a balanced diet is essential for stress management. What we eat affects our energy levels, mood, and overall health. A diet rich in fruits, vegetables, whole grains, and lean proteins provides the nutrients your body needs to function properly and combat stress. Avoiding excessive caffeine and sugar is also important. While these might offer a quick energy boost, they can lead to energy crashes and exacerbate stress. Staying hydrated is often overlooked but is vital for maintaining concentration and reducing fatigue, which can be aggravated by stress.
- Quality sleep is critical in managing stress. During sleep, the body repairs itself, and the mind processes the day’s events. Lack of sleep can lead to irritability, increased stress, and difficulty coping with challenges. Establish a regular sleep routine by going to bed and waking up at the same time every day, even on weekends. Creating a calming bedtime ritual, such as reading or taking a warm bath, can also help signal to your body that it’s time to wind down. Aim for 7-9 hours of sleep per night. If you have trouble sleeping, consider cutting back on screen time before bed and creating a comfortable sleep environment.
- Practicing mindfulness and relaxation techniques like meditation, deep-breathing exercises, or yoga can greatly reduce stress levels. These practices help calm the mind, focus your thoughts, and reduce the impact of stressors. Even just a few minutes a day of mindfulness meditation can help you feel more centered and less reactive to stress. It’s about training your mind to stay in the present moment rather than worrying about the past or future. Deep breathing exercises can be particularly effective in the moment when you’re feeling stressed. Slow, deep breaths help activate the body’s relaxation response, lowering heart rate and blood pressure.
- Maintaining strong social connections is another key factor in managing stress. Positive relationships with family, friends, and colleagues provide emotional support, reduce feelings of isolation, and help us gain perspective on our stressors. It is beneficial to make time to connect with others regularly, whether it’s through a phone call, video chat, or face-to-face interactions. Social activities can provide a much-needed break from stress and help reinforce your support network. Don’t hesitate to seek support when needed. Sometimes, talking about what’s stressing you out with someone who cares can be incredibly therapeutic.
- Effective time management can reduce the feeling of being overwhelmed, which is a common source of stress. Prioritizing tasks, breaking them into smaller steps, and setting realistic deadlines can help manage workload more effectively. Learning to say no when necessary is also an important skill. Taking on too much can lead to burnout, so it’s crucial to recognize your limits and prioritize self-care.
The next strategy for managing stress is gaining balance in life. Balance affects various aspects of life: work, family, personal time, and leisure. When one area dominates your life, it can lead to burnout and increased stress. Strategies for achieving balance include prioritization, setting boundaries, and making time for yourself.
- Prioritization is identifying what is most important to you. Focus on these priorities and learn to let go of less important tasks.
- Establishing clear boundaries, at work or home, can help protect your time and energy. For example, set limits on work hours to ensure you have time for personal activities and relaxation.
- Make time for yourself. Make sure you carve out time for activities you enjoy, whether it’s a hobby, reading, or simply relaxing. This personal time is crucial for recharging and maintaining balance. To assure you are focusing on these items, you should regularly assess your life’s balance. If you notice one area is taking over, make a conscious effort to adjust your schedule or commitments to restore equilibrium.
The next focus is understanding how you respond to family and friends during stressful times. Stress often affects how we interact with others. You might find yourself more irritable, withdrawn, or overly sensitive when under stress. Recognizing these changes is the first step to addressing them. Your stress responses can strain relationships with loved ones. For example, snapping at a family member or avoiding social interactions can lead to misunderstandings and conflict.
- You can manage this by being self-aware. Pay attention to how you react to those around you, especially in stressful situations. If you notice negative patterns, acknowledge them and consider what might be triggering these reactions.
- Open communication with family and friends is key. If you’re feeling stressed, let them know what you’re going through. Often, just sharing your feelings can reduce tension and foster understanding.
- When you feel stress building up, take a moment to use relaxation techniques like deep breathing before responding to others. This can help you maintain calm and avoid reactive behaviors.
- Another tactic is to reflect on your interactions at the end of each day. Ask yourself if stress influenced any negative reactions, and think about how you could handle similar situations better in the future.
Managing your work environment is another strategy to help cope with stress. Your work environment significantly impacts your stress levels. Factors like workload, physical workspace, and relationships with colleagues all contribute to your overall stress at work.
- Consider making changes to your workspace to make it more physically comfortable. This could include ergonomic adjustments, adding personal touches, or organizing your desk to reduce clutter.
- If your workload is overwhelming, talk to your supervisor about possible adjustments. This could involve delegating tasks, extending non-critical deadlines, or prioritizing projects differently. Ensure you take regular breaks throughout the day to recharge. Short breaks can improve focus and reduce stress.
- Foster positive relationships with your colleagues. A supportive work environment can make a big difference in managing stress. As a responder, your fellow providers will become a second family and these relationships can last a lifetime.
Finally, let’s talk about seeking professional assistance. Sometimes, stress can become overwhelming despite your best efforts to manage it. If you find that stress is interfering with your daily life, relationships, or health, it may be time to seek professional help. Getting help is not a sign of weakness; it’s a sign of being strong and recognizing you come first.
- Professional support can come in many forms such as counseling and therapy, Employee Assistance Programs (EAP), medical support, or support groups. A mental health professional can help you explore the underlying causes of your stress and develop effective coping strategies. Cognitive behavioral therapy (CBT) is particularly effective in managing stress.
- In some cases, stress might lead to physical symptoms that require medical attention. A healthcare provider can help address these symptoms and may suggest stress-reducing medications if necessary.
- Sometimes, talking to others who are experiencing similar stressors can be incredibly helpful. Support groups provide a space to share experiences and coping strategies.
- REMEMBER: Don’t hesitate to reach out if you feel overwhelmed. Start by talking to your primary care physician or looking for a licensed therapist who specializes in stress management. Seeking help is a sign of strength, not weakness, and it’s an important step in taking control of your stress.
Managing stress involves making thoughtful changes across multiple areas of your life—from your daily habits and work environment to how you interact with loved ones. By prioritizing balance, recognizing your stress responses, and seeking professional help when needed, you can effectively reduce stress and improve your overall well-being.
Get Help
The 988 Lifeline website provides you judgment-free care. Using the 988 Lifeline is free. When you call, text, or chat the 988 Lifeline, your conversation is confidential. Talking with someone can help save your life.
Critical Incident Stress Management
As we have discussed, responders will experience many traumatic events within their careers. This has been recognized by the profession, and as such, we have responded by developing the Critical Incident Stress Management (CISM) process. This process is managed by trained peer counselors and mental health professionals. When there is a response to a call that is especially stressful such as a tragic death or horrific scene, we need to support one another and have a process in place to help us manage the stress and impact on our team.
This process consists of a meeting with all the responders involved. It is typically held within 24-72 hours of a major event. Responders are not required to attend but they are strongly encouraged to do so. The debriefing meeting is confidential and is an open discussion to share feelings, fears, and reactions. During the meeting, CISM leaders and mental health professionals evaluate the information and offer suggestions on how to manage the feelings being experienced by the providers. It is important to understand this is not an interrogation or investigation about the event; it is an emotional debriefing for responders to process their feelings.
This has proven to be very effective. It allows feelings to be processed in a timely manner so the detrimental effects of stress have a lesser chance to become part of one’s life. Most services have information on how to access this resource. If it is not offered after a major event, you should talk to your service or medical director and they will make the request to get the CISM meeting scheduled.
CISM is more than just a meeting to share our thoughts and feelings. It is a support system with many components. It starts with pre-incident stress education where providers become aware of the process and resources available for stress management. This is followed by on-scene peer support as well as one-on-one peer support. Many times, responders become victims themselves. An example would be a hurricane. While responders are helping others, their home and family may be at risk. This arm of CISM helps with disaster services to help assure responders and their families are cared for as well thus relieving responders of additional stress. Additional services include spouse and family support, community outreach programs and health, welfare, and wellness programs.
Definitions:
Anxiety: A sense of fear or panic, ranging from dull to intense, sometimes accompanied by confusion or a sense of being overwhelmed.
Avoidance behaviors: How a person acts to avoid anticipated unpleasant situations, which may include places, activities, or people.
Burnout: Characterized by emotional exhaustion, depersonalization (feeling disconnected from real life), and a reduced sense of personal accomplishment.
Chronic fatigue: Feeling tired all the time, no matter how much sleep one gets. The fatigue can be experienced physically, mentally, and emotionally.
Depression: Feeling persistently sad or hopeless that may or may not have an obvious cause.
Emotional numbing.: Feeling detached from emotions or relationships, almost as if going through life on autopilot.
Flashbacks: Suddenly feeling like one is reliving a traumatic event, with the same intensity of emotions and physical sensations as when it first happened.
Hypervigilance: Constantly on edge, easily startled, and always alert to potential threats.
Irritability: Easily frustrated or annoyed by things that wouldn’t normally bother one.
Intrusive thoughts: Unwanted, distressing thoughts about an event that seem to come out of nowhere and are difficult to control or push away.
Sleep disorders: This problem can include difficulty falling asleep, staying asleep, or waking up feeling unrested, which becomes a pattern, not just an occasional busy shift or night.
1.3 Responder Health
Fitness
The wellness of a provider includes both the mind and the body. When it comes to physical fitness, there are three areas of focus: cardiovascular endurance, muscle strength, and muscle flexibility.
Cardiovascular endurance refers to the ability of the heart, lungs, and blood vessels to deliver oxygen to the body’s tissues during prolonged physical activity. It’s a key aspect of overall physical health because it determines how efficiently the body can sustain exercise like running, swimming, or cycling for extended periods without excessive fatigue.
Muscle strength refers to the ability of a muscle or group of muscles to exert force against resistance. It is a critical component of physical health because it supports daily activities, maintains posture, and prevents injury. Muscle strength is developed through resistance training, such as weight lifting, bodyweight exercises, or resistance bands.
Muscle flexibility refers to the ability of muscles and joints to move through their full range of motion without restriction or discomfort. Flexibility plays a crucial role in physical health by improving mobility, posture, and functional movement. It’s often developed through stretching exercises, such as yoga or static and dynamic stretching routines.
Staying fit is important so you can be physically ready to respond. The National Heart, Lung, and Blood Institute recommends most adults should have some physical activity every day. The recommendation is at least 60 minutes a week. However, the more you do in a week the bigger the benefits.
Guidelines for all adults
Physical Activity and Your Heart: Recommendations
The guidelines advise that:
- Some physical activity is better than none. Inactive adults should gradually increase their level of activity. People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week.
- For major health benefits, do at least 150 minutes (2 hours and 30 minutes) of moderate-intensity aerobic activity or 75 minutes (1 hour and 15 minutes) of vigorous-intensity aerobic activity each week. Another option is to do a combination of both. A general rule is that 2 minutes of moderate-intensity activity counts the same as 1 minute of vigorous-intensity activity.
- For even more health benefits, do 300 minutes (5 hours) of moderate-intensity aerobic activity or 150 minutes (2 hours and 30 minutes) of vigorous-intensity activity each week (or a combination of both). The more active you are, the more you will benefit.
Spread the activity throughout the week. Muscle-strengthening activities that are moderate or vigorous intensity should be included 2 or more days a week. These activities should work all the major muscle groups (legs, hips, back, chest, abdomen, shoulders, and arms). Examples include lifting weights, working with resistance bands, and doing situps and pushups, yoga, and heavy gardening.
View the following supplementary YouTube video for a preview of yoga specific to first responders: Strong Mind, Strong Body: FireFlex Yoga Training for First Responders
The focus is on being active and not being sedentary. The best activity for your health is simply walking. Walking provides many benefits such as increased endurance and flexibility. Stay active for better health.
Sleep
Staying active also has the benefit of getting you tired which leads to the next essential element of health. Quality sleep is essential for cognitive function, physical recovery, and emotional well-being. During sleep, the brain processes and consolidates memories, which enhances learning and problem-solving abilities. It also improves focus, attention, and creativity, allowing for better decision-making throughout the day. On the physical side, deep sleep promotes muscle repair and tissue growth, while strengthening the immune system. It helps the body recover from illness and lowers the risk of chronic conditions like heart disease and diabetes. Quality sleep also stabilizes mood, reduces anxiety, and supports mental health by regulating stress hormones.
In addition to its mental and physical health benefits, good sleep is crucial for maintaining a healthy metabolism and body weight. It regulates hunger hormones, helping to control appetite and reduce unhealthy cravings, which supports weight management. Athletes and those who engage in regular physical activity benefit from improved coordination, stamina, and faster recovery due to better sleep. Furthermore, getting consistent, restful sleep is linked to a longer lifespan and a lower risk of developing chronic diseases. In essence, good sleep is a cornerstone of overall well-being, impacting nearly every aspect of health.
Getting good sleep starts with establishing a consistent sleep routine. Going to bed and waking up at the same time every day helps regulate your body’s internal clock, making it easier to fall asleep and wake up feeling refreshed. It’s also important to create a calming bedtime routine, such as reading, meditating, or stretching, to signal to your brain that it’s time to wind down. Avoid using electronic devices like phones or tablets close to bedtime, as the blue light emitted can interfere with melatonin production, a hormone that regulates sleep. Limiting caffeine and heavy meals in the evening also improves the likelihood of falling asleep quickly and staying asleep through the night.
Your sleep environment plays a significant role in sleep quality. Make sure your bedroom is dark, quiet, and cool—ideally between 60-67°F. Comfortable bedding, a supportive mattress, and reducing noise or using white noise can also promote better rest. Regular exercise during the day can make it easier to fall asleep, but avoid vigorous activity too close to bedtime, as it might increase alertness. Small lifestyle adjustments like these can greatly enhance your sleep quality, leading to improved physical health, mental clarity, and overall well-being.

Disease Prevention
We will now discuss ways to prevent illness and maintain your well-being. Disease prevention offers profound benefits by reducing the risk of developing chronic conditions and improving overall quality of life. Through proactive measures like vaccinations, regular health screenings, and maintaining a healthy lifestyle, individuals can prevent the onset of diseases such as heart disease, diabetes, and certain cancers. Preventive care helps detect health issues early, allowing for timely intervention before they become severe. This leads to better health outcomes, less need for complex treatments, and a lower financial burden from medical expenses. By focusing on prevention, individuals not only enhance their own well-being but also reduce strain on healthcare systems.
Preventing diseases also supports a longer and more active life. Regular exercise, a balanced diet, and avoiding harmful habits like smoking significantly reduce the risk of chronic illnesses and complications. Disease prevention encourages a healthier immune system, making it easier for the body to fight infections and recover more quickly when illnesses do occur. In communities, widespread prevention efforts can lead to lower transmission rates of contagious diseases, protecting vulnerable populations and promoting public health. Ultimately, prioritizing disease prevention leads to a healthier society with improved longevity and better quality of life for everyone.
Injury Prevention and Safety
Another focus of provider health is injury prevention. Injury prevention plays a critical role in maintaining long-term physical health and ensuring a higher quality of life. By adopting safety measures like proper body mechanics, stretching, and strength training, individuals can avoid many common injuries, whether from physical activity, workplace tasks, or daily movements. These strategies help reduce the risk of musculoskeletal injuries such as strains, sprains, and joint issues, allowing people to stay active and functional. Injury prevention also means less time spent in recovery or rehabilitation, which can be physically and emotionally draining, and more time enjoying activities without limitations.
For EMRs, injury prevention is crucial due to the physically demanding nature of the job, which involves lifting, moving patients, and responding to high-stress emergency situations. Adopting proper lifting techniques, such as bending at the knees and keeping the back straight, can significantly reduce the risk of musculoskeletal injuries. Using assistive devices like stretchers with mechanical lifts and maintaining good posture while performing tasks can also help prevent strain and injury. Regular physical conditioning and strength training tailored to the demands of the job further enhance the body’s ability to handle the physical stress encountered during emergency responses.

In addition to physical practices, injury prevention for emergency medical responders involves prioritizing mental and emotional well-being (see the “Responder Stress” section on page XX for more). Furthermore, adhering to safety protocols, such as wearing appropriate personal protective equipment (PPE) and being vigilant about workplace hazards, contributes to a safer work environment. By addressing both physical and psychological aspects of injury prevention, EMRs can maintain their health and effectiveness in providing critical care.
Mental Well-being
Mental well-being is a vital aspect of overall health, encompassing various factors that influence emotional, psychological, and social stability. Addressing issues related to alcohol and drug use is crucial for maintaining mental health. Substance abuse can lead to a host of problems, including depression, anxiety, and impaired cognitive function. It often exacerbates existing mental health issues and can create a cycle of dependency that impacts relationships, work performance, and daily functioning. Seeking professional help through counseling, support groups, or rehabilitation programs can aid in recovery and promote long-term mental stability.
Smoking cessation is another critical component of mental well-being. Nicotine addiction not only harms physical health by increasing the risk of respiratory and cardiovascular diseases but also affects mental health. Smokers often experience heightened stress, anxiety, and mood swings when attempting to quit. However, successfully quitting smoking can lead to improved mood and reduced anxiety levels, as well as better overall mental clarity. Support from cessation programs, nicotine replacement therapies, and counseling can help individuals manage withdrawal symptoms and sustain a smoke-free lifestyle.
Stress management is essential for maintaining mental health and preventing burnout. Chronic stress can contribute to various mental health issues, including anxiety, depression, and insomnia. See the “Responder Stress” section on page XX for detailed strategies for stress management.
Relationship issues can significantly impact mental well-being, affecting self-esteem, emotional stability, and overall happiness. Healthy relationships are crucial for providing support, companionship, and emotional fulfillment. When relationships become strained or toxic, they can lead to feelings of isolation, sadness, and frustration. Addressing relationship issues through open communication, couples therapy, or individual counseling can help resolve conflicts and strengthen connections. Building and maintaining positive relationships contributes to a more balanced and resilient mental state, enhancing overall quality of life.
Communicable Disease Prevention
When responding to emergencies, both the EMR and patient are at risk for being exposed to infectious diseases. While the previous section about disease prevention focused on how it affects an EMR’s personal health, this section is about preventing disease while treating patients. Before we discuss the prevention of disease, we must first understand what disease is. Infectious agents are organisms that cause disease by invading a host organism. They include a wide range of pathogens such as bacteria, viruses, fungi, protozoa, and helminths, each with unique mechanisms for causing illness. Infectious agents can spread through various routes, including direct contact, contaminated food or water, and vectors like insects. Vectors carry disease, typically without becoming infected themselves. Mosquitoes are the most deadly animal in the world due to their ability to pass on disease. Understanding these agents and their modes of transmission is crucial for preventing and controlling infectious diseases, as it allows for the development of targeted treatments, vaccines, and public health measures to minimize their impact on health.
Fighting the World’s Deadliest Animal
At a glance
The mosquito is the world’s deadliest animal. Spreading diseases like malaria, dengue, West Nile, yellow fever, Zika, chikungunya, and lymphatic filariasis, the mosquito kills more people than any other creature in the world. The Centers for Disease Control and Prevention (CDC) is committed to providing scientific leadership in fighting these diseases, at home and around the world.

Bacteria are single-celled microorganisms that can thrive in a variety of environments, including soil, water, and the human body. While many bacteria are harmless or beneficial, such as those aiding digestion, others can cause diseases like tuberculosis, strep throat, and urinary tract infections. Bacterial infections are often treated with antibiotics, which target specific bacterial functions. However, antibiotic resistance is a growing concern, making it essential to use antibiotics judiciously and explore alternative treatments to manage bacterial infections effectively.
Viruses are tiny infectious agents that consist of genetic material encased in a protein coat. Unlike bacteria, viruses cannot replicate on their own and must invade a host cell to reproduce. They are responsible for a wide range of illnesses, from the common cold and influenza to more severe diseases like HIV/AIDS and COVID-19. Treatment for viral infections often focuses on relieving symptoms, although antiviral medications and vaccines can help manage or prevent certain viral diseases. Vaccination remains one of the most effective strategies for controlling viral outbreaks and protecting public health.
Fungi are a diverse group of organisms that include yeasts, molds, and mushrooms. They can be found in various environments, including soil, decaying organic matter, and on the human body. While many fungi are harmless, some can cause infections, particularly in individuals with weakened immune systems or underlying health conditions. Fungal infections range from superficial conditions like athlete’s foot to systemic infections like candidiasis. Antifungal medications are used to treat these infections, but prevention through good hygiene and proper management of underlying health issues is also important.
Protozoa are single-celled microorganisms that can be found in various environments, including water, soil, and within the human body. Some protozoa are harmless, while others can cause diseases such as malaria, amoebic dysentery, and sleeping sickness. These pathogens often spread through contaminated water or food, and their life cycles can involve complex interactions with host organisms. Treatment for protozoan infections typically involves specific antiparasitic medications, and efforts to prevent these diseases include improving sanitation and access to clean drinking water.
Helminths are large, multicellular parasites commonly known as worms. They include various types of parasitic worms, such as roundworms, tapeworms, and flukes. Helminths can infect the human gastrointestinal tract or other body tissues, causing diseases like ascariasis, schistosomiasis, and tapeworm infestations. Transmission often occurs through contaminated food, water, or soil. Treatment usually involves antiparasitic drugs, and prevention strategies focus on improving sanitation, hygiene, and access to clean water to reduce the risk of helminth infections.
Prevention
Healthcare providers should have regular check-ups and tests to monitor their health and ensure that no infection has occurred. Prevention is also key. For instance, tetanus prophylaxis involves a vaccine to protect against tetanus, especially if there’s a wound. Hepatitis B vaccination helps protect against hepatitis B virus, crucial for those at risk. It’s important for healthcare providers to check their immune status to confirm they are protected against diseases like measles, mumps, or chickenpox. Access to vaccines in the community ensures that everyone can get these important shots. Tuberculin purified protein derivative (PPD) testing is used to check for tuberculosis infections, which can be treated effectively if caught early. These measures help protect healthcare workers and maintain their health while they care for others.
Standard Precautions
Body substance isolation (BSI) in EMS is designed to protect both practitioners and patients from the transmission of infectious diseases. BSI involves using a range of personal protective equipment (PPE) and hygiene practices to minimize exposure to potentially infectious body fluids. For emergency medical practitioners, key components of BSI include regular hand washing, which is one of the most effective methods for preventing the spread of infections. Eye protection, such as goggles or face shields, is essential to shield against splashes and droplets. Gloves, both vinyl or nitrile for direct patient contact and utility gloves for cleaning tasks, help protect the skin from contaminants. Gowns and masks also play crucial roles; surgical masks are used for procedures where blood splatter is possible, while high efficiency particulate air (HEPA) respirators are necessary when dealing with airborne pathogens like TB or COVID-19. The availability of specialty training ensures that practitioners are well-informed about these protocols and can apply them effectively.
To remove soiled gloves:
- Pinch the palm of one hand and pull the glove off, inverting it as you work it off your fingers.
- With the gloved hand, ball up the removed glove.
- Using your ungloved hand, slide two fingers under the cuff of the glove still on your hand.
- Invert the glove as you remove your hand from the glove.
- Dispose of the balled-up gloves properly in a garbage or hazmat bag.
Scroll through the following images to see each step in more detail
Occupational Safety and Health Administration (OSHA) and state regulations provide guidelines and mandates for BSI to ensure the safety of both healthcare providers and patients. OSHA standards require that employers implement measures to protect employees from exposure to bloodborne pathogens and other infectious materials. This includes the use of PPE, proper training, and maintaining a clean work environment. State regulations may build upon these federal standards, providing additional requirements or clarifications specific to the local context. Compliance with these regulations is crucial for minimizing health risks and ensuring a safe working environment for EMRs.
Statutes and regulations regarding notification and testing in the event of an exposure incident are essential for managing potential infections and ensuring timely response. These regulations typically mandate that healthcare providers report any exposure to potentially infectious materials to their employer or designated health authorities immediately. They also outline the procedures for testing both the exposed individual and, if applicable, the source patient. These measures are designed to promptly identify and address any potential transmission of diseases, providing a clear protocol for follow-up care and support.
State and local protocols define specific steps that emergency medical practitioners need to take in the event of a significant body substance exposure. These protocols often include immediate actions such as washing the exposed area thoroughly, reporting the exposure to a supervisor, and seeking medical evaluation. Practitioners are also required to document the incident and follow up with necessary testing and treatment as prescribed by local health authorities. Adhering to these protocols helps ensure that exposure incidents are managed effectively, minimizing the risk of disease transmission and supporting the overall health and safety of EMRs.
Managing Contamination
Recommendations for cleaning or sterilization of equipment is important to prevent the spread of germs and keep everyone safe. Equipment used in medical settings needs to be thoroughly cleaned after each use. This means first washing or wiping any visible dirt, body fluids, or contaminants off them. Then, it should be disinfected using special cleaning solutions that kill germs. There are commercially available disinfectants but you can also simply use a 1:10 ratio of bleach to water. For items that can handle high temperatures, using an autoclave (which uses steam to sterilize) is often recommended. This thorough cleaning and sterilization process ensures that the equipment is safe to use again and helps prevent infections from spreading.
Recommendations for disposing of contaminated linens and supplies, including sharps, are important for keeping everyone safe from potential infections. Contaminated linens, like towels or sheets that have come into contact with body fluids, should be placed in special bags designed for hazardous materials. These bags are then sent to a facility where they are washed at high temperatures to kill any germs. Sharp objects, like needles or broken glass, need to be disposed of in sturdy, puncture-proof containers. These containers should be clearly labeled and securely closed before being discarded. Proper disposal helps prevent injuries and ensures that potentially harmful materials are handled safely.
While it is unlikely an EMR service will be transporting a patient, you may be part of a crew that transports in an ambulance. Recommendations for decontaminating the ambulance are all about keeping the vehicle clean and safe for the next use. After each patient, the inside of the ambulance should be cleaned thoroughly. This involves wiping down surfaces that came into contact with the patient or their fluids using disinfectant cleaners. Areas like the stretcher, seats, and door handles should be given extra attention. The use of gloves and other protective gear during cleaning helps keep the person doing the cleaning safe. Regular cleaning prevents the buildup of germs and ensures the ambulance remains a safe environment for both patients and medical staff.
As an EMR, you will be exposed to many different threats. Many of these can be managed through keeping a sound mind and body. There are many safety nets in place to help you manage the hazards and keeping safety and health in mind you can stay safe throughout your career.
1.4 Research
Learning Objectives
- Describe how research affects our practice and patient care.
Historically, research in emergency and critical care medicine was difficult and sparse. However, now “Compared with most medical specialties, emergency medicine (EM) is well positioned to bridge biomedical and public health approaches for preventing disease and injury and promoting health through population-based strategies targeted at the community [2].”
You as a provider may be involved in a research study so it is important to understand the relationship we have with research and practice. Research findings, gathered through valid data collection and evidence-based methodologies, drive improvements in EMS care. These studies identify gaps in practice, validate new techniques, and help modify guidelines for better patient outcomes. Research in EMS is crucial as it ensures practices align with the latest evidence. For example, updates in CPR procedures (e.g., compression rate or depth) are rooted in global studies analyzing cardiac arrest outcomes.
Quality assurance (QA) in EMS research focuses on analyzing system performance, identifying shortcomings, and making adjustments for continuous service improvement. QA processes often analyze patient care reports, response times, and patient outcomes, guiding system enhancements. QA research identifies areas for operational improvement in EMS services, ensuring that care delivery meets or exceeds standards. This type of research can lead to better resource allocation, improve protocol adherence, and even reduce response times in critical cases.
While much of the focus of QA is looking back on performance or outcomes, considered retrospective, Quality Improvement (QI) is a forward-looking, ongoing effort to enhance the overall performance of an EMS system. Rather than focusing solely on whether mistakes were made, QI looks for patterns and trends that can inform better training, process redesign, and more effective patient care. If QA identifies that certain protocols are frequently misunderstood or not enacted, QI initiatives might introduce new training modules or revise the protocols to improve clarity. QI fosters a culture of learning and progress, aiming to raise the standard of care across the system.
Accurate data collection forms the foundation for EMS research, QA and QI. It involves gathering information such as patient demographics, care outcomes, time metrics (e.g., response and transport times), and treatment modalities. Consistent and reliable data allows for benchmarking and drives actionable research. Reliable data collection is essential for any research, QA or QI process in EMS. This includes tracking everything from response times to patient outcomes. The strength of the research is directly tied to the quality and completeness of data gathered in the field, ensuring accurate conclusions that impact policy and practices. As we will see in the next section, research relies heavily on EMS data which starts with the documentation that you create when treating a patient.
1.5 Documentation
Learning Objectives
- Identify the components of the written and electronic patient care report (PCR) and list the information that should be included in the PCR.
- Identify the various sections of the PCR.
- Identify information required in each section of the prehospital PCR and how it should be entered.
- Identify special documentation considerations associated with patient refusal.
- Identify legal implications associated with the written and electronic PCR.
- Identify state and/or local records and reporting requirements.
- Identify the elements of the HIPAA Privacy Rule as it pertains to prehospital patient care reporting.
- Identify documentation associated with special situations.
- Demonstrate accurate completion of a PCR.
Documentation is one of the most important aspects of being an EMR. The information contained in the report is essential to the continuity of care for your patient. The hospital personnel cannot be on the scene or in an ambulance as the patient is transported. The patient care report (PCR) is essential in communicating your findings, assessment, and treatments to others unable to observe the patient from first contact
Patient Care Reports Providing Data
The patient care report is a collection of data elements that create a picture of the interaction between you and your patient. The National Emergency Medical Services Information System (NEMSIS) manages the national collection and reporting of EMS data. They also set the standard for what information is collected. Many of the elements that are collected include things such as chief complaint, primary assessment findings, vital signs, and patient demographics. There is also the collection of time elements to document the sequence of events. This data contained in the report has many uses, which include continuity of care, legal representation of care provided, education, administrative, research, and quality assurance.
Think of the PCR as a “handoff” between you and the next provider. If you miss something important, like how the patient responded to treatment, that might lead to delays or errors in their ongoing care. Hospital staff might need to reference your report later when making decisions about treatment, so this is why it’s important to be accurate and detailed. The PCR also ensures that information gathered in the field is transferred accurately to the hospital staff. Since the emergency department (ED) might not read the PCR immediately, it can become crucial later on in the patient’s care. For instance, if the patient is unconscious or has undergone multiple transfers between departments, the PCR may hold key details on their initial status and interventions. Ensuring thorough and clear documentation is vital. Even seemingly small details may assist in determining the patient’s care pathway.
The next aspect of a PCR is that it is a legal document. This might sound intimidating, but it’s about being thorough and professional, and must accurately reflect all aspects of care provided. This is important because if you go to court, the PCR will often be part of the evidence used and it will be scrutinized for accuracy and clarity. The report must include precise information on what care was provided and the patient’s condition at different points—on scene and upon arrival at the hospital. You should include both objective (factual) and subjective (perceived) information in your documentation. Objective information might be something like “patient’s pulse rate is 120 bpm.” Subjective information could be “patient appears anxious.”
The PCR is often used to teach new EMS personnel the importance of proper documentation. It can also serve as a learning tool for handling unique or difficult cases, and helps highlight mistakes or areas for improvement. Your PCR might one day be used to teach new EMS providers how to document correctly, especially if it’s a complex or uncommon case. When writing, imagine that someone in a training session will read your report and use it as an example of how to handle unusual cases.
It’s not only about patient care—your PCR helps the EMS service run smoothly. Billing teams rely on your documentation to charge for services accurately. If you don’t document that you provided care or used supplies, the agency can’t properly bill to recoup its costs. Everything from the care you provide to any medications or interventions is used to justify charges. Accurate documentation ensures your department can recoup costs and maintain its budget. Your PCR also contributes to statistics that help agencies track the frequency and types of calls, staffing needs, and equipment usage. It supports resource allocation and planning.
PCRs provide valuable data for research into medical trends, patient outcomes, and effectiveness of treatments. Patterns can be identified, leading to improvements in patient care across the system. Your accurate documentation can help the whole EMS system get better at what we do. For instance, reviewing a series of PCRs might reveal that a certain intervention consistently leads to better patient outcomes, prompting changes in protocols.
Think of the PCR as your feedback loop for Quality Assurance. It’s not just about catching mistakes; it is also about highlighting what is done right and finding areas where the system can improve. PCRs are frequently used in quality-improvement programs to evaluate the level of care provided. EMS agencies review PCRs to assess how well their teams perform in the field, spot trends, and identify areas for improvement. When people talk about “continuous quality improvement” in EMS, they’re often referring to this process of reviewing PCRs to ensure everyone is delivering top-notch care. If documentation or care delivery issues arise, a PCR review can help pinpoint where and why mistakes happened.
Your PCR is more than just paperwork—it is a key part of the patient’s care journey, a legal document, an educational tool, and a foundation for administrative tasks, research, and system improvements. Taking the time to fill it out correctly ensures that everyone involved in the patient’s care, both immediately and in the future, has the information they need.
Prehospital Patient Care Report Forms
As we have discussed, the patient care report (PCR) is essential to continuity of care. Let’s discuss the PCR’s components further. You can find two types of reports that could be used. These two types are the traditional paper form with boxes and checkboxes and then the electronic version which requires a computer to complete.
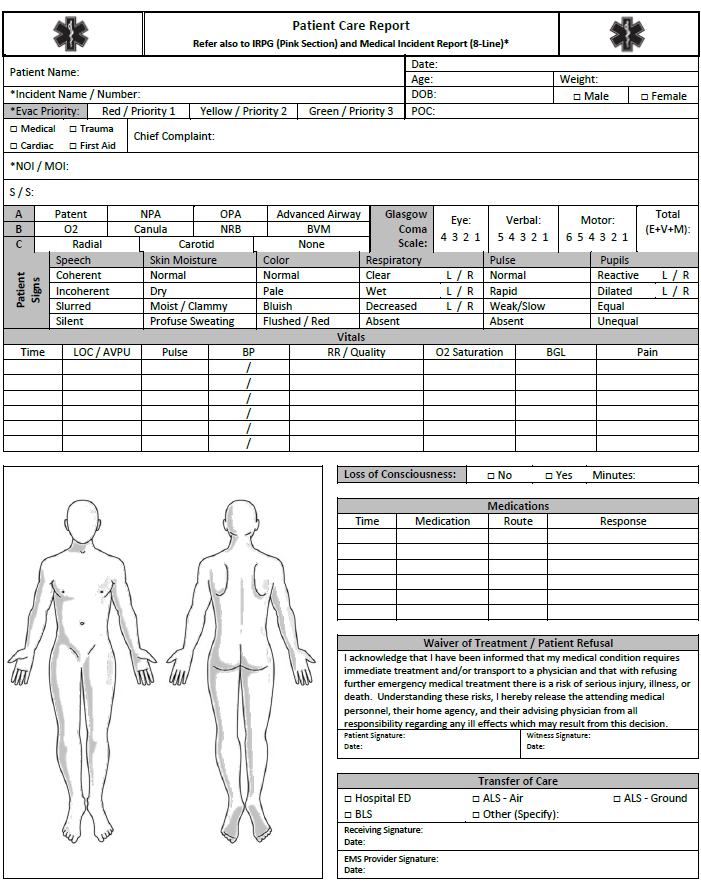
Access, download, or print a full copy of the Patient Care Report PDF
Most run reports, an older term for PCRs, will have places for run data such as date, time, service, unit number, and names of crew. There will also be a section for patient demographics such as address, date of birth, etc. The completion of the report is fairly straight-forward. You basically start at the top and work your way down. Something to focus on when completing a report is to fill in boxes completely and avoid making any stray marks. If you make a mistake, you should draw one line through the mistake and initial it. You don’t want to blacken anything out as it leaves doubt as to what was originally written and can be considered you covering something up.
Narrative
The biggest part of the PCR is the narrative section. This is where the majority of your data will be contained, the narrative should be written chronologically from the time you made patient contact to the time you handed off the patient.
Describe, don’t conclude. Stick to the facts! You are not there to diagnose or make conclusions; that is the job of the hospital staff. For example, instead of writing “patient is intoxicated,” write “patient has slurred speech and a strong odor of alcohol.” Descriptions are objective, whereas conclusions are subjective and can be misleading. Focus on documenting exactly what you observe without making assumptions. For example, instead of saying, “patient had a heart attack,” describe what you saw—chest pain, sweating, shortness of breath, etc. You might be right, but it is not our role to diagnose. Just describe!
Pertinent negatives show what you have ruled out. A pertinent negative is an important symptom or condition that is not present. For example, if a patient had chest pain but no shortness of breath, make sure to note that. Documenting these helps paint a clearer clinical picture. It shows you considered the possibility and assessed for it. “No shortness of breath” or “no signs of head trauma” are examples of pertinent negatives. They show what you checked for and found absent, which can be just as important as what is present. It’s a way to cover your bases and demonstrate thorough care.
Sometimes, the scene tells part of the story. Describe any significant scene details that may affect the patient’s condition or give context to the call. For example, if you find a suicide note, that’s critical information for the hospital staff and might shape their approach to treatment. Always make sure to document these observations carefully and objectively. Examples: “Front door was locked” or “kitchen knife on the floor near the patient.” These details provide valuable context for other healthcare providers and legal purposes.
Hospital staff and others might not be familiar with EMS abbreviations or numeric codes, and you don’t want your documentation to be confusing. Do not use radio codes or jargon in your PCR. Write in plain language to ensure anyone reading the report—whether hospital staff, administrators, or legal professionals—can understand the information clearly. For instance, instead of writing “Code 3 transport,” say “emergency transport with lights and sirens.” Keep things simple and clear for everyone reading the report.
Similarly, abbreviations are great for saving time but only use the ones everyone understands. “BP” for blood pressure is fine, but avoid local shorthand that others might not recognize. Only use common medical abbreviations that are widely understood. Unfamiliar abbreviations can lead to misunderstandings, which could compromise patient care. If someone down the line can’t understand your report, it can cause confusion or delays in care.
Sensitive information needs to be handled carefully. When documenting sensitive information (like a communicable disease or a patient’s mental health history), make sure to note where the information came from—whether from the patient, family, or records. For example, “patient’s spouse stated they are HIV-positive” or “medical bracelet indicated diabetes.” If the patient or their family tells you something, document it that way—don’t just state it as a fact.
Certain situations require mandatory reporting (e.g., child or elder abuse, domestic violence). If you suspect abuse or violence, your report might be the first step in a legal investigation. These cases require additional documentation and must follow specific legal protocols. Follow the laws for reporting, and make sure you document your observations and any mandatory steps you’ve taken.
Nothing kills credibility faster than misspelled medical terms! Spell-check your reports and be extra careful with medical terminology. Double-check terms like “myocardial infarction” or “tachycardia” to ensure accuracy. Correct spelling is crucial. Errors can lead to misunderstandings or make your report look unprofessional. A small typo could change the entire meaning of your report or make it harder for others to understand.
Every time you reassess the patient, document the time and your findings. Make sure you record both the time and what you found. For example, “At 12:45, patient’s blood pressure was 140/90 and heart rate was 100.” It helps build a timeline of the patient’s condition and shows how they responded to care over time. This can be critical information for the hospital and for any follow-up evaluations.
Following these documentation guidelines ensures that your PCR is accurate, professional, and useful for everyone involved in patient care. From the hospital staff to legal professionals, clear and complete documentation can make all the difference in how a patient’s care is managed and reviewed.
Legal Requirements
As we just discussed, there are local and state requirements that need to be considered. First there is the Health Information Portability and Accountability Act of 1996 (HIPAA). This was put into place to assure that patient healthcare information is kept confidential and is only shared with those that have a need to know. This is typically only those involved with the care of the patient so keep that in mind as you discuss or share information.
The next consideration (in Wisconsin) is DHS 110.34(8) and (9) (below). This requires services to comply with report submission to the Wisconsin Ambulance Run Data System (WARDS) and the data requirements identified by Wisconsin and NEMSIS.
“…input to WARDS or uploading patient care report data to WARDS within 7 days of the patient transport. If the emergency medical service provider is an emergency medical responder service provider, submit a patient care report to WARDS only if advanced skills are used in caring for the patient.”
The requirement is that EMRs need to submit a report when they have used advanced or optional skills. These skills include, but are not limited to, spinal immobilization, advanced airway, or medication administration, and are defined in the Scope of Practice document which is updated annually.
WI EMS Scope of Practice
Visit the following website to access, view, or download scope of practice documents: EMS: Scope of Practice and Protocols
Mandatory Reporting
In Wisconsin, EMRs and other healthcare providers have mandatory reporting requirements, particularly when protecting vulnerable populations. Here are the key situations where mandatory reporting is required:
The Wisconsin Child Abuse or Neglect (Wisconsin Legislature – Statutes 48.981) law requires healthcare providers, including EMRs, to report any suspected cases of child abuse or neglect. They should report any situation where a child has been harmed or is at risk of harm through physical, sexual, or emotional abuse, or neglect. The reporter does not need proof—just a reasonable suspicion. Typically, reports are made to county social services, child protective services, or law enforcement.
EMRs are required to report suspected abuse, neglect, or exploitation of an elderly adult (typically defined as someone 60 years or older) or at-risk adult (Wisconsin Legislature – Statutes 46.90). They should report physical abuse, emotional abuse, financial exploitation, neglect, or self-neglect. This should be reported to the local adult protective services, social services, or law enforcement.
While Wisconsin law does not mandate that healthcare providers report domestic violence for competent adult victims unless they request it, EMRs should document their findings and encourage victims to seek help. However, if the domestic violence affects children or vulnerable adults, mandatory reporting laws for those groups apply. If a child or vulnerable adult is also involved in the domestic violence situation, mandatory reporting for child abuse or elder abuse would be triggered.
Wisconsin law requires medical providers, including EMRs, to report gunshot wounds or other life-threatening injuries caused by violence, such as stab wounds (Wisconsin Legislature – Statutes 255.40). You should report any situation where a gunshot wound or a wound believed to have occurred due to a crime is suspected. These injuries must be reported to local law enforcement.
EMRs must report certain types of deaths to the appropriate authorities (Wisconsin Statute 979.01). You should report unnatural deaths, deaths resulting from violence, or deaths that occur under suspicious circumstances. Local law enforcement is typically involved. These are generally reported to the county coroner or medical examiner’s office.
Healthcare providers, including EMRs, are required by Wisconsin’s public health laws to report certain communicable diseases, such as tuberculosis, certain sexually transmitted infections (STIs), or other diseases deemed a public health threat (Wisconsin Administrative Code DHS 145). Any disease listed under the Wisconsin Department of Health Services (DHS) communicable disease reporting requirements must be reported. Reports are typically made to the local health department or Wisconsin DHS.
Similar to domestic violence, EMRs are not generally required to report adult sexual assault unless the victim consents. However, if the victim is a minor or vulnerable adult, mandatory reporting for child or elder abuse applies. Reports typically go to law enforcement or child/adult protective services.
As an EMR in Wisconsin, you are a mandated reporter in certain situations, particularly involving vulnerable populations such as children, the elderly, or those involved in violent situations. These reports are essential for protecting at-risk individuals and ensuring they receive the help they need. Always follow local protocols for reporting and document the source of any sensitive information accurately in your reports.
Falsification of Information
Falsification in medical documentation occurs when inaccurate information is recorded, either through errors of omission (failing to document something) or commission (documenting something incorrectly). In such cases, it is critical to record what was missed or done incorrectly, as well as any corrective actions taken. This ensures transparency and accountability. Accurate documentation, especially when addressing errors, prevents further confusion or harm down the line. Failing to do so can lead to miscommunication between healthcare providers, potentially jeopardizing the patient’s care.
Falsifying information in a patient care report can have serious consequences. Not only does it risk suspension or revocation of the EMS provider’s certification or license, but it can also lead to improper patient care. Other healthcare providers rely on the information in these reports to make informed treatment decisions. Misrepresenting vital signs or treatments, such as falsely documenting the administration of oxygen, creates a false clinical picture, which can result in inappropriate or delayed care for the patient. It’s essential to document only what was truly observed or performed, even if mistakes were made.
Documentation and Patient Refusals
Many services prohibit EMRs from obtaining a patient’s refusal for liability reasons. Your best course of action is to summon an ambulance and have their personnel assess and obtain a refusal. To understand the process, we will discuss refusals.
When a competent adult patient refuses treatment, EMS practitioners should respect the patient’s right to make that decision. However, before leaving the scene, the EMS provider should make every effort to persuade the patient to accept care, particularly transport to a hospital. This involves a respectful, thorough conversation where the practitioner tries to explain the potential benefits of treatment and the risks of refusal. The goal is to ensure the patient is fully informed before making a final decision.
To ensure the patient is making a rational, informed choice, EMS practitioners must assess the patient’s mental capacity. This includes verifying that the patient is not impaired by substances, medical conditions, or other factors that could cloud their judgment. Only when the patient demonstrates the ability to understand the consequences of their decision should their refusal be accepted. Additionally, the practitioner should explain the possible outcomes of refusing treatment, including the potential for serious harm or death.
Local protocols may require the EMS provider to consult with medical direction when a patient refuses care. This step ensures that a higher level of medical oversight is involved in the decision, especially in complex cases. If, after this consultation and all efforts to persuade the patient, they still refuse, the EMS provider must thoroughly document the situation. This documentation should include any assessment findings and care provided up to that point.
The next critical step is obtaining the patient’s signature on a refusal form, acknowledging that they have declined treatment against medical advice. If the patient refuses to sign, a family member, bystander, or law enforcement officer should sign the form to witness the refusal. This ensures there is a documented third-party verification of the patient’s decision, which can protect both the EMS provider and the patient legally.
The prehospital care report must be completed in detail. This report should include a thorough patient assessment, or if the patient declined a full assessment, documentation of the portions completed. The EMS provider should also note the care that was offered but refused by the patient, ensuring that a clear record is available of all actions taken to help the patient.
Lastly, include in the report a statement confirming that you informed the patient of the risks of refusal, including possible death, and offered alternative care options, such as contacting a primary care provider. It is also important to note that the EMS provider expressed a willingness to return if the patient changed their mind. This comprehensive documentation helps protect the patient’s rights while safeguarding the EMS provider from legal and medical liability.
Special Situations
When errors are discovered after a PCR form has already been submitted, it is important to correct them properly. The preferred method for correcting errors in handwritten reports involves drawing a single line through the error. The EMR should then initial and date the correction, along with providing the correct information. If any information was omitted, a note should be added with the missing details, along with the date and initials to maintain accuracy and accountability.
For electronic PCRs, many systems have built-in methods for entering corrections or amendments after submission. If an error is discovered after the report is completed electronically, the EMR should follow the system’s protocol for making changes or adding an addendum. However, if the electronic system does not have a method for corrections, print the report and follow the correction process used for handwritten reports by marking and dating the error and adding the correct information.
In cases of multiple casualty incidents (MCI), it’s often impractical to complete detailed reports before moving on to the next patient. In such scenarios, you may need to fill out the report later. Local MCI plans generally have procedures for temporarily recording essential medical information, such as using triage tags, which can be referenced when completing the report after the event. The standard for completing PCRs during an MCI differs from routine calls, with specific guidelines outlined in the local MCI plan to handle the high volume of patients.
Special situation reports are necessary when events occur that require reporting to local authorities or when additional information is needed to supplement the primary PCR. These reports must be submitted promptly and include the names of all individuals, agencies, and facilities involved in the incident. Accuracy and objectivity are critical when writing these reports, with a focus on describing the facts rather than drawing conclusions.
You should keep a copy of special situation reports when appropriate or allowed, ensuring you have a record for your own files. The report, along with any necessary copies, should be submitted to the appropriate authority as dictated by local protocols. This ensures proper follow-up and legal compliance for situations that may involve public health or safety concerns.
Special situation reports often involve documenting incidents like exposures to hazardous substances or injuries sustained during the event. These types of occurrences require immediate reporting to ensure the safety and well-being of the practitioner and the patient, and to trigger any necessary medical or legal actions.
References:
EMS Agenda 2025. (2021). The different types of EMS services. https://emsagenda2050.org/the-different-types-of-ems-services/
EMS.gov. (2024). Education. https://www.ems.gov/resources/search/?category=education#sort=date
Erich, J. (2011). Dead tired. Hmpgloballearningnetwork.com. https://www.hmpgloballearningnetwork.com/site/emsworld/article/10225273/dead-tired
Federal Emergency Management Agency. (n.d.). Emergency medical services. U.S. Fire Administration. https://www.usfa.fema.gov/ems/
Gillespie, C. B. (2013.). Revised code of ethics. NAEMT. https://www.naemt.org/about-ems/code-of-ethics (Original work published 1978)
Goss, J., & Simpson, L. (2006). The need to be more professional. Journal of Emergency Medical Services (JEMS) [Internet]. https://www.jems.com/ems-management/need-be-more-professional/
Mountfort, S., & Wilson, J. (2022). EMS provider health and wellness. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK493236/
National Association of Emergency Medical Technicians. (2025). EMS research. NAEMT. https://www.naemt.org/initiatives/ems-research
National EMS Quality Alliance. (n.d.). About. NEMSQA. https://www.nemsqa.org/about
National Highway Traffic Safety Administration (NHTSA) Office of EMS. (n.d.). State EMS systems. EMS.gov. https://www.ems.gov/issues/state-ems-systems/
National Highway Traffic Safety Administration (NHTSA) Office of EMS. (n.d.-a). 2019 national EMS scope of practice model available. EMS.gov. https://www.ems.gov/resources/newsletters/may-2019/2019-national-ems-scope-of-practice-model-now-available/
National Highway Traffic Safety Administration (NHTSA) Office of EMS. (n.d.-b). Education. EMS.gov. https://www.ems.gov/resources/search/?category=education#sort=date
National Highway Traffic Safety Administration (NHTSA) Office of EMS. (n.d.-c). Evidence-based guidelines. EMS.gov. https://www.ems.gov/resources/search/?category=evidence-based-guidelines#sort=date
National Highway Traffic Safety Administration (NHTSA) Office of EMS. (2025). Using EMS data. EMS.gov. https://www.ems.gov/issues/using-ems-data/
National Highway Traffic Safety Administration (NHTSA) Office of EMS. (2021). National EMS scope of practice model 2019: Including change notices 1.0 and 2.0 [PDF]. nasemso.org/. https://s3.amazonaws.com/ClubExpressClubFiles/157064/documents/National_EMS_Scope_of_Practice_Model_2021__438270816.pdf?AWSAccessKeyId=AKIA6MYUE6DNNJ6ROIH3&Expires=1748481222&response-content-disposition=inline%3B%20filename%3DNational_EMS_Scope_of_Practice_Model_2021_.pdf&Signature=KIw5Esypedt1VSPqLLfoAl8lxmg%3D
National Registry of Emergency Medical Technicians. (n.d.). Code of conduct. https://www.nremt.org/Policies/Certification-Policies/Code-of-Conduct
National Registry of Emergency Medical Technicians. (n.d.-a). National registry research department. https://www.nremt.org/Document/research
Office for Civil Rights. (2024). HIPAA for professionals. U.S. Department of Health and Human Services. https://www.hhs.gov/hipaa/for-professionals/index.html
Prehospital Guidelines Consortium. (2025). About us. https://prehospitalguidelines.org/about/
UCLA Center for Prehospital Care. (n.d.). About us. https://www.cpc.mednet.ucla.edu/about
U.S. Department of the Interior. (n.d.). Critical incident stress management. National Interagency Fire Center. https://www.nifc.gov/resources/taking-care-of-our-own/about-critical-incident-stress-management
U.S. Department of Labor. (n.d.). Critical incident stress guide. Occupational Safety and Health Administration. https://www.osha.gov/emergency-preparedness/guides/critical-incident-stress
U.S. Department of Health and Human Services. (2022). Physical activity and your heart: Recommendations. National Heart Lung and Blood Institute. https://www.nhlbi.nih.gov/health/heart/physical-activity/tips
Wisconsin Department of Health Services. (2024). Emergency medical services (EMS). https://www.dhs.wisconsin.gov/ems/index.htm
Wisconsin Department of Health Services. (2025). EMS: Scope of practice and protocols. https://www.dhs.wisconsin.gov/ems/licensing/scope.htm
Wisconsin State Legislature. (n.d.). Chapter 256 emergency medical services. https://docs.legis.wisconsin.gov/statutes/statutes/256/
Wisconsin State Legislature. (2025). Wisconsin administrative rule 110: Chapter DHS 110 emergency medical services licensing, certification, and training requirements. https://docs.legis.wisconsin.gov/code/admin_code/dhs/110/110
Images:
Figure 1.1: “EMS_pinwheel_graphic_4wings_F-1698341012” by unknown author, ems.gov, is in the Public Domain. Access for free at https://www.ems.gov/issues/ems-collaboration/
Figure 1.2: ”pexels-rdne-6519869” by RDNE Stock project, via Pexels is licensed under CC0
Figure 1.3: ”pexels-olly-3771069” by Andrea Piacquadio, via pexels.com is licensed under CC0
Figure 1.4: ”pexels-shox-28271067” by SHOX art, via pexels.com is licensed under CC0
Figure 1.5: ”Mosquito_Tasmania_crop” by JJ Harrison is licensed under CC BY-SA 3.0
Figure 1.6: “bmcc_book_photos-13” by Nickolas Oatley is licensed under CC BY-NC 2.0
Figure 1.7: “Patient Care Report by the U.S. Forest Service is in the Public Domain. Access for free at https://www.fs.usda.gov/sites/default/files/FS-6900-EMS-PCR-Form.pdf
Videos:
Fireflex Yoga. (2024, February 14). Strong mind, strong body: FireFlex Yoga training for first responders [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=w8msyMhLA_I
WCTCFire&EMS. (2019, March 24). Paramedic 1.12 – Workforce safety and wellness: Lifting and moving patients [Video]. YouTube. CC BY 4.0. https://www.youtube.com/watch?v=Q9nUVniccp4
National Highway Traffic Safety Administration
Validation of knowledge or skills provided by an oversight agency, such as CPR certification
Legal authority granted by a State for a person to practice within a defined scope.
Health Insurance Portability and Accountability Act of 1996
Feeling persistently sad or hopeless that may or may not have an obvious cause.
A sense of fear or panic, ranging from dull to intense, sometimes accompanied by confusion or a sense of being overwhelmed.
Constantly on edge, easily startled, and always alert to potential threats.
Suddenly feeling like one is reliving a traumatic event, with the same intensity of emotions and physical sensations as when it first happened.
Unwanted, distressing thoughts about an event that seem to come out of nowhere and are difficult to control or push away.
How a person acts to avoid anticipated unpleasant situations, which may include places, activities, or people.
Feeling detached from emotions or relationships, almost as if going through life on autopilot.
Easily frustrated or annoyed by things that wouldn’t normally bother one.
Characterized by emotional exhaustion, depersonalization (feeling disconnected from real life), and a reduced sense of personal accomplishment.
Feeling tired all the time, no matter how much sleep one gets. The fatigue can be experienced physically, mentally, and emotionally.
Critical Incident Stress Management or Debriefing
The basic level of infection control precautions used in the care of all patients. Components include hand hygiene, personal protective equipment such as gloves, and proper clean up and disposal of bodily fluids.
Body Substance Isolation, which is appropriate equipment to protect healthcare workers from bodily fluids and other potentially infectious materials.
Personal Protective Equipment, which is appropriate equipment to protect healthcare workers from bodily fluids and other potentially infectious materials.
Occupational Safety and Health Administration
Quality Assurance, which is review of standard performance to confirm adherence to guidelines or find areas for improvement, usually retrospective.
Quality Improvement or Continuous Quality Improvement which is developing ways to improve performance or processes, more prospective and ongoing
Patient Care Report or Electronic Patient Care Report
Wisconsin Ambulance Run Data System
National Emergency Medical Services Information System
Mass Casualty Incident

