6.3 Anatomy of the Skeletal System
Anatomy of the Skeletal System[1]
Shapes of Bones
At birth, a baby has 270–300 bones, some of which are made entirely of cartilage. These bones eventually fuse (grow together) to form 206 adult bones. Bones stop growing in length between the ages of 18 and 21, but the total amount of bone tissue a person has (called bone density) continues to increase slowly until the late 20s.
Bone tissue, also called osseous tissue, is different from other tissues in the body. Bone is hard and many of its functions depend on that hardness characteristic.
The 206 bones that compose the adult skeleton are divided into five categories based on their shapes. Each bone shape has a distinct function:
- Long Bones: A long bone is cylindrical in shape and is longer than it is wide. Long bones are found in the arms (i.e., humerus, ulna, and radius) and legs (i.e., femur, tibia, fibula), as well as in the fingers (i.e., metacarpals and phalanges) and toes (i.e., metatarsals and phalanges). Long bones function as levers that move when muscles contract.
- Short Bones: A short bone is cube-like in shape and about the same size in length, width, and thickness. The only short bones in humans are the carpals of the wrists and the tarsals of the ankles. Short bones provide stability and support, as well as some limited motion.
- Flat Bones: A flat bone is typically thin, but it is also often curved. Examples of flat bones include the cranial (skull) bones, the scapulae (shoulder blades), the sternum (breastbone), and the ribs. Flat bones serve as points of attachment for muscles and often protect internal organs.
- Irregular Bones: An irregular bone has a complex shape, such as the vertebrae that protect the spinal cord. It does not have an easily described shape and, therefore, does not fit any other classification. For example, many facial bones are classified as irregular bones.
- Sesamoid Bones: A sesamoid bone is a small, round bone that is shaped like a sesame seed. These bones form in tendons and help to protect them. Sesamoid bones vary in number and placement from person to person but are typically found in tendons associated with the feet, hands, and knees. The patellae (singular = patella) are the largest sesamoid bones found in humans.
See Figure 6.5[2] for an illustration of the classification of bones.
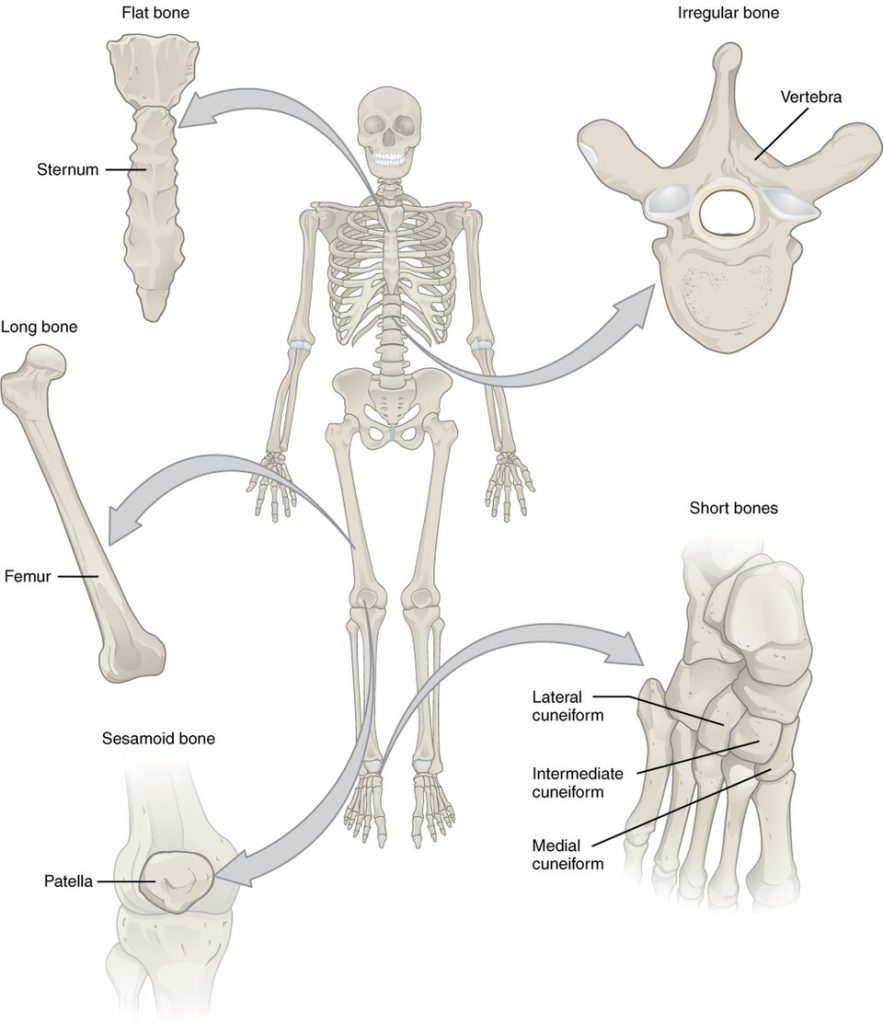
Table 6.3a reviews bone classifications with their associated features, functions, and examples.
Table 6.3a. Bone Classifications[3]
| Bone Classification | Features | Function(s) | Examples |
|---|---|---|---|
| Long | Cylinder-like shape; longer than it is wide | Leverage | Femur, tibia, fibula, metatarsals, humerus, ulna, radius, metacarpals, phalanges |
| Short | Cube-like shape approximately equal in length, width, and thickness | Provide stability and support while allowing for some motion | Carpals, tarsals |
| Flat | Thin and curved | Points of attachment for muscles; protectors of internal organs | Sternum, ribs, scapulae, cranial bones |
| Irregular | Complex shape | Protect internal organs | Vertebrae, facial bones |
| Sesamoid | Small and round; embedded in tendons | Protect tendons from compressive forces | Patellae |
Anatomy of a Long Bone
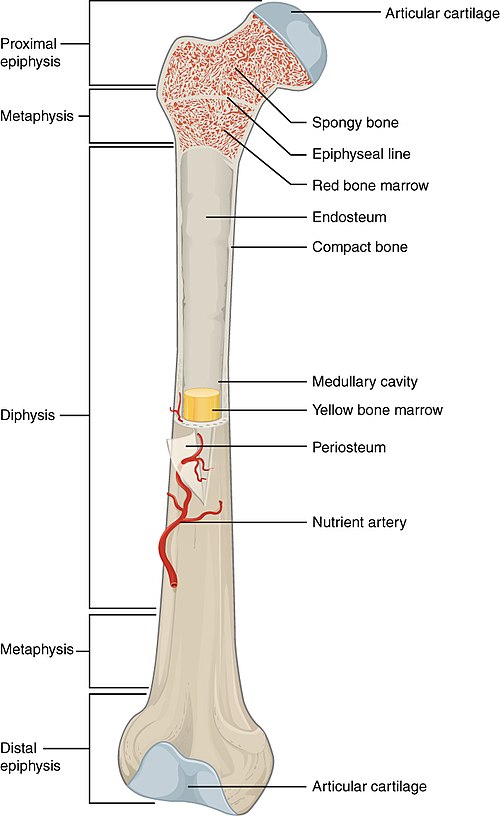
The structure of a long bone allows for the best visualization of all parts of a bone. See Figure 6.6[4] for an illustration of the anatomy of a long bone. Major parts of a long bone include the following:
- Diaphysis: The diaphysis is the shaft that runs between the proximal and distal ends of the bone. It is composed of compact or cortical bone tissue.
- Epiphysis: The epiphysis (plural = epiphyses) is the wider end of the bone and is made of spongy or cancellous bone tissue. Red marrow fills the spaces in the spongy bone.
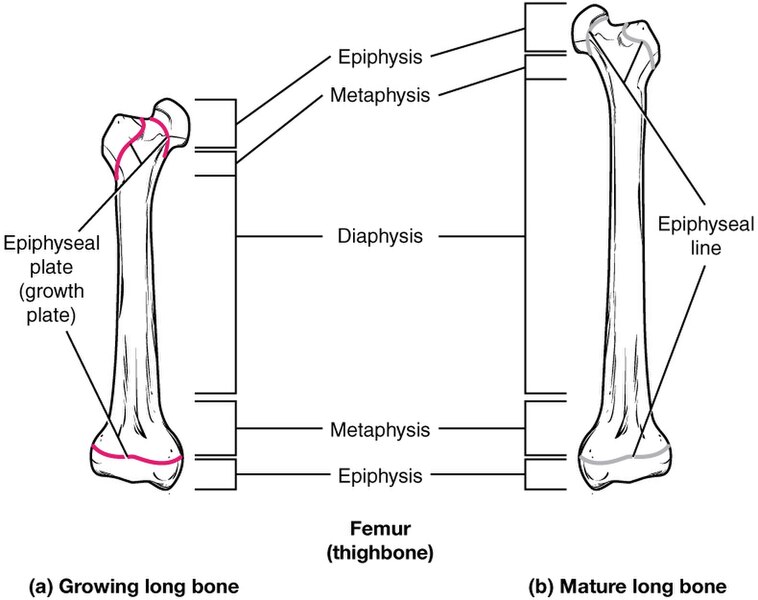
- Metaphysis: The epiphyses meet the diaphysis at the narrow area called the metaphysis. The metaphysis contains the epiphyseal plate (commonly referred to as the growth plate), a layer of hyaline cartilage in a growing bone. When the bone stops growing in early adulthood (at approximately 18–21 years of age), the hyaline cartilage is replaced by bone tissue and the epiphyseal plate becomes an epiphyseal line.
- Articular cartilage: The epiphyses are covered with articular cartilage, a thin layer of hyaline cartilage that reduces friction in joints and acts as a shock absorber.
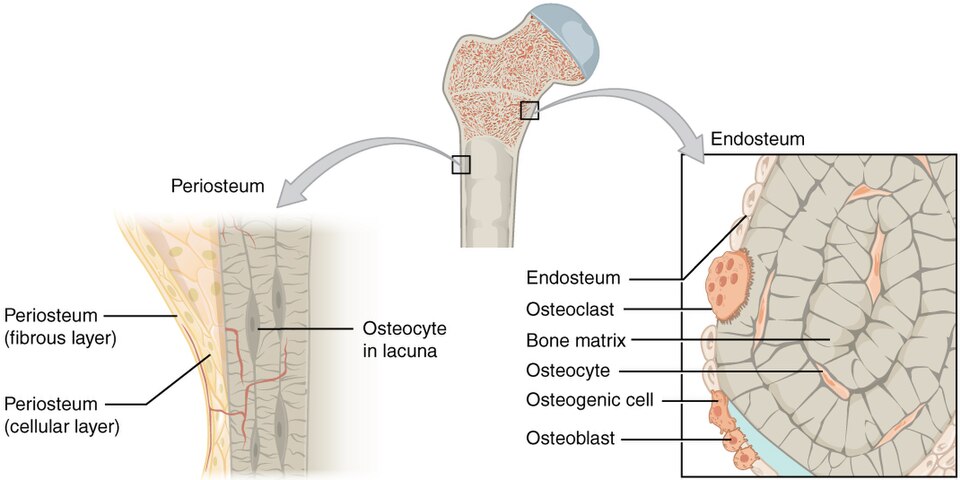
- Periosteum: The outer surface of the bone is covered with a fibrous membrane called the periosteum (peri- = “around” or “surrounding” and oste- = “bone”). The periosteum contains blood vessels, nerves, and lymphatic vessels that nourish compact bone. Tendons and ligaments also attach to bones at the periosteum. The periosteum covers the entire outer surface of the bone, except where the epiphyses meet other bones to form joints. See Figure 6.7[5] for an illustration of the periosteum.
- Medullary (or marrow) cavity: The hollow region in the diaphysis is called the medullary cavity, which is filled with red marrow in children and yellow marrow in adults.
- Endosteum: The endosteum (end- = “inside” and oste- = “bone”) is a delicate, membranous lining of the medullary cavity, where bone growth, repair, and remodeling occur. See Figure 6.7 for an illustration of the endosteum.
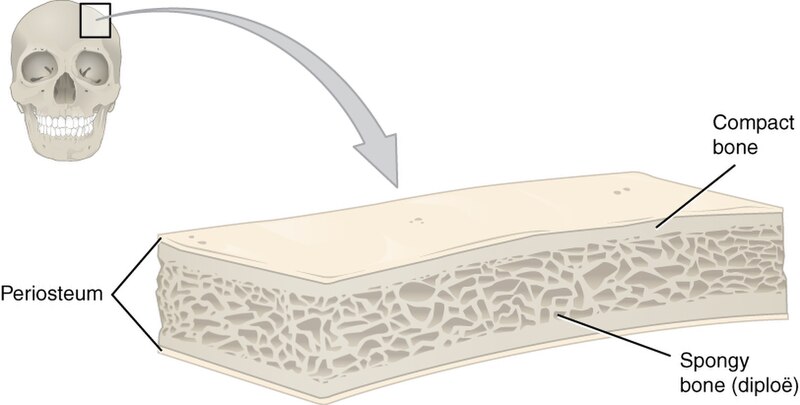
Anatomy of a Flat Bone
Flat bones, such as those of the skull, consist of an internal layer of spongy bone that is covered on either side by a layer of compact bone. The two layers of compact bone and the interior spongy bone work together to protect the internal organs. If the outer layer of a cranial bone fractures, the brain is still protected by the intact inner layer. Spongy and compact bone is further described below under the “Bone Tissue” subsection. See Figure 6.8[6] for an illustration of flat bones of the skull.
Bone Cells
Types of Bone Cells
Although bone cells make up a small amount of the bone volume, they are important to the function of bones. Four types of cells are found within bone tissue and include the following:
- Osteogenic cells: Osteogenic cells are stem cells with high mitotic activity, meaning they are the only bone cells that divide. Osteogenic cells are found in the deep layers of the periosteum and the marrow. Osteogenic cells differentiate and develop into osteoblasts.
- Osteoblasts: Osteoblasts continuously form new bone and are found primarily in the periosteum and endosteum. They make and secrete the collagen matrix of bone tissue. Calcium salts are deposited into this matrix to mineralize (harden) the bone. Osteoblasts do not divide.
- Osteocytes: An osteocyte is a mature bone cell responsible for maintaining bone tissue. It is the most common type of bone cell. Each osteocyte is located in a space called a lacuna (pleural = lacunae). Like osteoblasts, osteocytes lack mitotic activity. They communicate with each other and receive nutrients through canaliculi (singular = canaliculus), tiny channels within the bone matrix.
- Osteoclasts: Osteoclasts are responsible for bone resorption, or breakdown. They contain enzymes that dissolve bone. They are found on bone surfaces and are produced by bone marrow. The ongoing balance between osteoblasts and osteoclasts is responsible for the constant but subtle reshaping of bone.
See Figure 6.9[7] for an illustration of bone cells.
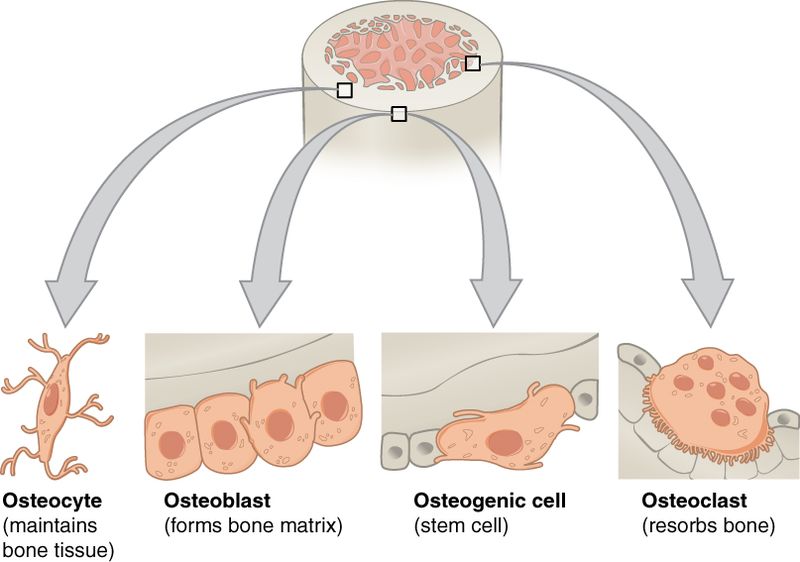
Table 63b summarizes the functions and locations of bone cells.
Table 6.3b. Functions and Locations of Bone Cells[8]
| Type of Bone Cell | Function | Location |
|---|---|---|
| Osteogenic Cells | Develop into osteoblasts | Deep layers of the periosteum and the marrow |
| Osteoblasts | Bone formation | Periosteum and endosteum |
| Osteocytes | Maintain bone tissue | Sit in lacunae within the matrix |
| Osteoclasts | Bone resorption | Bone surfaces and at sites of old, injured, or unneeded bone |
Bone Tissue
The difference between compact and spongy bone is best explored through their histology (tissues). Most bones contain both compact and spongy bone tissue, but their amounts vary based on the bone’s function. Compact bone is dense so that it can withstand weight and force, while spongy (cancellous) bone has open spaces and supports shifts in weight distribution.
Compact Bone
Compact bone is the denser, stronger of the two types of bone tissue. It can be found deep to the periosteum and in the diaphyses (shafts) of long bones, where it provides support and protection. See Figure 6.10[9] for an illustration of compact bone.
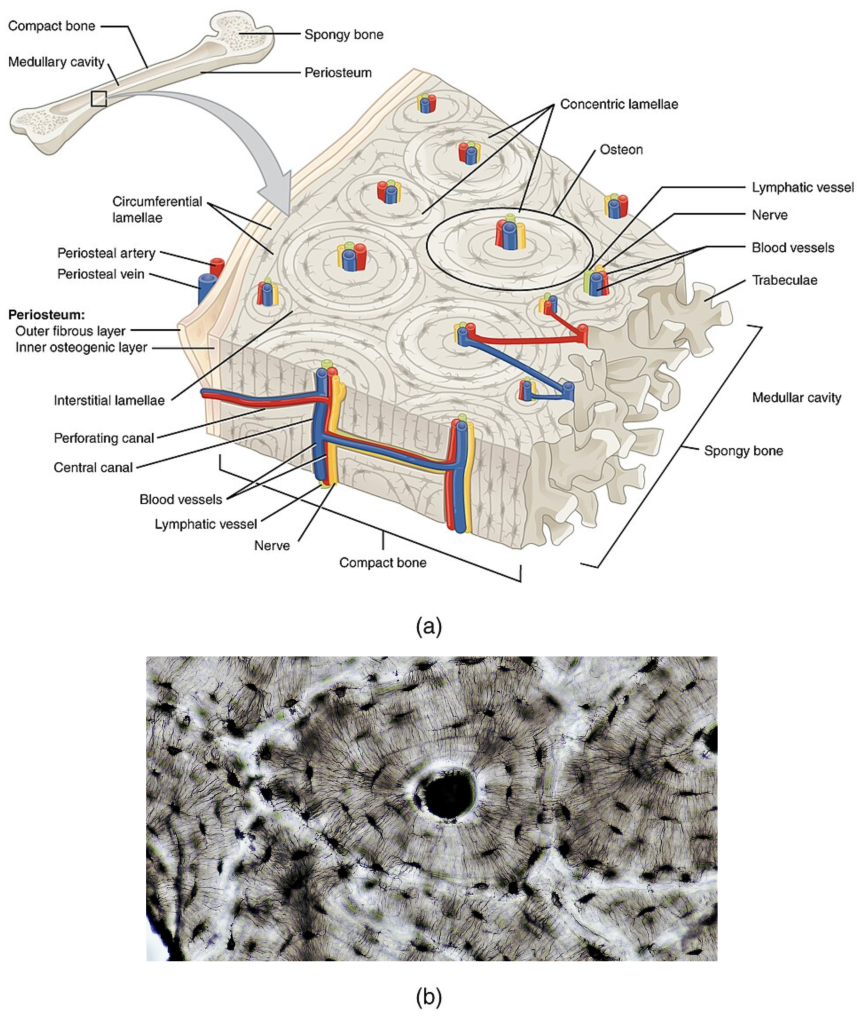
Osteon
The basic structural unit of compact bone is called an osteon, also called the Haversian system. Each osteon is composed of the following:
- Lamellae: Lamellae (singular = lamella) are circular/concentric rings of calcified matrix.
- Central Canal: The central canal (also called Havesian canal) is found in the center of each osteon. It contains blood vessels, nerves, and lymphatic vessels. These vessels and nerves branch off at right angles through a perforating canal (also called Volkmann’s canal) to extend to the periosteum and endosteum.
- Lacunae: Lacunae (singular = lacuna) are spaces that hold the osteocytes.
- Canaliculi: Canaliculi are tiny canals that connect lacunae with the central canal. The canaliculi transport nutrients from the central canal to the osteocytes and wastes from the osteocytes to the central canal.
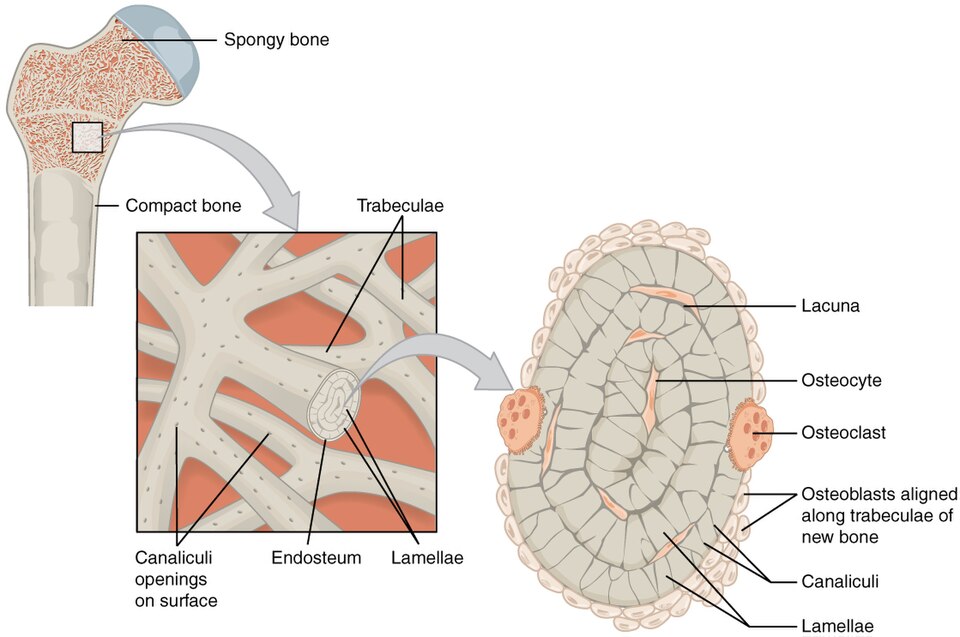
Spongy Bone
Like compact bone, spongy bone (also known as cancellous bone), contains osteocytes in lacunae, but they are not arranged in osteons. Instead, the lacunae and osteocytes are found in a lattice-like network of matrix called trabeculae (singular = trabecula). Each trabecula forms along lines of stress to provide strength to the bone. The spaces make bones lighter so muscles can move them easily. In addition, the spaces in spongy bone contain red marrow where blood cell formation occurs. See Figure 6.11[10] for an illustration of spongy bone.
Bone Formation
In the early stages of embryonic development, the embryo’s skeleton is made up of fibrous membranes and hyaline cartilage. By the sixth or seventh week of embryonic life, the process of actual bone development called ossification (or osteogenesis) begins. There are two bone development pathways called intramembranous ossification and endochondral ossification.
Intramembranous Ossification
During intramembranous ossification, compact and spongy bone develop directly from sheets of mesenchymal (undifferentiated) connective tissue. Examples of bones formed by intramembranous ossification are the flat bones of the face, most of the cranial bones, and the clavicles.
There are four steps in intramembranous ossification that include the following:
- Mesenchymal (undifferentiated) cells in the embryonic skeleton clump together and begin to differentiate into specialized cells. Some cells differentiate into capillaries, while others become osteogenic cells that turn into osteoblasts.
- The osteoblasts secrete osteoid, an uncalcified bone matrix, which calcifies (hardens) within a few days as mineral salts are deposited in it. The calcified matrix traps osteoblasts within it. Once trapped, the osteoblasts become osteocytes.
- Osteoid is secreted around the capillaries and forms spongy bone trabeculae while mesenchymal cells on the surface of the spongy bone form the periosteum.
- The periosteum forms a protective layer of compact bone around the trabecular bone. Blood vessels in the spongy bone condense to form red marrow.
See Figure 6.12[11] for an illustration of these steps of intramembranous ossification.
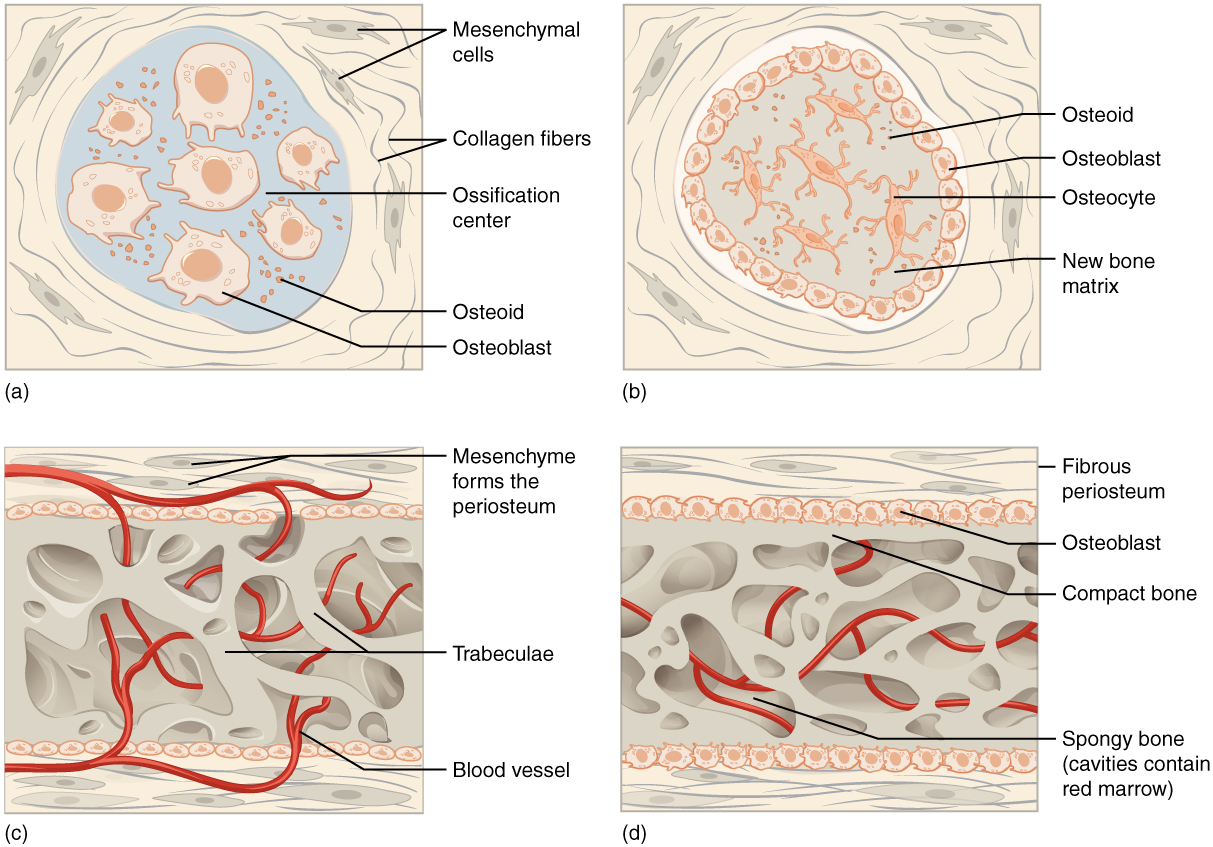
Intramembranous ossification begins during fetal development in the uterus and continues into adolescence. At birth, the skull and clavicles are not fully ossified yet. This allows the skull and shoulders to deform during passage through the birth canal. The last bones to ossify by intramembranous ossification are the flat bones of the face, which reach their adult size at the end of the adolescent growth spurt.
Endochondral Ossification
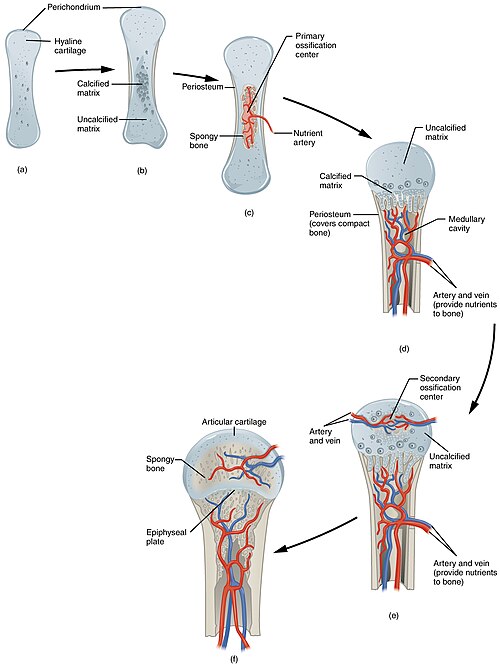
During endochondral ossification, bone develops by replacing hyaline cartilage. The cartilage serves as a template that will be completely replaced by new bone. Endochondral ossification takes much longer than intramembranous ossification. Most bones of the body are formed by endochondral ossification.
Steps of endochondral ossification include the following:
- Mesenchymal cells differentiate into chondroblasts (cartilage-forming cells). Chondroblasts form a hyaline cartilage model in the shape of the future bone. The perichondrium, a membrane that surrounds the cartilage model, also forms.
- The cartilage calcifies.
- Blood vessels grow into the calcified cartilage of the diaphysis that stimulates osteoblasts to form spongy bone in the primary ossification center (first place bone develops). The perichondrium becomes the periosteum at this point.
- A medullary cavity is formed. Eventually, the spongy bone of the diaphysis will be turned into compact bone.
- Around birth, the secondary ossification centers (second place bone is formed) develop in the epiphyses of the bone. The process is similar where an artery grows into the calcified cartilage and stimulates osteoblasts to form spongy bone. Unlike the diaphysis, the epiphyses will remain spongy bone, and no medullary cavity is formed.
- Cartilage remains in the epiphyseal (growth) plate and on the epiphysis surface as articular (joint) cartilage.
See Figure 6.13[12] for an illustration of endochondral ossification.
Bone Growth and Remodeling
Bones grow and repair themselves through interstitial growth, appositional growth, and bone remodeling.
Interstitial Growth
Interstitial growth refers to longitudinal bone growth (lengthening of the bone). The epiphyseal plate (growth plate) is an area of hyaline cartilage where growth occurs in immature long bones until early adulthood. During interstitial growth, the epiphyseal (end) side of the epiphyseal plate forms cartilage, and on the diaphyseal side, the cartilage is ossified, causing the diaphysis (shaft) to grow in length.
The epiphyseal plate has four zones of cells and activity including the following:
- The reserve zone is the region closest to the epiphyseal end of the plate and contains small chondrocytes (cartilage cells) within the matrix. These chondrocytes do not participate in bone growth but attach the epiphyseal plate to the epiphysis.
- The proliferative zone is the next layer and contains stacks of slightly larger chondrocytes. It makes new chondrocytes via mitosis to replace those that die at the diaphyseal end of the plate.
- Chondrocytes in the next layer, the zone of maturation and hypertrophy, are older and larger than those in the proliferative zone. The more mature cells are located closer to the diaphyseal end of the plate. The longitudinal growth of bone is a result of cell division in the proliferative zone and the maturing of cells in the zone of maturation and hypertrophy that will be converted to bone.
- Most of the chondrocytes in the zone of calcified matrix, the zone closest to the diaphysis, are dead because the matrix around them has calcified. Capillaries and osteoblasts from the diaphysis enter this zone, and the osteoblasts secrete bone matrix in the remaining calcified cartilage. Thus, the zone of calcified matrix connects the epiphyseal plate to the diaphysis. A bone grows in length when bone tissue is added to the diaphysis.
See Figure 6.14[13] for an illustration of long bone growth by interstitial growth.
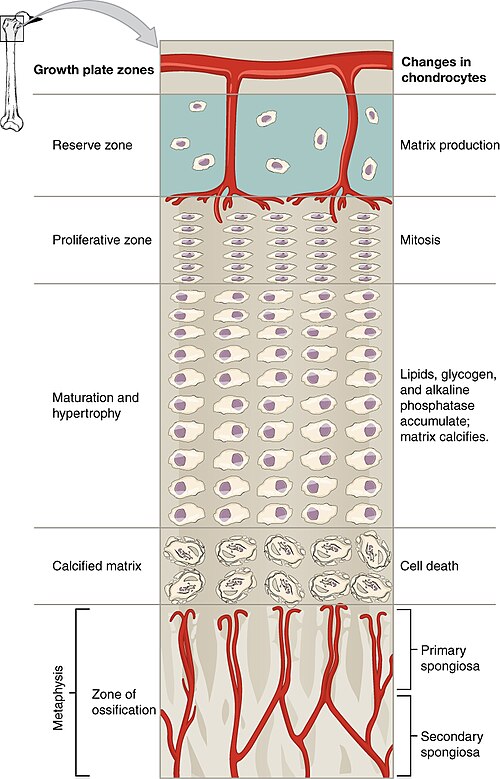
Bones continue to grow in length until early adulthood. The rate of growth is controlled by hormones. When the chondrocytes in the epiphyseal plate stop dividing and bone replaces the cartilage, longitudinal growth stops. All that remains of the epiphyseal plate is the epiphyseal line. See Figure 6.15[14] for an illustration of progression from the epiphyseal plate to the epiphyseal line.
See Figure 6.16[15] for a radiographic image of bone plates.

View a supplementary YouTube video[16] on bone growth from the BBC: The Secret Behind Long Bone Growth – The Human Body: Secrets of Your Life Revealed – Grow – BBC.
Appositional Growth
While bones are increasing in length, they are also increasing in diameter, called appositional growth. Growth in diameter can continue even after longitudinal growth stops. Osteoclasts resorb old bone that lines the medullary cavity, while osteoblasts produce new bone tissue deep to the periosteum. The erosion of old bone along the medullary cavity and the deposition of new bone beneath the periosteum increase the diameter of the diaphysis and also increase the diameter of the medullary cavity. This process is called modeling.
Bone Remodeling
Bone remodeling is the resorption of old or damaged bone while osteoblasts lay new bone to replace it. Injury, exercise, and other activities lead to remodeling, but even without injury or exercise, about 5 to 10 percent of the skeleton is remodeled annually just by destroying old bone and replacing it with fresh bone.
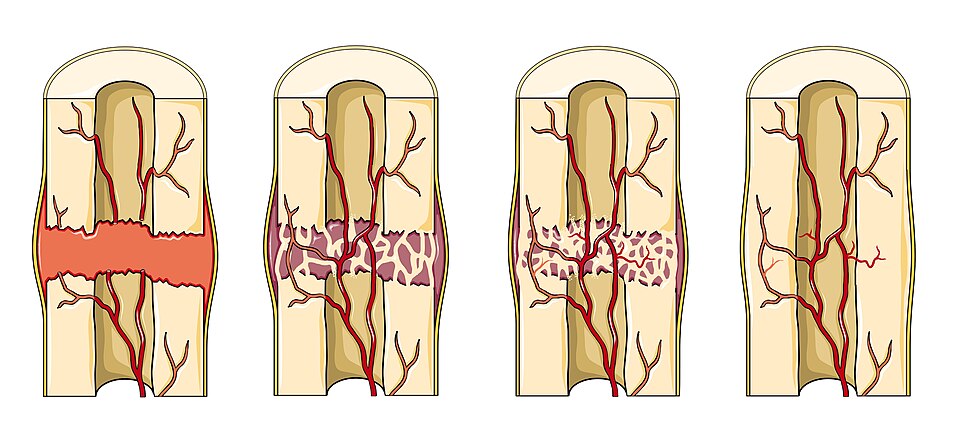
Fractures and Fracture Repair
A fracture is a broken bone. While some fractures are minor, others can be severe and result in complications. For example, a fractured diaphysis of the femur has the potential to release fat globules into the bloodstream. These can become lodged in the capillary beds of the lungs, leading to respiratory distress and, if not treated quickly, result in death.
There are four stages of fracture repair that include the following:
- Formation of a fracture hematoma: When a bone breaks, bleeding occurs from vessels torn by the fracture. These vessels can be in the periosteum, osteons, and/or medullary cavity. The blood begins to clot, and about six to eight hours after the fracture, the clotted blood forms a fracture hematoma. The interruption of blood flow to the bone results in the death of bone cells around the fracture.
- Formation of a fibrocartilaginous (soft) callus. Over the next two to three weeks, chondrocytes from the endosteum form fibrocartilage between the two ends of the broken bone.
- Formation of a bony (hard) callus. Over the next three to four months, osteoclasts resorb the dead bone. Osteogenic cells become active, divide, and differentiate into osteoblasts. The cartilage in the callus is replaced by spongy bone formed by endochondral ossification.
- Remodeling. Compact bone replaces the spongy bone at the outer margins of the fracture, and healing is complete. A slight swelling may remain on the surface of the bone, which may be visible on an X-ray, but typically there is no external evidence of the fracture.
See Figure 6.17[17] for an illustration of the stages of fracture repair.
Types of Fractures
Fractures can be classified in many ways, including by their complexity and location. See Figure 6.18[18] for an illustration of types of fractures.
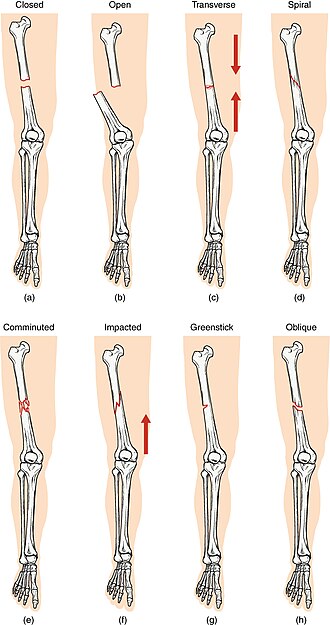
Table 6.3c outlines common types of fractures. A fracture may be described by using more than one term because it may have the features of more than one type. For example, an open transverse fracture refers to a fracture that occurs across the axis of a long bone where at least one end of the bone is also protruding from the skin.
Table 6.3c. Types of Fractures[19]
| Type of Fracture | Description |
|---|---|
| Transverse | Occurs straight across the long axis of the bone |
| Oblique | Occurs at an angle that is not 90 degrees |
| Spiral | Bone segments are pulled apart as a result of a twisting motion |
| Comminuted | Several breaks result in many small pieces between two large segments |
| Impacted | One fragment is driven into the other, usually as a result of compression |
| Greenstick | A partial fracture in which only one side of the bone is broken; common in children |
| Open (or compound) | A fracture in which at least one end of the broken bone tears through the skin; carries a high risk of infection |
| Closed (or simple) | A fracture that does not break the skin |
Hormones of the Skeletal System
Bones contain more calcium than any other organ. When blood calcium levels decrease below normal levels, calcium is released from the bones by the osteoclasts so there is an adequate supply for the body’s physiological needs. In contrast, when blood calcium levels are increased, excess calcium is stored in bone by the osteoblasts. This dynamic process of releasing and storing calcium goes on continuously.
Two hormones that maintain calcium homeostasis are parathyroid hormone (PTH) and calcitonin.
- Parathyroid Hormone (PTH): PTH is secreted by the parathyroid glands to stimulate osteoclast activity. As a result, bone is broken down and calcium is released from the bones into the blood, thus increasing blood calcium level.
- Calcitonin: Calcitonin is secreted by the thyroid gland to inhibit osteoclast activity and stimulate calcium storage in the bones, thus lowering blood calcium level.
Because of their opposing functions in maintaining calcium homeostasis, PTH and calcitonin are generally not secreted at the same time. Table 6.3d summarizes other hormones that also influence the skeletal system.
Table 6.3d. Hormones That Affect the Skeletal System[20]
| Hormone | Role |
|---|---|
| Human Growth Hormone and Insulin-like Growth Factors (IGF) | Increases the length of long bones (interstitial growth), enhances mineralization, and improves bone density |
| Thyroxine | Stimulates bone growth and promotes production of bone matrix |
| Sex Hormones (Estrogen and Testosterone) | Promote osteoblastic activity and production of bone matrix; responsible for adolescent growth spurt; close the epiphyseal plate (growth plate) at the end of adolescence |
| Calcitriol | Stimulates absorption of calcium and phosphate from digestive tract |
| Parathyroid Hormone | Stimulates osteoclast activity to release calcium from the bones to increase blood calcium level |
| Calcitonin | Inhibits osteoclast activity and stimulates calcium storage by bones to lower blood calcium level |
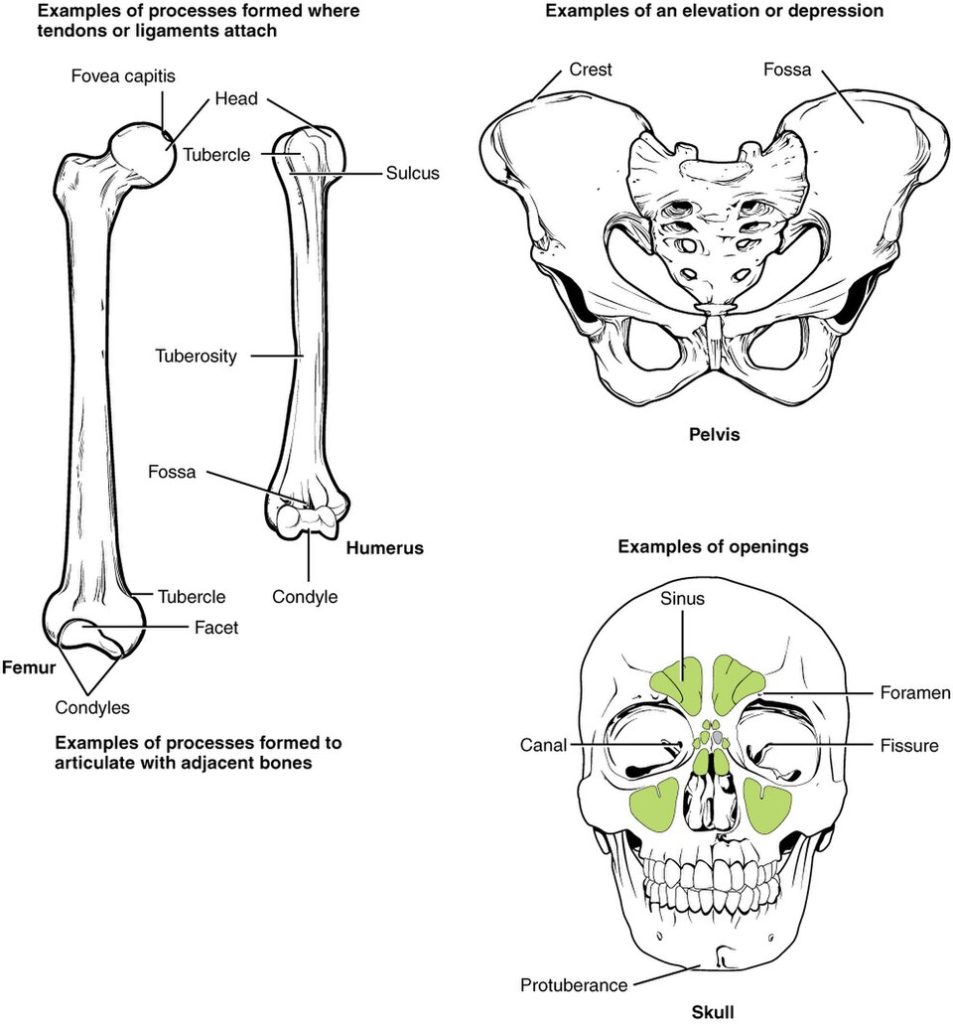
Bone Markings
The surface features of bones vary considerably, depending on the function and location in the body. There are several classes of bone markings including the following:
- Projections: A projection is an area of a bone that projects above the surface of the bone. These are the attachment points for tendons and ligaments.
- Holes: A hole is an opening or groove in the bone that allows blood vessels and nerves to enter the bone. As with the other markings, their size and shape reflect the size of the vessels and nerves that penetrate the bone at these points.
Table 6.3e describes various bone markings, which are also illustrated in Figure 6.19.[21]
Table 6.3e. Bone Markings[22]
| Marking | Description | Example |
|---|---|---|
| Head | Prominent rounded surface | Head of femur |
| Facet | Flat surface | Vertebrae |
| Condyle | Rounded surface | Occipital condyles |
| Protuberance | Protruding | Chin |
| Process | Prominence feature | Transverse process of vertebra |
| Spine | Sharp process | Ischial spine |
| Tubercle | Small, rounded process | Tubercle of humerus |
| Tuberosity | Rough surface | Deltoid tuberosity |
| Line | Slight, elongated ridge | Temporal lines of the parietal bones |
| Crest | Ridge | Iliac crest |
| Fossa | Elongated basin | Mandibular fossa |
| Fovea | Small pit | Fovea capitis on the head of the femur |
| Sulcus | Groove | Sigmoid sulcus of the temporal bones |
| Canal | Passage in bone | Auditory canal |
| Fissure | Slit through bone | Auricular fissure |
| Foramen | Hole in bone | Foramen magnum in the occipital bone |
| Meatus | Opening into canal | External auditory meatus |
| Sinus | Air-filled space in bone | Nasal sinus |
Divisions of the Skeletal System
The skeleton is subdivided into two major divisions called the axial skeleton and appendicular skeleton. The axial skeleton serves to protect the brain, spinal cord, heart, and lungs and also serves as the attachment site for muscles that move the head, neck, and back. It consists of 80 bones, including all bones of the skull, the vertebral column, and the thoracic cage (chest):
- The skull is formed by 22 bones. Also associated with the skull are an additional seven bones, including the hyoid bone and the ear ossicles (three small bones found in each middle ear).
- The vertebral column consists of 24 bones, each called a vertebra, plus the sacrum and coccyx.
- The thoracic cage includes the 12 pairs of ribs and the sternum (the flattened bone of the anterior chest).
The appendicular skeleton includes all bones of the upper and lower limbs, plus the bones that attach each limb to the axial skeleton. There are 126 bones in the appendicular skeleton of an adult. See Figure 6.20[23] for an illustration of the axial and appendicular skeleton.
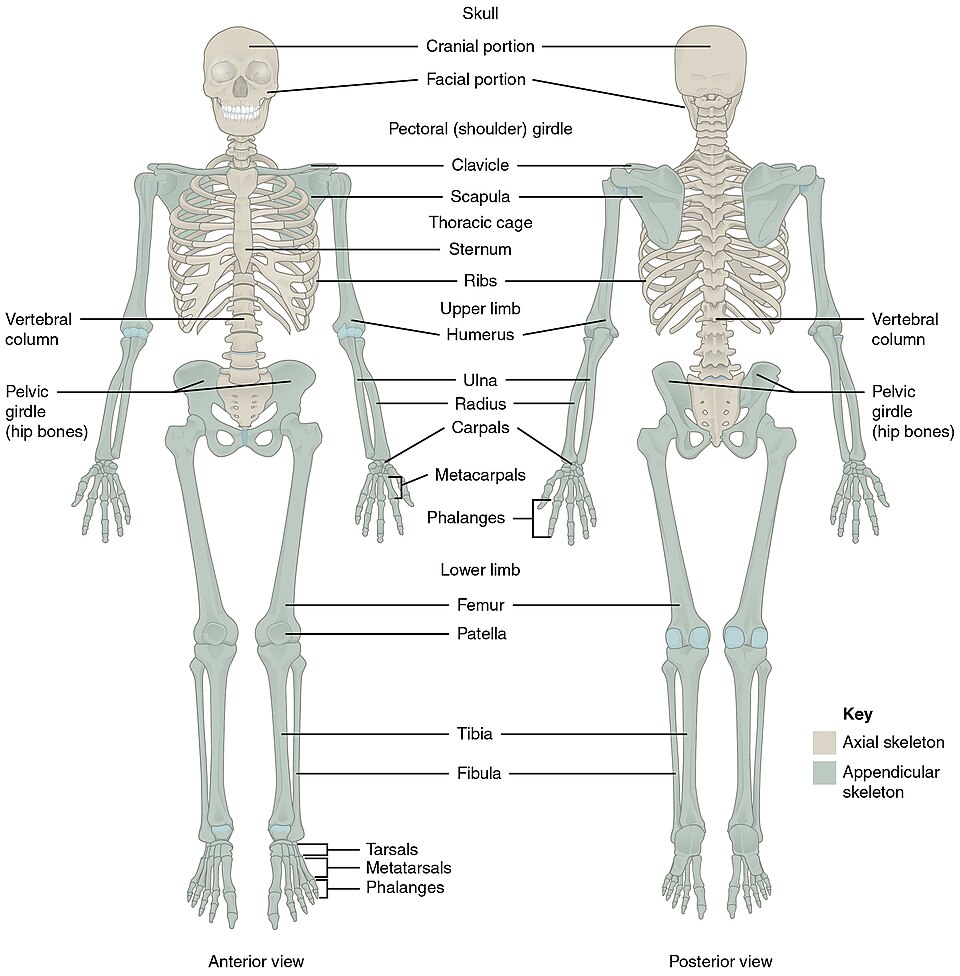
The following sections will discuss bones of the axial skeleton and the appendicular skeleton in greater detail.
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- “601_Bone_Classification” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Desaix, P., Johnson, E., Johnson, J. E., Korol, O., Kruse, D., Poe, B., Wise, J., Womble, M. D., & Young, K. A. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “603_Anatomy_of_Long_Bone” by OpenStax College is licensed under CC BY 3.0 ↵
- “607_Periosteum_and_Endosteum” by OpenStax College is licensed under CC BY 3.0 ↵
- “621_Anatomy_of_a_Flat_Bone” by OpenStax College is licensed under CC BY 3.0 ↵
- “604_Bone_cells” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Desaix, P., Johnson, E., Johnson, J. E., Korol, O., Kruse, D., Poe, B., Wise, J., Womble, M. D., & Young, K. A. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- This image is a modification of “624_Diagram_of_Compact_Bone-new” by OpenStax College, licensed under CC BY 3.0 and “Connective_Tissue_Compact_Bone_(41068142774)” by Berkshire Community College Bioscience Image Library, licensed under CC0, Public Domain. ↵
- “606_Spongy_Bone” by OpenStax College is licensed under CC BY 3.0 ↵
- “adc7826f821d921d2b47a768327e1204b1a47dc7” by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology-2e/pages/6-4-bone-formation-and-development#fig-ch06_04_01 ↵
- “608_Endochrondal_Ossification.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- “622_Longitudinal_Bone_Growth” by OpenStax College is licensed under CC BY 3.0 ↵
- “623_Epiphyseal_Plate-Line” by OpenStax College is licensed under CC BY 3.0 ↵
- “Tib_fib_growth_plates” by Gilo1969 is licensed under CC BY 3.0 ↵
- BBC. (2017, October 5). The secret behind long bone growth - The human body: Secrets of your life revealed - Grow - BBC [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=r1wyy_3_4mk ↵
- “Fracture_repair_--_Smart-Servier_(cropped)" by Laboratoires Servier is licensed under CC BY-SA 3.0 ↵
- “612_Types_of_Fractures” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Desaix, P., Johnson, E., Johnson, J. E., Korol, O., Kruse, D., Poe, B., Wise, J., Womble, M. D., & Young, K. A. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Desaix, P., Johnson, E., Johnson, J. E., Korol, O., Kruse, D., Poe, B., Wise, J., Womble, M. D., & Young, K. A. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “602_Bone_Markings” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Desaix, P., Johnson, E., Johnson, J. E., Korol, O., Kruse, D., Poe, B., Wise, J., Womble, M. D., & Young, K. A. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “701_Axial_Skeleton-01” by OpenStax College is licensed under CC BY 3.0 ↵
To grow together.
The total amount of bone tissue a person.
Cylindrical in shape and longer than wide, these bones are found in the arms (humerus, ulna, and radius), legs (femur, tibia, and fibula), fingers (metacarpals and phalanges), and toes (metatarsals and phalanges). They function as levers that move when muscles contract.
Cube-like in shape, with nearly equal length, width, and thickness. In the human body, the only short bones are found in the wrists (carpals) and ankles (tarsals). These bones are designed to provide stability and support while allowing for limited motion.
These bones are typically thin and often curved. They include the cranial bones, scapulae (shoulder blades), sternum (breastbone), and ribs. They provide protection for internal organs and serve as important attachment points for muscles.
With complex shapes that don’t fit into other bone classifications, these bones include structures like the vertebrae, which protect the spinal cord, and many of the bones in the face.
A small, round bone shaped like a sesame seed. These bones develop within tendons and serve to protect the tendon and increase its mechanical efficiency.
The shaft that runs between the proximal and distal ends of the bone.
The wider end of the bone and is made of spongy or cancellous bone tissue.
The narrow region of a long bone where the epiphysis (end) meets the diaphysis (shaft).
The remnant of the epiphyseal plate (growth plate) found in adult bones. It appears as a thin, solid line of bone where the cartilage used to be and marks the point where the bone has stopped growing in length after puberty.
A thin layer of hyaline cartilage that reduces friction in joints and acts as a shock absorber.
The fibrous layer covering the outer surface of the bone.
The hollow region in the diaphysis.
A delicate, membranous lining of the medullary cavity, where bone growth, repair, and remodeling occur.
These are bone stem cells with the unique ability to divide through mitosis. Found in the deep layers of the periosteum and within the bone marrow, they serve as the origin for other bone cells by developing into osteoblasts, which are responsible for forming new bone tissue.
These are bone-forming cells found mainly in the periosteum and endosteum. They produce and secrete the collagen matrix that provides structure to bone tissue. Calcium salts are later deposited into this matrix, causing the bone to harden. Unlike some other bone cells, they do not divide.
A mature bone cell responsible for maintaining bone tissue.
These are tiny, hair-like canals that connect the lacunae (spaces housing osteocytes) to the central canal in compact bone. They facilitate the transport of nutrients from the central canal to the osteocytes and remove waste products from the osteocytes back to the central canal.
These are large, bone-breaking cells responsible for the breakdown and resorption of bone tissue. Found on bone surfaces, they dissolve the mineral matrix and collagen, helping to shape bones during growth, repair damage, and regulate calcium levels in the blood. Unlike osteoblasts, they break down bone rather than build it.
Dense, hard bone tissue that provides strength and support, also known as cortical bone.
Basic structural unit of compact bone.
Circular/concentric rings of calcified matrix.
Located at the center of each osteon in compact bone, this channel houses blood vessels, nerves, and lymphatic vessels. It allows for the nourishment and communication of bone cells throughout the tissue.
These are channels that run perpendicular to the central canals (Haversian canals) in compact bone. They allow blood vessels, nerves, and lymphatic vessels to extend from the central canals to the periosteum and endosteum, ensuring the bone tissue receives adequate nutrients and communication. Also known as the Volmann’s canal.
Spaces that hold the osteocytes.
Porous bone tissue that provides structural support and houses bone marrow, also known as cancellous bone.
A light, porous type of bone tissue found primarily at the ends of long bones and within the vertebrae, also known as spongy bone.
Small, beam-like structures in bone and other tissues that create a supportive network.
Process of actual bone development.
This is a process of bone formation in which compact and spongy bone develop directly from sheets of mesenchymal (undifferentiated) connective tissue.
An uncalcified bone matrix.
This is the process of bone development in which hyaline cartilage is gradually replaced by bone tissue. The cartilage acts as a template that is eventually replaced by new bone.
Cartilage-forming cells.
A membrane that surrounds the cartilage model.
This is the region in a developing long bone where bone formation begins during endochondral ossification.
This is the area in a developing long bone where bone formation begins after the primary ossification center. It typically appears in the epiphyses (ends) of the bone, where cartilage remains in the form of articular cartilage and the epiphyseal plate (growth plate).
Refers to longitudinal bone growth (lengthening of the bone).
The region closest to the epiphyseal end of the plate and contains small chondrocytes (cartilage cells) within the matrix.
This is the second layer of the epiphyseal plate, located just below the zone of reserve cartilage. It contains stacks of slightly larger chondrocytes that actively divide through mitosis.
This layer of the epiphyseal plate contains older chondrocytes that have stopped dividing and begin to enlarge (hypertrophy). The lacunae surrounding them also expand, creating spaces that will later become part of the bone’s structure. This zone contributes to the lengthening of the bone as the cells grow in size.
This layer of the epiphyseal plate contains chondrocytes that are dying or already dead, as the surrounding matrix becomes calcified. Calcium salts are deposited in the matrix, hardening it and preparing it for the arrival of bone-forming cells. This zone acts as the transition between cartilage and new bone tissue.
The is the process by which bones grow in width or diameter.
The process in which old bone is eroded from the inner surface (along the medullary cavity) while new bone is deposited beneath the periosteum.
The resorption of old or damaged bone while osteoblasts lay new bone to replace it.
A broken bone.
This is the mass of clotted blood that forms at the site of a bone fracture, typically within six to eight hours after the injury. It results from blood vessel damage and serves as the first step in the bone healing process, helping to stabilize the break and initiate tissue repair.
Fracture that occurs straight across the long axis of the bone.
A term describing muscles with fibers that run at an angle to the midline of the body, such as the abdominal oblique muscles.
Fracture in which bone segments are pulled apart as a result of a twisting motion.
Several breaks result in many small pieces between two large segments.
Fracture in which one fragment is driven into the other, usually as a result of compression.
A partial fracture in which only one side of the bone is broken, common in children
A fracture in which at least one end of the broken bone tears through the skin; carries a high risk of infection.
A fracture that does not break the skin.
An area of a bone that projects above the surface of the bone.
An opening or groove in the bone that allows blood vessels and nerves to enter the bone.
Serves to protect the brain, spinal cord, heart, and lungs and also serves as the attachment site for muscles that move the head, neck, and back.
All bones of the upper and lower limbs, plus the bones that attach each limb to the axial skeleton.

