5.5 Skin Disorders
Skin Disorders[1]
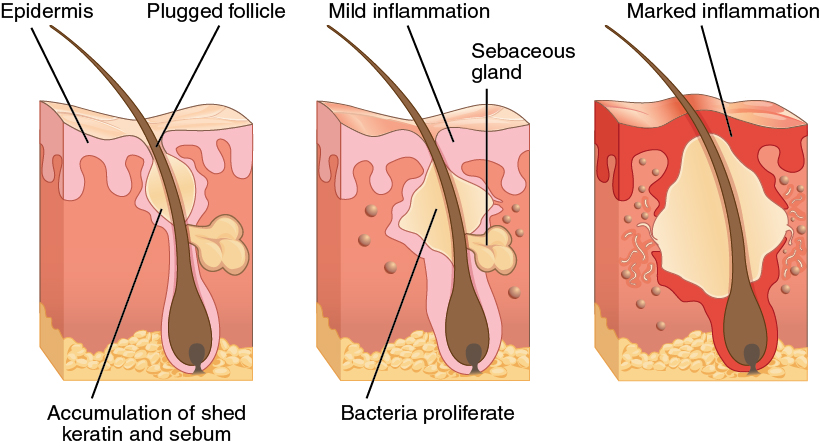
Acne
Acne is a skin condition that typically occurs on the face and back, which are areas rich in sebaceous (oil) glands. It is most common at the onset of puberty due to hormonal changes but can also occur in infants and continue into adulthood. See Figure 5.12[2] for an illustration of acne.
Albinism
Albinism is a genetic disorder that completely or partially affects the color of the skin, hair, and eyes due to the inability of melanocytes to produce melanin. This lack of melanin causes skin and hair to appear white or very pale. Individuals with albinism need more protection from UV radiation, as they are more prone to sunburns and skin cancer. They also tend to be more sensitive to light and may have vision problems due to the lack of pigmentation in the retina. Treatment of this disorder usually involves limiting UV exposure to the skin and eyes. See Figure 5.13[3] for an image of an infant with albinism.

Alopecia
Alopecia is the medical term for hair loss in areas where hair normally grows. See Figure 5.14[4] for an image of alopecia.

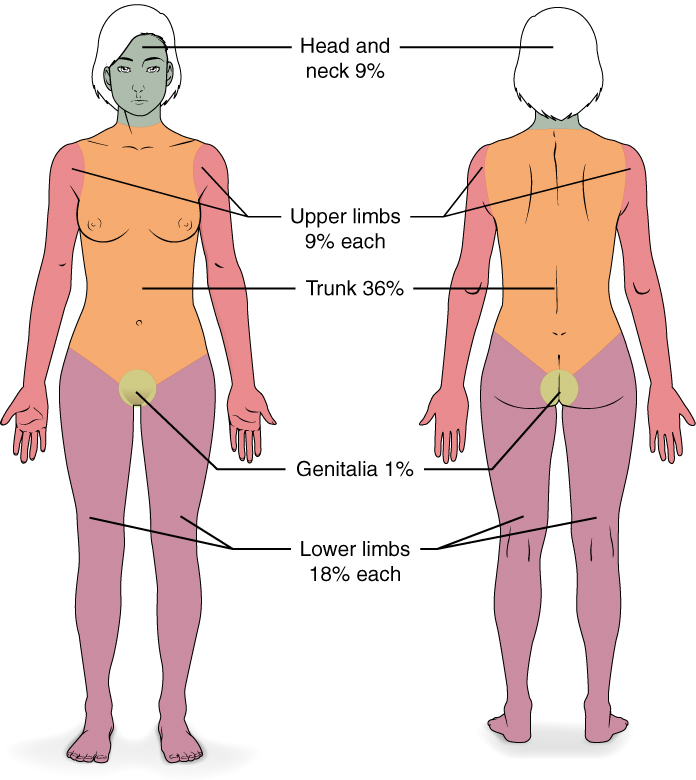
Burns
A burn is skin damage caused by intense heat, radiation, electricity, or chemicals. Burns can result in the death of skin cells, and large burns result in massive fluid loss that can result in dehydration, infection, electrolyte imbalance, and renal and circulatory failure that can be fatal.
Patients with severe burns are treated with intravenous fluids to offset dehydration, as well as intravenous nutrients that enable the body to repair tissues and replace lost proteins. Another serious threat to burn patients is infection. Burned skin is extremely susceptible to bacteria and other pathogens, due to the loss of protection by intact layers of skin.
Burns can be measured in terms of the total surface area affected. This is referred to as the “rule of nines,” which gives specific anatomical areas a percentage that is a factor of nine. See Figure 5.15[5] for an illustration of the rule of nines.
Burns are also classified by the degree of their severity using the guidelines described in the following subsections. See Figure 5.16[6] for illustrations of first-degree, second-degree, and third-degree burns.
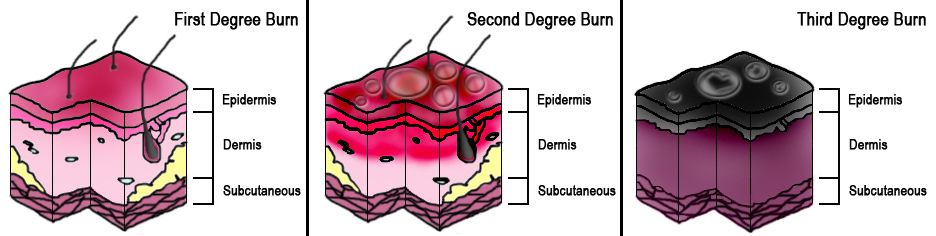
First-Degree Burn
A first-degree burn is a superficial burn that affects only the epidermis. Although the skin may be red, painful, and swollen, these burns typically heal on their own within a few days. A mild sunburn is an example of a first-degree burn. See Figure 5.17[7] for an image of a first-degree burn.

Second-Degree Burn
A second-degree burn, referred to as a partial thickness burn, affects both the epidermis and a portion of the dermis. These burns result in redness, swelling, and a painful blistering of the skin. It is important to keep the burn site clean to prevent infection. Second-degree burns will usually heal within several weeks. See Figure 5.18[8] for an image of a second-degree burn.

Third-Degree and Fourth-Degree Burns
Third-degree burns are referred to as full thickness burns and extend fully into the epidermis, dermis, and hypodermis, destroying the tissue and affecting the nerve endings and sensory function. These are serious burns requiring medical attention that may appear white, red, or black. They are usually not as painful as second-degree burns because the nerve endings are damaged. See Figure 5.19[9] for an image of a third-degree burn.

A fourth-degree burn is even more severe, affecting the underlying muscle and bone. See Figure 5.20[10] for an image of severe fourth-degree electrical burn.

Full-thickness burns cannot be repaired by the body because the local tissues used for repair are damaged. They often require debridement, or amputation in severe cases, followed by grafting of the skin from an unaffected part of the body or from skin grown in tissue culture.
Callus
A callus is a thickened area of the epidermis due to constant rubbing or abrasion. The stem cells in the stratum basale are stimulated to increase the thickness of the skin to protect it from further damage. See Figure 5.21[11] for an image of calluses on a person’s plantar surface of their right foot and medial surface of their left foot.

A corn is a specialized form of a callus formed by abrasions on the skin that result from an elliptical-type motion. They’re usually found on the feet.
Dandruff
Dandruff is a condition of flakes of dead skin from the scalp. See Figure 5.22[12] for an image of dandruff.
Eczema
Eczema is an allergic reaction that appears as dry, itchy patches of skin resembling rashes. Eczema may be accompanied by swelling of the skin, flaking, and in severe cases, bleeding. See Figure 5.23[13] for an illustration of eczema.

Freckles
Freckles are patches of melanin determined by genetics. See Figure 5.24[14] for an image of an individual with freckles.

Fungal Infections
Tinea is the name of a group of skin diseases caused by a fungus. Types of tinea include ringworm, athlete’s foot, and jock itch. These infections are usually not serious, but they can be uncomfortable because of the symptoms of itching and burning. They can be transmitted by touching infected people, damp surfaces such as shower floors, or even from pets. Ringworm (tinea corporis) is a type of rash that forms on the body that typically looks like a red ring with a clear center, although a worm doesn’t cause it. Scalp ringworm (tinea capitis) causes itchy, red patches on the head that can leave bald spots. Athlete’s foot (tinea pedis) causes itching, burning, and cracked skin between the toes. Jock itch (tinea cruris) causes an itchy, burning rash in the groin area. Fungal infections are often treated successfully with over-the-counter creams and powders, but some require prescription medicine such as nystatin. See Figure 5.25[15] for an image of tinea pedis (athlete’s foot).

Hirsutism
Hirsutism is the medical term for excessive hair growth in areas where hair is usually minimal or absent. See Figure 5.26[16] for an image of hirsutism in a female.

Hives
Hives (also known as urticaria) are circular, fluid-filled, itchy, raised lesions, often due to an allergic reaction. See Figure 5.27[17] for an image of hives.

Hyperhidrosis
Hyperhidrosis is a medical condition of excessive sweating that is not related to heat or exercise. It is treated with medications, Botox injections, or surgery. See Figure 5.28[18] for an image depicting hyperhidrosis.

Keloid
A keloid is a raised bump due to an overproduction of scar tissue. See Figure 5.29[19] for an image of post-surgical keloids.

Laceration
A laceration is an irregular tear or cut of the skin that may require suturing or other type of surgical repair. See Figure 5.30[20] for an image of a laceration before and after it was sutured.

Moles
Moles (or nevi) are large masses of melanocytes that are usually benign but should be monitored for changes that could indicate the presence of skin cancer. See Figure 5.31[21] for an image of a normal-appearing mole.

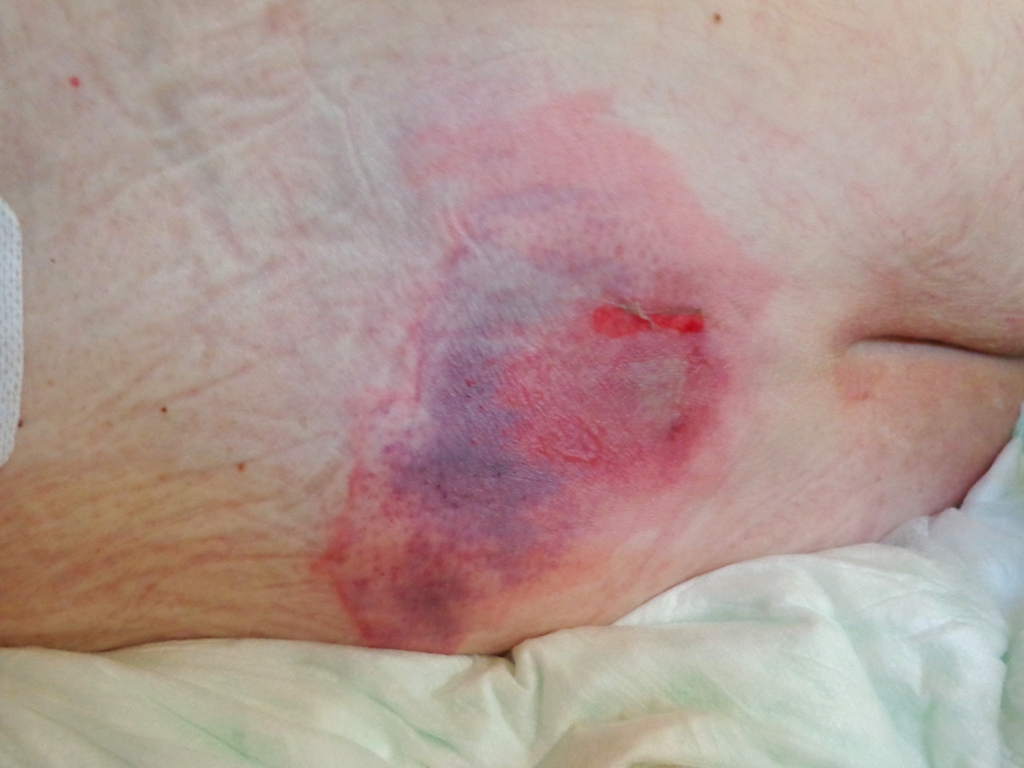
Pressure Injuries
Pressure injuries (also known as pressure ulcers, decubitus ulcers, and bedsores) are caused by constant pressure on bony areas that reduce blood flow and lead to tissue injury and necrosis (tissue death). See Figure 5.32[22] for an image of a pressure injury.
Psoriasis
Psoriasis is a skin condition in which keratinocytes in the epidermis divide and move too quickly to the surface, resulting in patchy, scaly build-ups on the skin. See Figure 5.33[23] for an image of psoriasis on an individual’s arm.

Shingles
Shingles is a painful rash that occurs along nerves and is caused by reactivation of the varicella-zoster virus. Chicken pox is a disease caused by the first exposure to the virus, and shingles is a reactivation of the same virus. See Figure 5.34[24] for an image of shingles.

Skin Cancer
The Skin Cancer Foundation reports that one in five Americans will experience some type of skin cancer in their lifetime. Too much sun exposure can lead to wrinkling of the skin due to the destruction of the cellular structure and, in severe cases, can cause enough DNA damage to result in skin cancer. One of the contributing factors to the increase in the number of skin cancer cases is the breakdown of the ozone layer of the atmosphere, which has resulted in increased exposure to UV radiation. Other risk factors for skin cancer include older age, family history, fair skin, and immunosuppression.
Skin cancers fall into three main types: basal cell carcinoma, squamous cell carcinoma, and malignant melanoma.
Basal Cell Carcinoma
Basal cell carcinoma is a form of skin cancer that affects the stem cells in the stratum basale layer of the epidermis. It is the most common type of skin cancer in the United States and is frequently found on the head, neck, arms, and back, which are the areas most susceptible to long-term sun exposure.
Although UV radiation is the main cause of basal cell carcinoma, exposure to other agents, such as arsenic and radiation medical therapy, can also lead to basal cell carcinoma.
Basal cell carcinomas start in the stratum basale and usually spread along this boundary. At some point, they begin to grow toward the surface and become an uneven patch, bump, growth, or scar on the skin surface. Like most cancers, basal cell carcinomas respond best to treatment when caught early. Treatment options include surgery, freezing (cryosurgery), and topical ointments.
See Figure 5.35[25] for an image of basal cell carcinoma.

Squamous Cell Carcinoma
Squamous cell carcinoma is the second most common skin cancer. The American Cancer Society reports that two out of every ten skin cancers are squamous cell carcinomas. It is more aggressive than basal cell carcinoma. Squamous cell carcinoma affects the keratinocytes of the stratum spinosum and usually appears as lesions on the scalp, ears, and hands. If not removed, these carcinomas can metastasize or spread to other areas of the body. Surgery and radiation are used to treat squamous cell carcinoma. See Figure 5.36[26] for an image of squamous cell carcinoma.

Melanoma
A melanoma is a cancer characterized by the uncontrolled growth of melanocytes, the melanin-producing cells in the epidermis. Typically, a melanoma develops from a mole. It is the most fatal of all skin cancers, as it is highly metastatic and can be difficult to detect before it has spread to other organs. Melanomas usually appear as asymmetrical brown and black patches with uneven borders and a raised surface. Treatment typically involves surgical excision and immunotherapy. See Figure 5.37[27] for an image of melanoma.

Patients are taught the following ABCDE mnemonic to help notice signs of early-stage melanoma. If you observe a mole on your body displaying these signs, consult your health care provider:
- Asymmetry – the two sides are not symmetrical or don’t match
- Borders – the edges are irregular in shape
- Color – the color is varied shades of brown, black, or other colors
- Diameter – it is larger than 6 mm (0.24 in), the size of a pencil eraser
- Evolving – its shape has changed, or it is growing
Some specialists cite the following additional signs for serious forms of nodular melanoma:
- Elevated – it is raised on the skin surface
- Firm – it feels hard to the touch
- Growing – it is getting larger
Striae
Striae, commonly called stretch marks, result when the dermis is stretched beyond its limits of elasticity, often due to rapid weight gain during puberty and pregnancy. They often appear on the hips and abdomen and initially have a reddish color but lighten over time. See Figure 5.38[28] for an image of striae.

Vitiligo
Vitiligo is a skin condition in which melanocytes in some areas lose their ability to produce melanin, resulting in lighter patches of skin. See Figure 5.39[29] for an image of vitiligo on a person with darker-pigmented skin.

Wart
A wart is an uncontrolled growth of epidermal cells caused by the papilloma virus. See Figure 5.40[30] for an image of a wart on a toe.

- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “515_Acne_formation” by OpenStax College is licensed under CC BY 3.0 ↵
- “12135299916_fcfb0b2012_h” by Felipe Fernandes is licensed under CC BY-SA 2.0 ↵
- “Alopecia_areata_1” by Thirunavukkarasye-Raveendran is licensed under CC BY 4.0 ↵
- “513_Degree_of_burns” by OpenStax College is licensed under CC BY 3.0 ↵
- “Burn_Degree_Diagram” by Persian Poet Gal at English Wikipedia is licensed under CC BY 3.0 ↵
- “First-degree_burn” by Bejinhan is licensed under CC BY-SA 3.0 ↵
- “Hand2ndburn” by Kronoman is licensed under CC BY-SA 3.0 ↵
- “8-day-old-3rd-degree-burn” by Craig0927 is in the Public Domain ↵
- ”Ожог Кисть” by goga312 is licensed under CC BY-SA 3.0 ↵
- “Calluses” by Jmarchn is licensed under CC BY-SA 3.0 ↵
- “Dandruff_with_Hair” by BestShah is licensed under CC BY-SA 4.0 ↵
- “Eczema-arms” by Jambula at English Wikipedia is in the Public Domain. “Child_with_Eczema_(34034003933)” by NIAID is licensed under CC BY 2.0 ↵
- “Vesnuschki” by Loyna is licensed under CC BY-SA 2.5 ↵
- “Athlete%27s_foot” by ProjectManhattan is licensed under CC BY-SA 3.0 ↵
- “PMC4103002_ircmj-16-9410-g001” by Gacaferri Lumezi B, Goci A, Lokaj V, Latifi H, Karahoda N, Minci G, Telaku D, Gercari A, Kocinaj A is licensed under CC BY 3.0 ↵
- “Rash” by Enochlau is licensed under CC BY-SA 3.0 ↵
- “Hyperhidrosis” by Amnaijaz23 is licensed under CC BY-SA 4.0 ↵
- “Keloid,_Post_Surgical” by Htirgan is licensed under CC BY-SA 3.0 ↵
- “Suture,_before_and_after,_RMO” by Jeanne Oostdyk is licensed under CC BY-SA 3.0 ↵
- “Normal Mole with No Color Differences” by unknown Photographer, Skin Cancer Foundation is in the Public Domain ↵
- “Decubitus_01” by AfroBrazilian is licensed under CC BY-SA 3.0 ↵
- “Psoriasis_002” by Jacopo188 is licensed under CC BY-SA 3.0 ↵
- “Shingles_on_the_chest” by Preston Hunt (me@prestonhunt.com) is licensed under CC BY 3.0 ↵
- “Basal_cell_carcinoma” by John Hendrix is in the Public Domain. ↵
- “Squamous_Cell_Carcinoma” by unknown photographer is in the Public Domain. ↵
- “Melanoma” by unknown photographer is in the Public Domain. ↵
- “Striae_Alba_-_Stretch_Mark” by Medicalpal is licensed under CC BY-SA 4.0 ↵
- “Vitiligo” by Grook Da Oger is licensed under CC BY-SA 4.0 ↵
- “Verruca_vulgaris_on_the_first_toe” by Mndno is licensed under CC BY-SA 3.0 ↵
A skin condition that typically occurs on the face and back which are areas rich in sebaceous (oil) glands.
A genetic disorder that completely or partially affects the color of the skin, hair, and eyes due to the inability of melanocytes to produce melanin.
The medical term for hair loss in areas where hair normally grows.
Skin damage caused by intense heat, radiation, electricity, or chemicals.
A superficial burn that affects only the epidermis.
Referred to as a partial thickness burn, affects both the epidermis and a portion of the dermis.
Referred to as full thickness burns that extend fully into the epidermis, dermis, and hypodermis destroying the tissue and affecting the nerve endings and sensory function.
Burns that extend fully into the epidermis, dermis, and hypodermis destroying the tissue and affecting the nerve endings and sensory function.
Burn affecting the underlying muscle and bone.
A thickened area of the epidermis due to constant rubbing or abrasion.
A specialized form of a callus formed by abrasions on the skin that result from an elliptical-type motion.
A condition of flakes of dead skin from the scalp.
An allergic reaction that appears as dry, itchy patches of skin resembling rashes.
Patches of melanin determined by genetics.
Group of skin diseases caused by a fungus, types include ringworm, athlete’s foot, and jock itch.
The medical term for excessive hair growth in areas where hair is usually minimal or absent.
Circular, fluid-filled, itchy, raised lesions, often due to an allergic reaction.
Circular, fluid-filled, itchy, raised lesions, often due to an allergic reaction.
A medical condition of excessive sweating that is not related to heat or exercise.
A raised bump due to an overproduction of scar tissue.
An irregular tear or cut of the skin that may require suturing or other type of surgical repair.
Large masses of melanocytes that are usually benign, but should be monitored for changes that could indicate the presence of skin cancer.
Large masses of melanocytes that are usually benign, but should be monitored for changes that could indicate the presence of skin cancer.
Caused by constant pressure on bony areas that reduce blood flow and lead to tissue injury, also known as pressure ulcers, decubitus ulcers, and bedsores.
Tissue death
A skin condition in which keratinocytes in the epidermis divide and move too quickly to the surface, resulting in patchy, scaly build-ups on the skin.
A painful rash that occurs along nerves and is caused by reactivation of the varicella-zoster virus.
A form of skin cancer that affects the stem cells in the stratum basale layer of the epidermis.
The second most common skin cancer, affecting the keratinocytes of the stratum spinosum, and usually appears as lesions on the scalp, ears, and hands.
Spread to other areas of the body.
Cancer characterized by the uncontrolled growth of melanocytes, the melanin-producing cells in the epidermis.
When the dermis is stretched beyond its limits of elasticity, often due to rapid weight gain during puberty and pregnancy. They often appear on the hips and abdomen and initially have a reddish color, but lighten over time. Commonly called stretch marks.
A skin condition in which melanocytes in some areas lose their ability to produce melanin resulting in lighter patches of skin.
An uncontrolled growth of epidermal cells caused by the papilloma virus.

