16.7 Reproductive System Diseases and Disorders
Reproductive System Diseases and Disorders
Andropause (Male Menopause)
Declines in Leydig cell activity can occur in males beginning at 40 to 50 years of age. Because Leydig cells secrete testosterone, the resulting reduction in testosterone can lead to symptoms of andropause, also known as male menopause. While the reduction in sex hormones is similar to female menopause, there is no clear sign—such as a lack of a menstrual period—to indicate the beginning of andropause. Instead, people with this condition report feelings of fatigue, reduced muscle mass, depression, anxiety, irritability, loss of libido, and insomnia. A reduction in spermatogenesis resulting in lowered fertility is also reported, and sexual dysfunction can also be associated with andropausal symptoms.
While some researchers believe that certain aspects of andropause are difficult to tell from aging in general, testosterone replacement may be prescribed to alleviate some symptoms. Androgen replacement therapy may help prevent new onset of depression in elderly males, but long-term treatment with high doses of testosterone can sharply increase the risk of heart disease and prostate cancer.
Benign Prostatic Hypertrophy
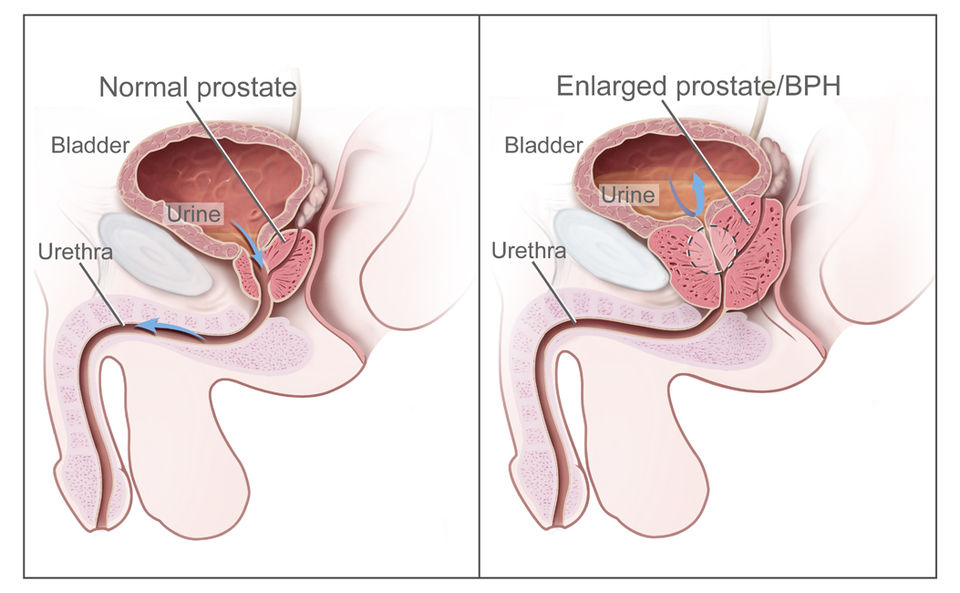
The prostate gland in males normally doubles in size during puberty. At approximately age 25, it gradually begins to enlarge again, but does not cause problems. Abnormal growth of the prostate, or benign prostatic hypertrophy (BPH), can cause constriction of the urethra as it passes through the middle of the prostate gland, leading to a number of lower urinary tract symptoms, such as a frequent and intense urge to urinate, a weak stream, and a sensation that the bladder has not emptied completely.
By age 60, approximately 40 percent of males have some degree of benign prostatic hypertrophy. By age 80, the number of affected individuals is as high as 80 percent. Treatments for BPH attempt to relieve the pressure on the urethra so that urine can flow more normally. Mild to moderate symptoms are treated with medication, whereas severe enlargement of the prostate is treated by surgery in which a portion of the prostate tissue is removed. See Figure 16.18[1] for an illustration comparing a normal prostate to benign prostatic hypertrophy.
Breast Cancer[2],[3]
Breast cancer occurs when cancerous cells in the breasts multiply and form tumors. About 80% of breast cancer cases are invasive, meaning a tumor may spread from the breast to other areas of the body. Breast cancer typically affects women aged 50 and older, but it can also affect women who are younger than 50. Men may also develop breast cancer. People of both genders who have a strong family history of breast cancer or inherited changes in BRCA1 and BRCA2 genes have a high risk of getting breast cancer.
Types of Breast Cancer
Because there are several types of breast cancer, an accurate diagnosis must be made so that the appropriate treatment is used. Common types of breast cancer include the following:
- Invasive (infiltrating) ductal carcinoma (IDC): This cancer starts in the milk ducts and spreads to nearby breast tissue. It is the most common type of breast cancer in the United States.
- Lobular breast cancer: This breast cancer starts in the milk-producing glands (lobules) in the breast and often spreads to nearby breast tissue. It is the second most common breast cancer in the United States.
- Ductal carcinoma in situ (DCIS): Like IDC, this breast cancer starts in the milk ducts. The difference is DCIS doesn’t spread beyond the milk ducts.
Less common breast cancer types are as follows:
- Inflammatory breast cancer (IBC): This rare, fast-growing cancer looks like a rash on the breast.
- Paget’s disease of the breast: This rare cancer affects the skin of the nipple and may look like a rash. Less than 4% of all breast cancers are Paget’s disease of the breast.
Breast Cancer Subtypes
Health care providers classify breast cancer subtypes by receptor cell status. Receptors are protein molecules in or on breast cancer cell membranes that attach to certain proteins or hormones, such as estrogen and progesterone. Estrogen and progesterone promote the growth of cancerous cells. Determining if cancerous cells have estrogen or progesterone receptors helps health care providers plan breast cancer treatment.
Subtypes of breast cancer include the following:
- ER-positive (ER+): Estrogen receptors are present.
- PR-positive (PR+): Progesterone receptors are present.
- HR-positive (HR+): Estrogen and/or progesterone receptors are present.
- HR-negative (HR-): Estrogen or progesterone receptors are not present.
- HER2-positive (HER2+): Higher than normal levels of the HER2 protein are present, leading to accelerated cell growth. About 15% to 20% of all breast cancers are HER2-positive.
- Triple-negative breast cancer (TNBC): Estrogen and progesterone receptors are not present, and HER2 protein is not present. This invasive cancer is aggressive and spreads more quickly than other breast cancers.
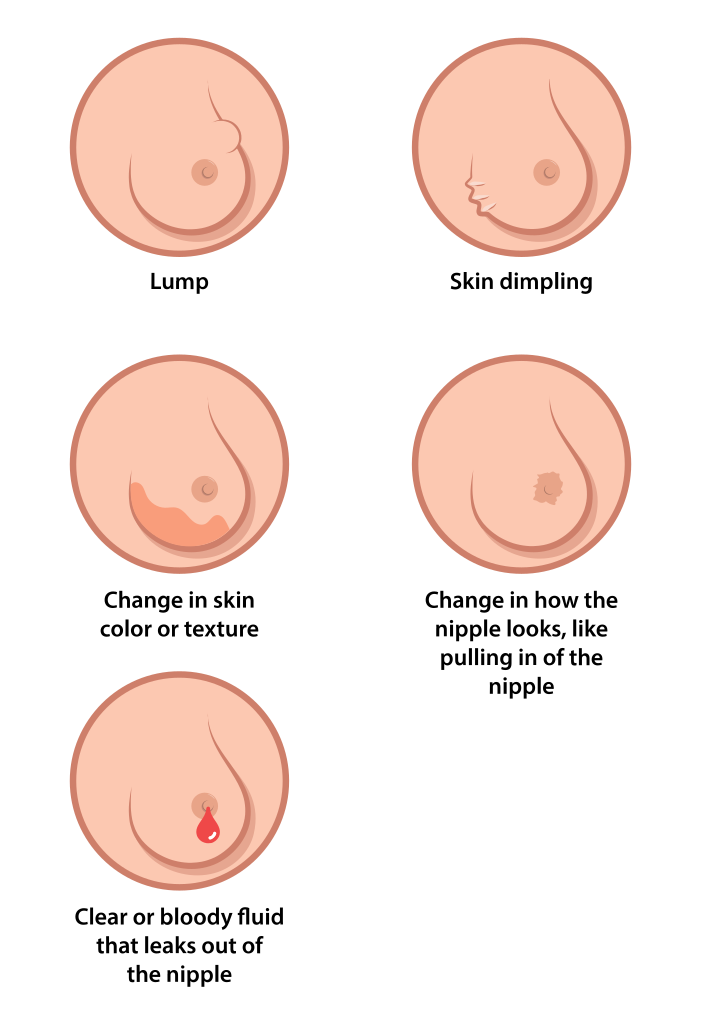
Breast cancer may not cause noticeable symptoms, but when it does, symptoms may include a change in the size, shape, or contour of the breast; a mass or lump, which may feel as small as a pea; a lump or thickening in or near the breast or in the underarm that persists throughout the menstrual cycle; a change in the look or feel of the skin on the breast or nipple (dimpled, puckered, scaly, inflamed or red, purple, or darker than other parts of the breast); a marble-like hardened area under the skin; and a blood-stained or clear fluid discharge from the nipple. See Figure 16.19[4] for an illustration of potential symptoms of breast cancer.
The American Cancer Society recommends a mammogram every year for most women starting at age 45. A mammogram is a radiographic image of breast tissue that can detect signs of cancer, often before a lump is felt. People suspected of having breast cancer or those at high risk may have additional diagnostic tests. Breast cancer may be treated with surgery, such as mastectomy (removal of one or both breasts), lumpectomy (removal of the tumor), and breast reconstruction. Other treatments include chemotherapy; radiation therapy; immunotherapy; or hormone therapy, including selective estrogen receptor modulator (SERM) therapy and other targeted therapy.
Cervical Cancer[5]
Cervical cancer begins when abnormal cells in the cervix become cancerous. This type of cancer tends to grow slowly, but if left untreated, it can spread to other parts of the body. Almost all cervical cancers are caused by infection with a virus called human papillomavirus (HPV). There are many types of HPV, but the types that cause cancer are called “high-risk HPV.” High-risk HPV is very common and is transmitted during oral, vaginal, or anal sex. However, HPV typically does not cause symptoms, and most people don’t know they have it. When cancer cells begin to grow in the cervix, symptoms may include abnormal vaginal bleeding, such as bleeding after sex or between menstrual periods, or pelvic pain or pain during sex.
Treatment for cervical cancer depends on the type of cancer and whether it has spread. Treatments include surgery to remove the cancer, radiation therapy, chemotherapy, targeted therapy, and immunotherapy.
Almost all cervical cancer can be prevented by the HPV vaccination. Read more about HPV vaccination in the “Human Papillomavirus Infection” subsection. Cervical cancer can also be prevented or diagnosed early by routine cervical cancer screening. Two types of screening tests use a sample of cervical cells that your provider collects with a swab: a Pap smear checks for abnormal cells so they can be treated before they become cancer, and an HPV test checks for high-risk HPV infections that can cause cancer.
Cryptorchidism[6]
A testis that doesn’t move down into its proper place in the scrotum before birth is called cryptorchidism or an undescended testicle. Most often, just one testicle does not descend into the scrotum, but sometimes both testicles are affected.
An undescended testicle is more common in premature babies than it is in full-term infants. An undescended testicle often moves down into the scrotum on its own within a few months after the baby is born. If a baby has an undescended testicle that doesn’t correct itself, surgery is performed to move the testicle into the scrotum. Treatment before age 1 may lower the risk of health problems linked with an undescended testicle, such as infertility and testicular cancer.
Ectopic Pregnancy[7]
An ectopic pregnancy occurs when a fertilized egg implants and grows outside of the uterus, most commonly in the Fallopian tube, where the tissue cannot support the growing embryo. If left untreated, rupture of the growing tissue can cause severe internal bleeding and potential death. Symptoms of an ectopic pregnancy are similar to a normal early pregnancy, but additional symptoms, such as abdominal pain and vaginal bleeding require immediate medical attention. Treatment depends on the stage of the ectopic pregnancy and may include medication to dissolve the ectopic tissue or surgery to remove the ectopic pregnancy (sometimes including the affected Fallopian tube).
Endometriosis[8]
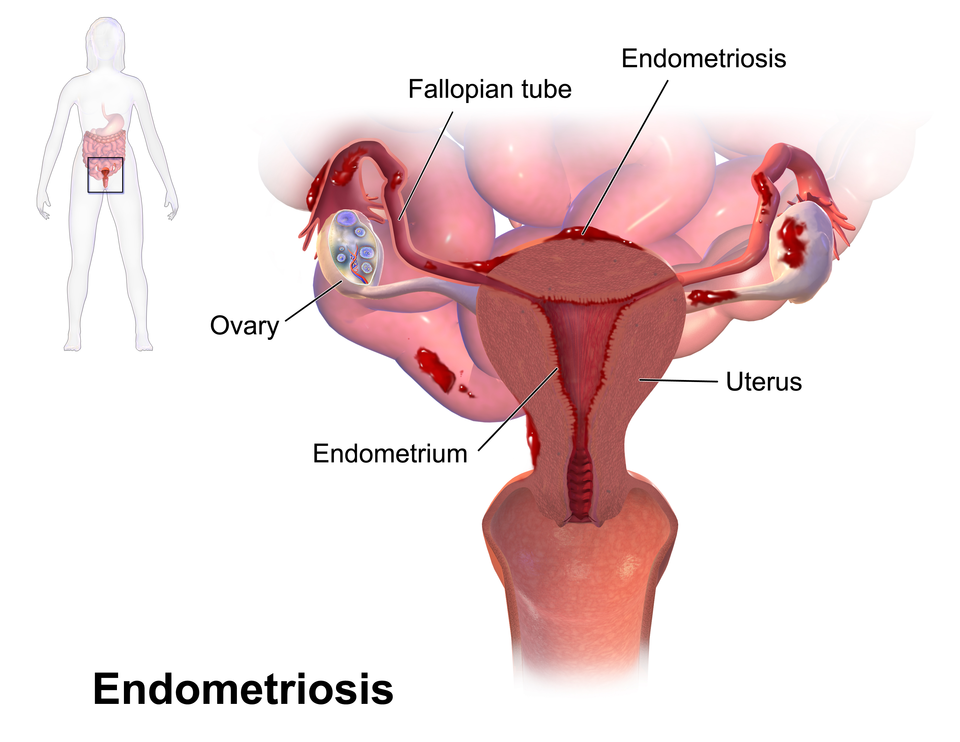
Endometriosis is a common health problem in women with approximately 11% of women, or more than 6.5 million women in the United States, having endometriosis. Endometriosis can happen in any individual who has menstrual periods, but it is more common in women in their 30s and 40s. It gets its name from the word endometrium, the tissue that normally lines the uterus. Endometriosis happens when tissue similar to the lining of the uterus grows outside of the uterus and in other areas in the body where it doesn’t belong. Most often, endometriosis is found on the ovaries, Fallopian tubes, tissues that hold the uterus in place, and the outer surface of the uterus. Other sites for growths can include the vagina, cervix, vulva, bowel, bladder, or rectum. Rarely, endometriosis appears in other parts of the body, such as the lungs, brain, and skin. See Figure 16.20[9] for an illustration of endometriosis.
Symptoms of endometriosis are as follows:
- Pain: Women with endometriosis commonly experience different kinds of pain, including the following:
- Very painful menstrual cramps that may worsen over time
- Chronic (long-term) pain in the lower back and pelvis
- Pelvic pain during or after sex, usually described as a “deep” pain
- Abdominal pain
- Painful bowel movements or pain when urinating during menstrual periods
- Bleeding or spotting between menstrual periods
- Infertility (not being able to get pregnant)
- Digestive problems such as diarrhea, constipation, bloating, or nausea, especially during menstrual periods
There is no cure for endometriosis. Symptoms may be managed with medications or surgical procedures.
Erectile Dysfunction[10]
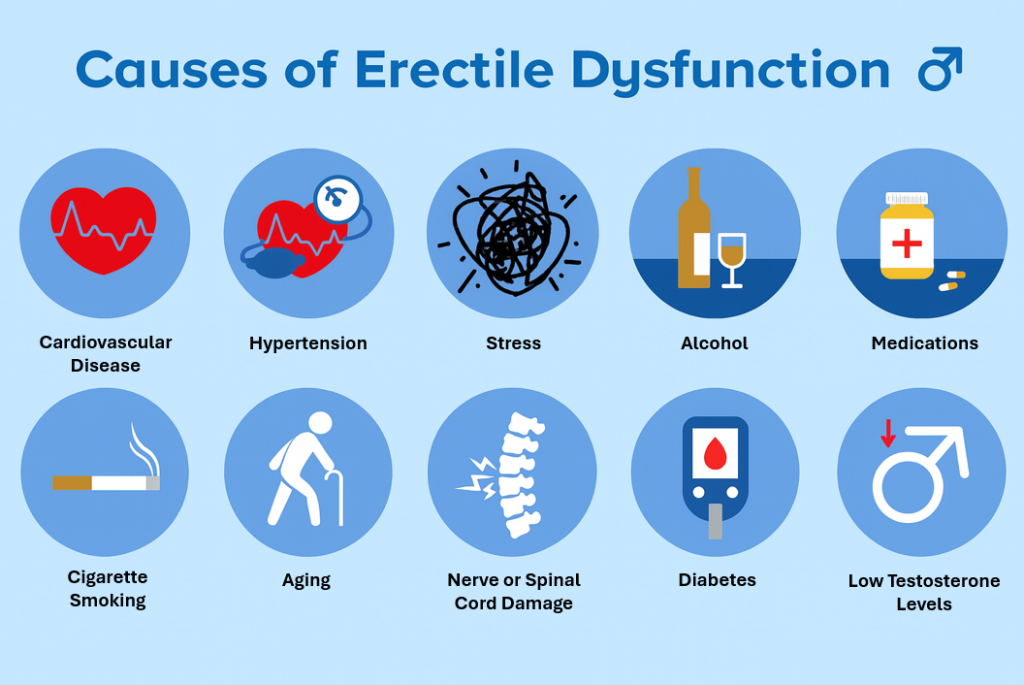
Erectile dysfunction (ED) is the difficulty or inability to attain and/or maintain an erection that is sufficient for satisfactory sexual activity. Erectile dysfunction is a relatively common problem, affecting up to 30 million men of all ages in the United States and more than 150 million worldwide. The ability to have an erection requires complex coordination between nerves, blood vessels, muscles, and the brain.
A variety of factors – frequently in combination – can cause erectile dysfunction. These factors include neurological, hormonal, and vascular disorders, as well as the natural aging process and certain chronic diseases. ED is also a common side effect of treatments for prostate cancer. In addition, psychological issues, such as depression, anxiety, or performance concerns, play at least some part in virtually every case of ED. See Figure 16.21[11] for an illustration of common factors causing erectile dysfunction.
Human Papillomavirus Infection (HPV)[12],[13]
Human papillomavirus (HPV) is a common sexually transmitted infection that can affect males and females. More than half of sexually active men and women will become infected with HPV at some point in their lifetime.
HPV strains are classified as high or low risk according to their potential to cause cancer. Though most HPV infections do not cause disease, the disruption of normal cellular functions in the low-risk forms of HPV can cause genital warts. In most healthy individuals, the immune system is able to clear these strains of HPV infection within two years. However, more serious, high-risk strains of HPV can result in cancer of the vulva, vagina, penis, anus, or throat. Read more about cancer in the “Cervical Cancer” subsection.
The Centers for Disease Control and Prevention recommends routine HPV vaccination for males and females beginning at age 11, before possible exposure when becoming sexually active, and for everyone through age 26 years if not adequately vaccinated when younger.[14]
Infertility[15]
Infertility is the inability to conceive after 12 months of unprotected sexual intercourse or after six months of unprotected intercourse for women over 35 years old. It also refers to the inability of a woman to carry a pregnancy to live birth. Infertility affects millions of people around the world and can also impact their families and communities. Estimates suggest that approximately one in every six people of reproductive age worldwide experience infertility in their lifetime. In the male reproductive system, infertility is most commonly caused by problems in the ejection of semen, low levels or absences of sperm production, or abnormal morphology (shape) or motility (movement) of sperm. In the female reproductive system, infertility may be caused by a variety of abnormalities of the ovaries, uterus, Fallopian tubes, and the endocrine system. In some cases, a specific cause for a couple’s infertility cannot be determined.
Inguinal Hernia[16]
A hernia occurs when tissue from one body cavity bulges through an opening in the muscle wall into another. Inguinal hernias are the most common type of hernia, making up 75% of all hernias. Around 25% of males will have an inguinal hernia during their lifetime, compared to 2% of females.
Inguinal hernias occur when abdominal tissue bulges through an opening in the lower abdominal wall called the inguinal canal, a passageway that runs down either side of the pelvis into the sex organs. During development in male infants, the testicles descend from the abdomen and pass through the inguinal canal to reach the scrotum, making this preexisting opening a common place for hernias to develop. In females, the inguinal canal is narrower and contains the round ligament that supports the uterus. This tough ligament helps to reinforce the muscle wall. Women with connective tissue disease are more susceptible to hernias. Inguinal hernias are treated with surgery to prevent complications.
Pelvic Inflammatory Disease[17]
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs that typically occurs when a sexually transmitted infection spreads from the vagina to the uterus, Fallopian tubes, or ovaries. Many types of bacteria can cause PID, but gonorrhea and chlamydia are the most common causes. Less commonly, bacteria can enter the reproductive tract during menstruation, childbirth, miscarriage, or abortion.
The signs and symptoms of pelvic inflammatory disease might be mild and difficult to recognize. When signs and symptoms of PID are present, they most often include pain, ranging from mild to severe in the lower abdomen and pelvis; unusual or heavy vaginal discharge that may have an unpleasant odor; unusual vaginal bleeding during or after sex or between periods; pain during sex; fever; and painful or frequent urination.
PID is treated with medications to treat the underlying infection, but scarring or damage that may have occurred due to the infection cannot be reversed.
Polycystic Ovary Syndrome[18]
Polycystic ovary syndrome (PCOS) is a condition characterized by hormone imbalances, ovulatory dysfunction, and multiple ovarian cysts (i.e., small sacs of fluid). Fluid-filled cysts containing immature eggs are called follicles. Instead of releasing an egg during ovulation, the follicles (cysts) build up and enlarge. See Figure 16.22[19] for an illustration of PCOS.
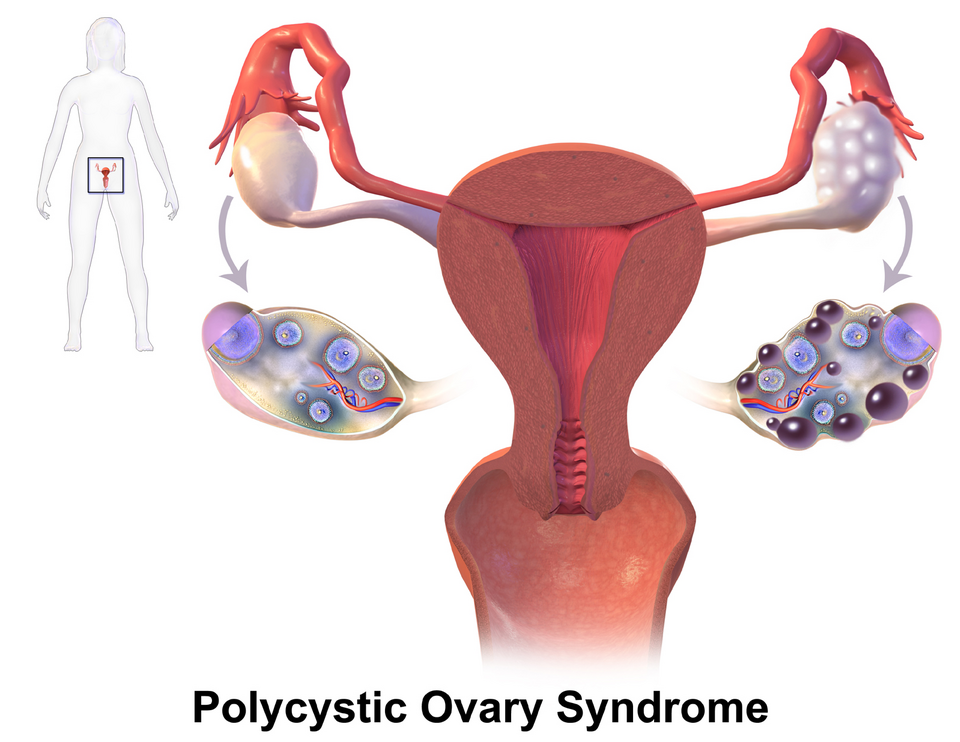
PCOS has no known cause, but it is associated with obesity and excessive insulin production. Common symptoms of PCOS include oligomenorrhea, amenorrhea, polymenorrhea, and enlarged ovaries due to multiple cysts or follicles. High levels of androgen hormones associated with PCOS can cause hirsutism or excess facial and body hair. PCOS can also cause infertility.
PCOS is diagnosed with blood tests and a transvaginal ultrasound. Treatments for PCOS include birth control pills to control menstrual cycles, diabetes medications to reduce insulin resistance, and medication to promote ovulation.
Premenstrual Syndrome (PMS)[20]
Many women feel physical or mood changes during the days before menstruation. When these symptoms happen every month and they are significant enough to affect a woman’s quality of life, they are known as premenstrual syndrome (PMS).
Emotional symptoms include depression, angry outbursts, irritability, crying spells, anxiety, confusion, social withdrawal, poor concentration, insomnia, increased nap taking, and changes in sexual desire. Physical symptoms include thirst and appetite changes (food cravings), breast tenderness, bloating and weight gain, headache, swelling of the hands or feet, aches and pains, fatigue, skin problems, gastrointestinal symptoms, and abdominal pain.
Mild to moderate symptoms may be relieved by changes in lifestyle or diet, but medications may be prescribed if PMS symptoms are severe and interfere with daily life.
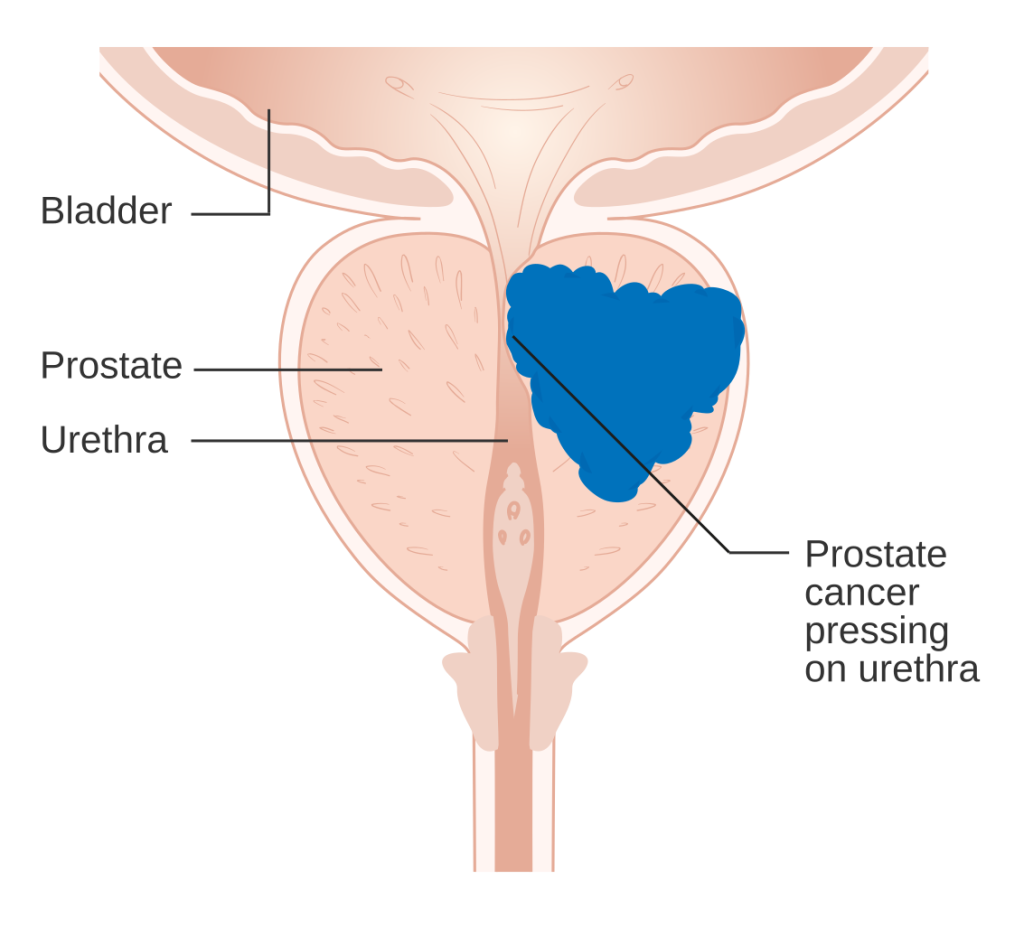
Prostate Cancer[21]
Prostate cancer is a common type of cancer in males over age 50. Prostate cancer typically grows slowly. The risk for developing prostate cancer increases in males with a family history of prostate cancer or African American ancestry. Early prostate cancer is often asymptomatic but may cause problems urinating; blood in the urine or semen; or pain in the lower back, hips, or pelvis. However, many men develop problems urinating from an enlarged prostate as they age, making early signs of prostate cancer easy to miss. Aggressive types of prostate cancer can spread to other parts of the body, most commonly the bones and lymph nodes.
Treatment options depend on a person’s age, their general health, and the aggressiveness of the cancer. Treatment may include active surveillance, surgical removal of the cancer, radiation therapy, hormone therapy, chemotherapy, targeted therapy, and immunotherapy.
See Figure 16.23[22] for an illustration of prostate cancer.
Prostatitis[23]
Prostatitis is inflammation of the prostate, a painful condition that occurs in 10-12% of young and middle-aged men. Symptoms of prostatitis include painful urination, frequent urination, burning in the penis with or without urination, pain in the rectum and scrotal area, lower abdominal or back pain, pain with ejaculation, and fever or chills.
There are four types of prostatitis:
- Acute bacterial prostatitis is diagnosed based on bacteria and white blood cells present in the urine and prostate fluid and is typically treated with intravenous antibiotics for up to two to four weeks.
- Chronic bacterial prostatitis refers to long-term infection in the prostate that seems to resolve and reoccur. Treatment includes antibiotics for up to six months to prevent recurrent infection. If a blockage is present that causes incomplete emptying of the bladder, surgery may be performed.
- Chronic prostatitis/chronic pelvic pain syndrome is the most common but least understood type of prostatitis and results in inflammation of the prostate for more than three months in men of any age. It may or may not be caused by a bacterial infection, and it may cause chronic pelvic pain. Treatment may include antibiotics if caused by a bacterial infection, medications to relax the muscle tissue in the prostate, and pain relievers. Lifestyle changes, such as avoiding caffeine, alcohol, and spicy foods, as well as stress management techniques, may improve symptoms.
- Asymptomatic inflammatory prostatitis is diagnosed when there are white blood cells present in semen, but the patient does not have pain or discomfort. This type of prostatitis is diagnosed when a patient is being evaluated for causes of infertility or tested for prostate cancer, and no treatment is required.
Sexually Transmitted Infection[24],[25]
Sexually transmitted infections (STIs) are caused by bacteria, viruses, or parasites that are passed from person to person during exposure to body fluids during sexual contact, including oral, vaginal, and anal sex. STIs can also spread to infants from their mothers during pregnancy or childbirth. Some STIs, such as hepatitis and HIV, can also be spread through blood by drug users sharing needles.
STIs do not always cause symptoms. A person can get an STI from another person who seems healthy and does not know they have an infection. Common STIs and their symptoms include the following:
- Chlamydia: A common bacterial infection that can cause vaginal or penile discharge, painful urination, and pelvic pain.
- Genital Herpes: A chronic viral infection that causes sores and blisters on the genitals.
- Gonorrhea: A common bacterial infection that can cause painful urination, discharge, and painful intercourse.
- Hepatitis B or C: A viral infection that damages the liver.
- HIV: A chronic viral infection that weakens the immune system and can lead to AIDS.
- Human Papillomavirus (HPV): A common viral infection that can cause genital warts and cancer.
- Syphilis: A bacterial infection that can progress through different stages, causing sores, rash, and serious complications if left untreated.
- Trichomoniasis: A parasitic infection that can cause vaginal discharge, itching, and painful urination.
STIs are treated with antibiotics or antivirals based on the cause but cannot always be cured. For example, genital herpes cannot be cured. There are many ways to prevent STIs. The best way to prevent STIs is to not have sex or to have sex in a long-term, mutually monogamous relationship, meaning you both agree to be sexually active only with each other after being tested for possible STIs. Vaccinations, such as the HPV or hepatitis vaccines, can also help prevent these STIs. Otherwise, before participating in any sexual contact, it is important to talk to your partner about practicing safer sex and using latex condoms consistently and correctly.
Testicular Cancer[26]
Testicular cancer typically occurs in young men between the ages of 15 and 45. The first sign of testicular cancer often is a lump on a testicle. The cancer cells can grow quickly and spread to other parts of the body. If diagnosed and treated early with surgery and chemotherapy, testicular cancer has a high cure rate.
Testicular Torsion[27]
Testicular torsion occurs when a testicle rotates, twisting the spermatic cord that brings blood to the scrotum. The reduced blood flow causes sudden, severe pain and swelling. Testicular torsion commonly occurs between ages 12 and 18 and usually requires emergency surgery. If treated quickly, the testicle can usually be saved. But when blood flow has been cut off for too long, a testicle might become so badly damaged that it has to be removed.
- ”Benign_Prostatic_Hyperplasia_nci-vol-7137-300” by unknown author, via National Cancer Institute is in the Public Domain. ↵
- Cleveland Clinic. (2023). Breast cancer. https://my.clevelandclinic.org/health/diseases/3986-breast-cancer ↵
- American Cancer Society. (2023). Breast cancer. https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html ↵
- “Breast_cancer_illustration_en.svg” by Raphseck is licensed under CC BY-SA 4.0 ↵
- Medline [Internet]. (n.d.). Cervical cancer. https://medlineplus.gov/cervicalcancer.html ↵
- Mayo Clinic. (2023). Undescended testicle. https://www.mayoclinic.org/diseases-conditions/undescended-testicle/diagnosis-treatment/drc-20352000 ↵
- Mayo Clinic. (2022). Ectopic pregnancy. https://www.mayoclinic.org/diseases-conditions/ectopic-pregnancy/symptoms-causes/syc-20372088 ↵
- Eisenberg, E., & Chahine, E. B. (2021). Endometriosis. Office on Women’s Health. (https://womenshealth.gov/a-z-topics/endometriosis ↵
- “Blausen_0349_Endometriosis.png” by Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014” is licensed under CC BY 3.0 ↵
- Shindel, A. W. (2022). Erectile dysfunction. University of California San Francisco. https://www.ucsfhealth.org/conditions/erectile-dysfunction ↵
- This image is derived from “Common_causes_of_erectile_dysfunction” by Click2pharmacy.co.uk Images is licensed under CC BY 2.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Johnson, T. C. (2024). HPV Infection in men. WebMD. https://www.webmd.com/sexual-conditions/hpv-genital-warts/hpv-virus-men ↵
- Centers for Disease Control and Prevention. (2021). HPV vaccination recommendations. https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html#:~:text=Dosing%20Schedules%0A%0ATwo%20doses%20of%20HPV%20vaccine%20are,require%20a%20third%20dose%20of%20HPV%20vaccine ↵
- World Health Organization. (2024). Infertility. https://www.who.int/news-room/fact-sheets/detail/infertility#:~:text=Infertility%20is%20a%20disease%20of,types%20of%20medically%20assisted%20reproduction ↵
- Cleveland Clinic. (2022). Inguinal hernia (groin hernia). https://my.clevelandclinic.org/health/diseases/16266-inguinal-hernia ↵
- Mayo Clinic. (2022). Pelvic inflammatory disease (PID). https://www.mayoclinic.org/diseases-conditions/pelvic-inflammatory-disease/symptoms-causes/syc-20352594 ↵
- Mayo Clinic. (2022). Polycystic ovary syndrome (PCOS). https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439 ↵
- “PCOS_%28Part_2%29.png” by BruceBlaus is licensed under CC BY 4.0 ↵
- American College of Obstetricians and Gynecologists. (2023). Premenstual syndrome (PMS). https://www.acog.org/womens-health/faqs/premenstrual-syndrome ↵
- Medline [Internet]. (n.d.). Prostate cancer. https://medlineplus.gov/prostatecancer.html ↵
- “Diagram_showing_prostate_cancer_pressing_on_the_urethra_CRUK_182” by Cancer Research UK is licensed under CC BY-SA 4.0 ↵
- Department of Urology. (n.d.). Prostatitis. University of Washington Medicine. https://urology.uw.edu/patient-care/conditions-and-treatments/prostatitis ↵
- Mayo Clinic. (2023). Sexually transmitted diseases (STDs). https://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/symptoms-causes/syc-20351240 ↵
- Medline [Internet]. (n.d.). Sexually transmitted infections. https://medlineplus.gov/sexuallytransmittedinfections.html ↵
- Johns Hopkins Medicine. (n.d.). Testicular cancer. https://www.hopkinsmedicine.org/health/conditions-and-diseases/testicular-cancer ↵
- Mayo Clinic. (2022). Testicular torsion. https://www.mayoclinic.org/diseases-conditions/testicular-torsion/symptoms-causes/syc-20378270 ↵
A condition in males, also called male menopause, marked by a decline in testosterone levels and related symptoms, typically starting around 40 to 50 years of age.
Noncancerous enlargement of the prostate gland that can constrict the urethra and cause urinary symptoms like frequent urination, weak stream, and incomplete bladder emptying.
Cancer that starts in the milk ducts and spreads to nearby breast tissue. It is the most common type of breast cancer in the United States.
Breast cancer that starts in the milk-producing glands (lobules) in the breast and often spreads to nearby breast tissue. It is the second most common breast cancer in the United States.
Breast cancer that starts in the milk ducts but doesn’t spread beyond the milk ducts.
Rare, fast-growing cancer looks like a rash on the breast.
Rare cancer that affects the skin of the nipple and may look like a rash. Less than 4% of all breast cancers are Paget’s disease of the breast.
A slow-growing cancer that starts when abnormal cells in the cervix become malignant and can spread to other parts of the body if untreated.
A virus that causes almost all cases of cervical cancer by infecting cervical cells.
A testis that doesn't move down into its proper place in the scrotum before birth.
Occurs when a fertilized egg implants and grows outside of the uterus, most commonly in the fallopian tube, where the tissue cannot support the growing embryo.
A common health condition where tissue similar to the uterine lining grows outside the uterus, affecting about 11% of women in the U.S., especially those in their 30s and 40s.
The difficulty or inability to attain and/or maintain an erection that is sufficient for satisfactory sexual activity.
The inability to conceive after 12 months of unprotected sexual intercourse or after six months of unprotected intercourse for women over 35 years old.
The most common type of hernia, making up 75% of all hernias. Occurs when abdominal tissues bulge through an opening in the lower abdomen wall.
An infection of the female reproductive organs that typically occurs when a sexually transmitted infection spreads from the vagina to the uterus, Fallopian tubes, or ovaries.
A condition characterized by hormone imbalances, ovulatory dysfunction, and multiple ovarian cysts (i.e., small sacs of fluid).
The medical term for excessive hair growth in areas where hair is usually minimal or absent.
Menstruation symptoms that happen every month and are significant enough to affect a woman’s quality of life.
Inflammation of the prostate, a painful condition that occurs in 10-12% of young and middle-aged men.
Diagnosed based on bacteria and white blood cells present in the urine and prostate fluid and is typically treated with intravenous antibiotics for up to two to four weeks.
Long-term infection in the prostate that seems to resolve and reoccur. Treatment includes antibiotics for up to six months to prevent recurrent infection.
The most common but least understood type of prostatitis and results in inflammation of the prostate for more than three months in men of any age.
Diagnosed when there are white blood cells present in semen, but the patient does not have pain or discomfort.
A common bacterial infection that can cause vaginal or penile discharge, painful urination, and pelvic pain.
A chronic viral infection that causes sores and blisters on the genitals.
A common bacterial infection that can cause painful urination, discharge, and painful intercourse.
A viral infection that damages the liver.
A chronic viral infection that weakens the immune system and can lead to AIDS.
A bacterial infection that can progress through different stages, causing sores, rash, and serious complications if left untreated.
A parasitic infection that can cause vaginal discharge, itching, and painful urination.
Occurs when a testicle rotates, twisting the spermatic cord that brings blood to the scrotum.

