16.6 Female Puberty, Ovarian Cycle, & Menstrual Cycle
Female Puberty, Ovarian Cycle, & Menstrual Cycle
Much of the development of the reproductive system occurs during female puberty and is marked by the appearance of sex-specific characteristics in adolescents. Multiple factors influence the onset of puberty, including genetics, environment, and psychological stress. Historical data shows the effect of improved nutrition on the age of menarche (the start of menstruation) in the United States, which decreased from an average age of 17 in 1860 to 12.75 years in 1960, where it remains today. Body fat appears to have a strong role in determining menarche, likely due to the high metabolic needs of pregnancy and lactation to the human body. In fact, adolescent females who are extremely lean and highly active, such as gymnasts, often experience a delay in the onset of puberty.
Secondary Sex Characteristics
Female secondary sex characteristics are physical characteristics that are influenced by estrogen and are important for reproductive function. As a female reaches puberty, the first change usually visible is the development of the breasts. The reproductive organs will also grow at this time, axillary (armpit) and pubic hair will appear, and the hips widen. A growth spurt normally starts around the age of 9 to 11 and may last two years or more. During this time, height can increase up to three inches in a year.
Female Reproductive Hormones
Puberty is initiated by the gonadotropin-releasing hormone (GnRH), a hormone secreted by the hypothalamus. GnRH stimulates the anterior pituitary to secrete follicle stimulating hormone (FSH) and luteinizing hormone (LH). FSH targets the ovaries to stimulate follicular development (these follicles then secrete estrogens) and egg maturation. LH triggers ovulation, as well as the production of estrogens and progesterone by the ovaries.
The primary hormones produced by the ovaries are estrogens, which include estradiol, estriol, and estrone, and progesterone. Estrogens play an important role in many physiological processes, including the development of the reproductive system, regulation of the menstrual cycle, development of secondary sex characteristics, and the maintenance of pregnancy. Progesterone helps regulate the menstrual cycle and prepare for and maintain pregnancy.
Ovarian Cycle
The ovarian cycle is the development of oocytes and ovarian follicles within the ovary. During the reproductive years, it is a roughly 28-day cycle that occurs simultaneously with the menstrual (uterine) cycle (see below). The ovarian cycle includes two related processes: oogenesis (the production of an ovum) and folliculogenesis (the growth and development of ovarian follicles).
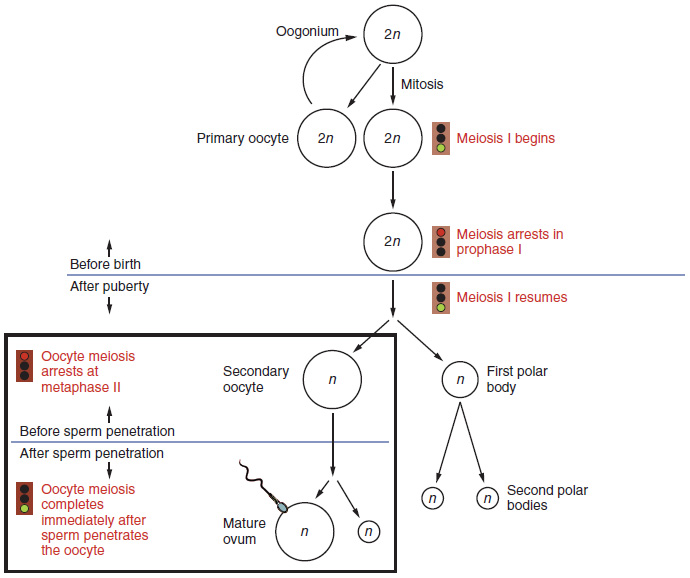
Oogenesis
The production of an ovum (egg) is called oogenesis. The process begins with ovarian stem cells called oogonia. Oogonia are formed during fetal development and divide via mitosis, much like spermatogonia in the testis. However, unlike spermatogonia, oogonia form millions of primary oocytes in the fetal ovaries prior to birth. These primary oocytes then stop at this stage of Meiosis I and resume meiosis years later at puberty and continue until close to menopause (the ending of a female’s reproductive functions). The number of primary oocytes present in the ovaries is approximately one to two million in an infant, which declines to approximately 400,000 at puberty and to zero by the end of menopause. See Figure 16.13[1] for an overview of oogenesis.
The initiation of ovulation—the release of an oocyte from the ovary—marks the transition from puberty into reproductive maturity. From then on, throughout the reproductive years, ovulation occurs approximately once every 28 days.
Just prior to ovulation, a surge of luteinizing hormone (LH) triggers the restarting of meiosis in a primary oocyte. This initiates the transition from primary to secondary oocyte. However, this cell division does not result in two identical cells. These cells have half the number of chromosomes as the primary oocyte. Also, the cytoplasm is divided unequally, and one daughter cell is much larger than the other. This larger cell, the secondary oocyte, eventually leaves the ovary during ovulation. The smaller cell, called the first polar body, may or may not divide again; but in either case, it eventually disintegrates. Therefore, even though oogenesis produces up to four cells, only one survives. Only if fertilization by a sperm occurs, will the secondary oocyte ever finish meiosis by dividing into an ovum and a second polar body (which disintegrates).
View a supplementary YouTube video[2] on oogenesis: Oogenesis: Learn@Visible Body.
Folliculogenesis
After puberty, follicles grow and develop in a process called folliculogenesis, which typically leads to ovulation of one oocyte approximately every 28 days, along with death to multiple other follicles. The death of ovarian follicles is called atresia and can occur at any point during follicular development.
Folliculogenesis begins with follicles in a resting state. These small primordial follicles are present in female newborns and are the most common type of follicle in the adult ovary. Primordial follicles have a single flat layer of support cells, called granulosa cells, that surround the oocyte, and they can stay in this resting state for years—some until right before menopause.
Some primordial follicles will grow in response to the hormone FSH to become primary follicles. Primary follicles start with the same single layer of granulosa cells, but they become active, increase in size, and proliferate.
As the granulosa cells divide, the follicles, now called secondary follicles, increase in diameter, adding a new outer layer of connective tissue, blood vessels, and theca cells—cells that work with the granulosa cells to produce estrogens. Within the growing secondary follicle, the primary oocyte creates a thin acellular membrane called the zona pellucida. A thick fluid, called follicular fluid, collects in a space called the antrum.
Follicles with a large and fully formed antrum are considered tertiary follicles (also known as Graafian follicles). Most follicles don’t make it to this point. Usually only one follicle reaches the tertiary stage when it will release its secondary oocyte during ovulation. The rest of the developing follicles undergo atresia. Roughly 99 percent of the follicles in the ovary will undergo atresia, which can occur at any stage of folliculogenesis. After ovulation, the empty follicle is now called the corpus luteum. It will continue secreting progesterone and estrogens for the second half of the menstrual cycle (and longer if pregnancy happens that cycle).
See Figure 16.14[3] for an illustration of folliculogenesis.
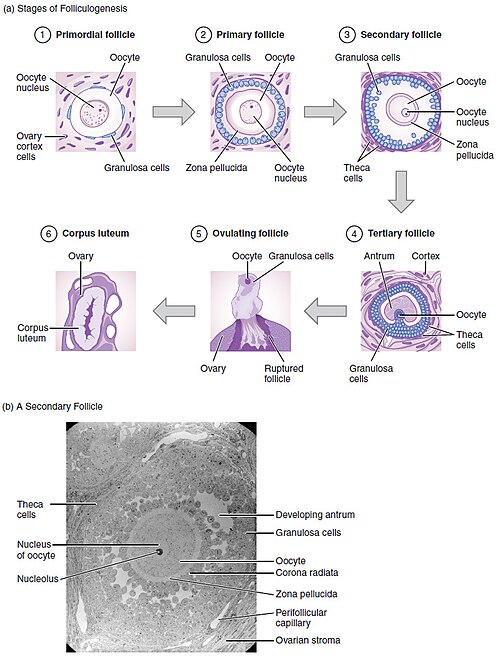
The process of development just described, from primordial follicle to early tertiary follicle, takes approximately two months in humans. The final stages of follicular development, ending with ovulation of a secondary oocyte, occur over a course of approximately 28 days.
Phases of the Ovarian Cycle
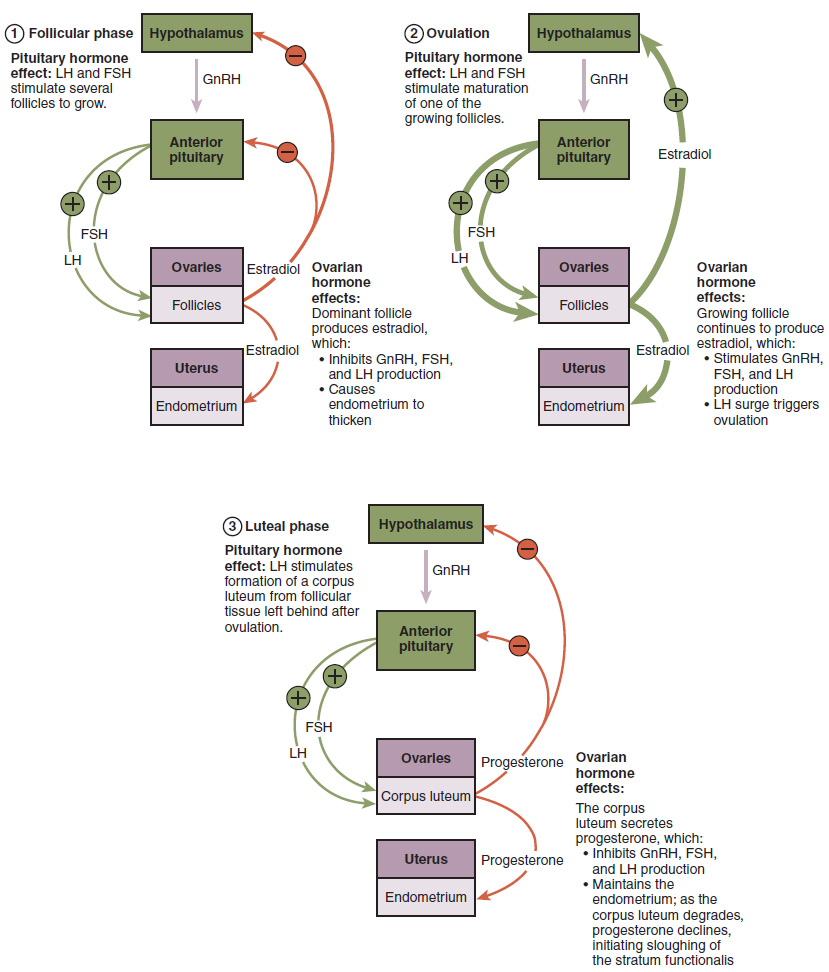
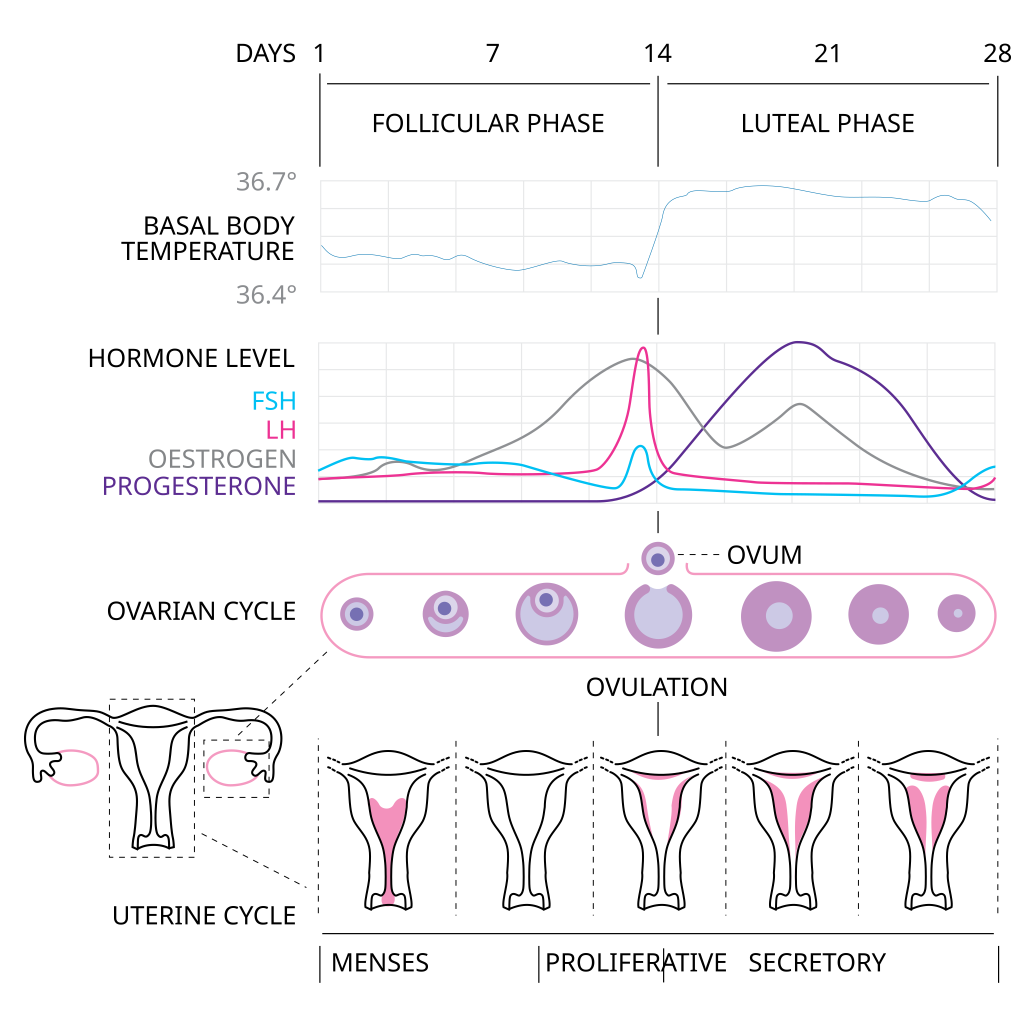
The ovarian cycle can be divided into three steps – the follicular phase, ovulation, and the luteal phase.
Follicular Phase
FSH stimulates the follicles to grow (hence the name “follicle-stimulating hormone”). The release of LH also stimulates the granulosa and theca cells of the follicles to produce estrogen. This phase of the ovarian cycle, when the follicles are growing and secreting estrogen, is known as the follicular phase. In this phase, the tertiary (antral) follicles (ovarian follicles with a primary or secondary oocyte, multiple layers of granulosa cells, and a fully formed antrum) are growing and secreting estrogen. The more granulosa and theca cells a follicle has (that is, the larger and more developed it is), the more estrogen it will produce in response to LH stimulation.
As a result of these large follicles producing large amounts of estrogen, systemic plasma estrogen concentrations increase. Following a classic negative feedback loop, the high concentrations of estrogen will stimulate the hypothalamus and anterior pituitary gland to reduce the production of GnRH, LH, and FSH. Because the large tertiary follicles require FSH to grow and survive at this point, this decline in FSH caused by negative feedback causes most of them to die (atresia).
Typically, only one follicle, now called the dominant follicle, will survive this reduction in FSH. This remaining follicle will be the one that releases an oocyte. Scientists have studied many factors that lead to a particular follicle becoming dominant. The size, the number of granulosa cells, and the number of FSH receptors on those granulosa cells all contribute to a follicle becoming the one surviving dominant follicle.
Ovulation
When only the one dominant follicle remains in the ovary, it again begins to secrete estrogen. It produces more estrogen than all of the developing follicles did together before the negative feedback occurred. It produces so much estrogen that the normal negative feedback doesn’t occur. Instead, these extremely high concentrations of systemic plasma estrogen trigger a regulatory switch in the anterior pituitary that responds by secreting large amounts of LH and FSH into the bloodstream. The positive feedback loop by which more estrogen triggers release of more LH and FSH only occurs at this point in the cycle.
It is this large burst of LH (called the LH surge) that leads to ovulation of the dominant follicle. The LH surge induces many changes in the dominant follicle, including stimulating the resumption of meiosis of the primary oocyte to a secondary oocyte. As noted earlier, the polar body that results from unequal cell division simply degrades. The LH surge also triggers proteases (enzymes that cleave proteins) to break down structural proteins in the ovary wall on the surface of the bulging dominant follicle. This degradation of the wall, combined with pressure from the large, fluid-filled antrum, results in the expulsion of the oocyte surrounded by granulosa cells into the peritoneal cavity. This release is ovulation.
The surge of LH also stimulates a change in the granulosa and theca cells that remain in the follicle after the oocyte has been ovulated. This change is called luteinization (recall that the full name of LH is luteinizing hormone), and it transforms the collapsed follicle into a new, temporary endocrine structure called the corpus luteum, a term meaning “yellowish body.” Instead of estrogen, the luteinized granulosa and theca cells of the corpus luteum begin to produce large amounts of the sex steroid hormone progesterone, a hormone that is critical for the establishment and maintenance of pregnancy. Progesterone triggers negative feedback at the hypothalamus and pituitary, which keeps GnRH, LH, and FSH secretions low, so no new dominant follicles develop at this time.
Luteal Phase
The postovulatory phase of progesterone secretion is known as the luteal phase of the ovarian cycle. If pregnancy does not occur within 10 to 12 days, the corpus luteum will stop secreting progesterone and degrade into the corpus albicans, a nonfunctional “whitish body” that will disintegrate in the ovary over a period of several months. During this time of reduced progesterone secretion, FSH and LH are once again stimulated, and the follicular phase begins again with a new cohort of early tertiary follicles beginning to grow and secrete estrogen.
View a supplementary YouTube video[4] on the ovaries and the ovarian cycle: How Does the Ovarian Cycle Work?
See Figure 16.15[5] for an illustration of the hormonal regulation of ovulation.
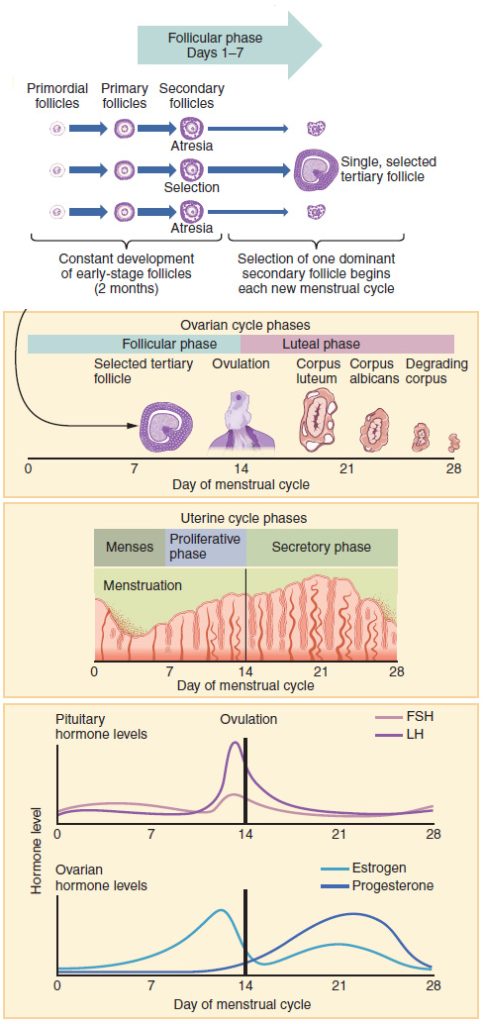
Menstrual (Uterine) Cycle
The menstrual (uterine) cycle starts with the first day of menstruation, referred to as day one of the menstrual cycle. The average length of a menstrual cycle is 28 days, but this varies between individuals and even in the same person from one cycle to the next, typically lasting anywhere from 21 to 32 days. There are three distinct phases of the menstrual cycle called the menstrual phase, the proliferative phase, and the secretory phase. These phases happen in the uterus while the oocyte is developing simultaneously in the ovaries.
Menstrual (Menses) Phase
The menstrual phase of the menstrual cycle is when the stratum functionalis of the uterus is shed, also known as menstruation. Menstruation occurs for an average of about five days but can last from two to seven days, or even longer.
The menses phase occurs during the early days of the follicular phase of the ovarian cycle, when progesterone, estrogen, FSH, and LH levels are low. These low levels of hormones cause tiny arterioles in the uterus to constrict, cutting off oxygen to the stratum functionalis. The stratum functionalis then dies and is shed as the menstrual period.
Proliferative Phase
Once menstrual flow stops, the endometrium begins to grow (proliferate) again, marking the beginning of the proliferative phase of the menstrual cycle. FSH and LH stimulate the growth of several follicles in the ovaries, and the follicles begin to secrete increased amounts of estrogen, stimulating the endometrial lining to rebuild. Ovulation marks the end of the proliferative phase.
Secretory Phase
In the secretory phase, the hormone progesterone (secreted by the corpus luteum) finishes maturing the endometrial lining for the possible implantation of a fertilized egg. Spiral arteries develop and provide blood to the thickened stratum functionalis. The endometrial glands secrete a glycogen rich fluid that will nourish an embryo if fertilization occurs. High levels of estrogen increase Fallopian tube contractions to help move the ovulated oocyte toward the uterus. Estrogen also decreases the acidity of the vagina, making it more hospitable to sperm.
If fertilization does not occur, the corpus luteum will degenerate into the corpus albicans and will no longer be able to secrete hormones to sustain the stratum functionalis. The levels of both estrogen and progesterone will fall. Prostaglandins will be secreted, causing constriction of the spiral arteries. This reduces the oxygen supply to the stratum functionalis layer, which will die and is shed, resulting in menstruation—or the first day of the next cycle.
See Figures 16.16[6] and 16.17[7] for illustrations of hormone levels in the ovarian and menstrual cycles.
View a supplementary YouTube video[8] on the menstrual cycle: Menstrual Cycle Walkthrough: Phases & Hormonal Regulation.
Menopause
Menopause is the cessation of the menstrual cycle as a result of the loss of ovarian follicles and the hormones that they produce. Female fertility (the ability to conceive) peaks when women are in their 20s and slowly declines until 35 years of age. After that time, fertility declines more rapidly, until it ends completely at the end of menopause.
Menopause is considered complete if a person has not menstruated for a full year. After that point, they are considered postmenopausal. The average age of menopause worldwide is between the ages of 50 and 52 but can occur any time between 40 and 60. Poor health, including smoking, can lead to earlier loss of fertility and earlier menopause.
As the age of menopause approaches, the decreasing number of follicles in the ovaries affects the hormonal regulation of the menstrual cycle. In the years leading up to menopause, there is a decrease in the hormone inhibin, which leads to an increase in FSH. This increase in FSH stimulates more follicles to grow and secrete estrogen. Because small, secondary follicles also respond to increases in FSH levels, larger numbers of follicles are stimulated to grow but most undergo atresia and die. Eventually, this process leads to the depletion of all follicles in the ovaries, and the production of estrogen falls dramatically. It is primarily the lack of estrogens that leads to the symptoms of menopause.
The earliest changes occur during the menopausal transition, often referred to as perimenopause, when a menstrual cycle becomes irregular but does not stop entirely. As estrogen levels change, other symptoms that occur are hot flashes and night sweats; trouble sleeping; vaginal dryness; mood swings; difficulty focusing; and thinning of hair on the head, along with the growth of more hair on the face. Depending on the individual, these symptoms can be entirely absent, moderate, or severe. Hormone therapy (synthetic estrogen and progesterone) may be prescribed to increase estrogen and progesterone levels and alleviate some of the symptoms of menopause.
After menopause, lower amounts of estrogen can lead to other changes. Cardiovascular disease becomes as prevalent in females as in males, possibly because estrogens reduce the amount of cholesterol in the blood vessels. When estrogen is lacking, many women find they suddenly have high cholesterol and associated cardiovascular issues. Osteoporosis may also occur because bone density decreases rapidly in the first years after menopause. The reduction in bone density leads to a higher incidence of fractures.
- “Figure_28_02_03” by OpenStax College is licensed under CC BY 3.0 ↵
- Visible Body. (2021, October 4). Oogenesis: Learn@Visible Body [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=-s7a3ffuckQ ↵
- “Figure_28_02_04” by OpenStax College is licensed under CC BY 3.0 ↵
- Visible Body. (2023, October 24). How does the ovarian cycle work? [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=l6IQyVIFA7w How Does the Ovarian Cycle Work? ↵
- “Figure_28_02_05” by OpenStax College is licensed under CC BY 3.0 ↵
- “Figure_28_02_07” by OpenStax College is licensed under CC BY 3.0 ↵
- “Menstrual_cycle.svg” by Isometrik, Kaldari; Begoon; Marnanel is licensed under CC BY-SA 3.0 ↵
- Amoeba Sisters. (2025, February 27). Menstrual cycle walkthrough: Phases & hormonal regulation [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=h36poEtEbi4 ↵
The start of menstruation.
Physical characteristics that are influenced by estrogen and are important for reproductive function.
A hormone secreted by the hypothalamus that stimulates the anterior pituitary to secrete follicle stimulating hormone (FSH) and luteinizing hormone (LH).
A gonadotropin that promotes the production and development of sex cells (ova in females and sperm in males).
A gonadotropin that triggers ovulation in females and stimulates testosterone production in males.
Hormones produced by the ovaries, including estradiol, estriol, and estrone, that regulate the reproductive system, menstrual cycle, female secondary sex traits, and pregnancy.
A hormone from the ovaries that helps regulate the menstrual cycle and supports pregnancy preparation and maintenance.
The production of an ovum (egg).
Ovarian stem cells formed during fetal development.
Immature egg cells that are arrested in prophase I of meiosis and remain dormant until puberty, when they may resume development during the menstrual cycle.
The ending of a female's reproductive functions.
The release of an oocyte from the ovary.
A mature egg cell produced after meiosis I that is released during ovulation and will complete meiosis II only if fertilization occurs.
A small cell produced during oogenesis that contains little cytoplasm and typically disintegrates, ensuring most resources go to the developing oocyte.
The process by which ovarian follicles grow and develop, usually resulting in ovulation of one oocyte and the degeneration of the others.
The death of ovarian follicles.
The earliest and most immature ovarian follicles, consisting of a primary oocyte surrounded by a single layer of flat supporting cells.
A single flat layer of support cells that surround the oocyte and can stay in this resting state for years—some until right before menopause.
Single layer of granulosa cells, but they become active, increase in size, and proliferate.
Follicles that have grown larger with dividing granulosa cells and an added outer layer of connective tissue, blood vessels, and theca cells that help produce estrogens.
Cells that work with the granulosa cells to produce estrogens.
Acellular membrane surrounding the oocyte that protects it and plays a key role in sperm binding during fertilization.
A fluid-filled cavity that forms within a developing ovarian follicle.
A temporary endocrine structure formed from the ruptured follicle after ovulation that secretes progesterone to support pregnancy.
The phase of the ovarian cycle when the follicles are growing and secreting estrogen.
Starts with the first day of menstruation, referred to as day one of the menstrual cycle.
Phase of the menstrual cycle when the stratum functionalis of the uterus is shed, also known as menstruation.
A phase characterized by growth and multiplication of cells to build new tissue, occurring in processes such as the menstrual cycle or wound healing.
A scar-like structure formed when the corpus luteum degenerates if pregnancy does not occur.
The stage after menopause when menstruation has ceased permanently.
The earliest changes occur during the menopausal transition when a menstrual cycle becomes irregular but does not stop entirely.

