16.4 Male Puberty and Spermatogenesis
Male Puberty and Spermatogenesis
Puberty is the stage of development when individuals become sexually mature. Though the outcomes of puberty for males and females are very different, the hormonal control of the process is very similar. In addition, though the timing of these events varies between individuals, the sequence of changes that occur is predictable for adolescents.
Male Reproductive Hormones
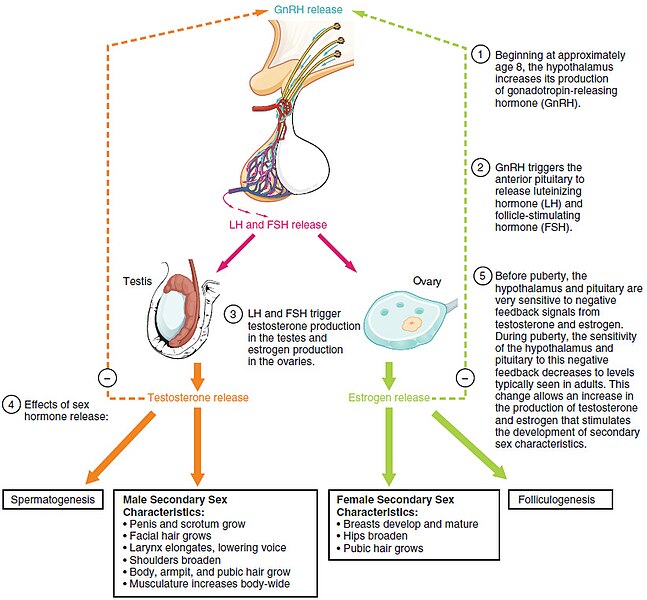
The onset of puberty is controlled by hormones. The hypothalamus begins to secrete a hormone called gonadotropin releasing hormone (GnRH). This hormone stimulates the anterior pituitary gland to secrete follicle stimulating hormone (FSH) and luteinizing hormone (LH). The first changes begin around the age of eight or nine when the production of LH becomes detectable. The release of LH occurs primarily at night during sleep and precedes the physical changes of puberty by several years.
As an individual approaches puberty, the levels of LH and FSH slowly increase and lead to the enlargement and maturation of the testes. LH stimulates the Leydig cells to secrete higher levels of testosterone, and FSH stimulates the Sertoli cells to begin spermatogenesis (sperm production).
Secondary Sex Characteristics
The increasing levels of testosterone also cause the development of secondary sex characteristics. In males, the growth of the testes is typically the first physical sign of the beginning of puberty, which is followed by growth and increased pigmentation of the scrotum and growth of the penis. The next step is the growth of hair, including armpit, pubic, chest, and facial hair. Testosterone stimulates the growth of the larynx and thickening and lengthening of the vocal folds, which causes the voice to deepen or drop in pitch. The first fertile ejaculations typically appear at approximately 15 years of age, but this age can vary widely across individuals. The male growth spurt occurs throughout puberty, at approximately age 11 to 13, and height can increase as much as four inches in a year. In some individuals, pubertal development can continue through the early 20s.
In addition to age, multiple factors can affect the age of onset of puberty, including genetics, environment, psychological stress, and nutrition. Some studies indicate a link between puberty onset and the amount of stored fat in an individual. This effect is more pronounced in females but has been documented in both sexes.
See Figure 16.6[1] for an illustration of the hormones of puberty.
Spermatogenesis
Spermatogenesis, the production of sperm, occurs in the seminiferous tubules. Spermatogenesis begins at puberty and continues throughout life. The production of sperm from a spermatogonium to a mature sperm takes approximately 64 days. The number of sperm produced per day varies from 100,000 to 300,000. Sperm counts slowly decline after the age of 35, and some studies suggest that smoking can lower sperm counts at any age.
The process of spermatogenesis uses two types of cell division, mitosis and meiosis. Mitosis is the division of a somatic cell (all the cells in the body except the sperm and ovum) into two identical daughter cells, each with 46 chromosomes.
Meiosis is a special type of cell division that occurs only in the sperm and ovum. It requires two rounds of division (prophase, anaphase, metaphase, and telophase) with no interphase between round one (Meiosis I) and round two (Meiosis II). An exchange of genes between chromosomes called “crossing over” occurs during Prophase I, the beginning of meiosis, resulting in a new combination of genes. The two rounds of division result in four genetically unique daughter cells with 23 chromosomes in each cell.
Step I: Mitosis of the Spermatogonia
The process of spermatogenesis begins with mitosis of the spermatogonia (sperm-producing stem cells). Because spermatogonia are diploid (2n), they have 46 total chromosomes arranged in 23 pairs of chromosomes. A copy of these chromosomes is made during interphase so that when the spermatogonia divide, the new cells will have the same number of chromosomes as the original cell. The division of the spermatogonia by mitosis results in two identical diploid spermatogonium cells, each with 46 chromosomes.
One of these two cells remains a spermatogonium, and the other differentiates or passes through the blood testis barrier and becomes a primary spermatocyte.
Step II – Meiosis I
DNA is replicated again during interphase in a primary spermatocyte, so the cell starts Meiosis I with 46 chromosomes and a copy of those 46 chromosomes. The primary spermatocyte goes through Prophase I, Metaphase I, Anaphase I, and Telophase I to divide, resulting in two cells called secondary spermatocytes. Each secondary spermatocyte now has half the number of chromosomes or 23 chromosomes. No replication of DNA occurs between Meiosis I and Meiosis II, and the two secondary spermatocytes go directly into Meiosis II.
Step III: Meiosis II
The two secondary spermatocytes begin Meiosis II with 23 total chromosomes in each cell. They both go through Prophase II, Metaphase II, Anaphase II, and Telophase II to divide, resulting in four haploid cells with 23 chromosomes in each cell. Each of these new haploid cells is called a spermatid.
See Figure 16.7[2] for an overview of spermatogenesis.
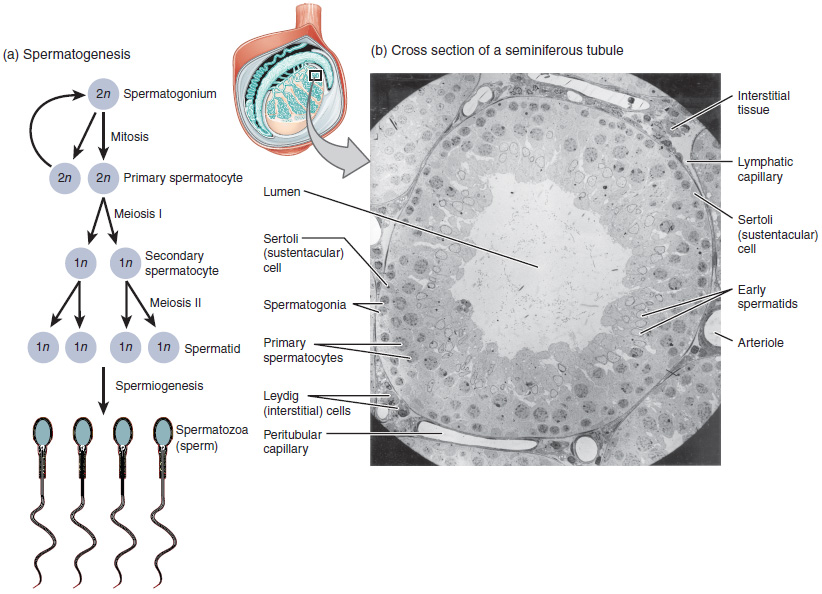
Spermiogenesis
A process called spermiogenesis transforms these early spermatids, beginning the formation of the parts of a true sperm. Spermatozoa, or formed sperm, are the end result of this process. Eventually, the sperm are released into the lumen and travel to the epididymis to mature.
Sperm
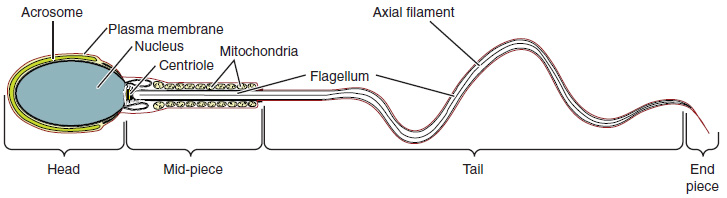
Sperm are smaller than most cells in the body; in fact, the size of a sperm cell is 85,000 times smaller than that of the ovum. Sperm have a distinctive head, midpiece, and tail region.
The head of the sperm contains the nucleus and DNA. A structure called the acrosome covers most of the head of the sperm cell as a “cap” that is filled with lysosomal enzymes important for the sperm to penetrate an egg. Mitochondria fill the midpiece of the sperm. ATP produced by these mitochondria will power the flagellum, which extends from the midpiece through the tail of the sperm, enabling it to move the entire sperm cell. See Figure 16.8[3] for an illustration of the structure of a sperm cell.
- “Figure_28_03_01” by OpenStax College is licensed under CC BY 3.0 ↵
- “Figure_28_01_04” by OpenStax College is licensed under CC BY 3.0 ↵
- “63e4c7b77be4e97c88b4c649fbd6c6472cf58466” by OpenStax College is licensed under CC BY 4.0. https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
The stage of development when individuals become sexually mature.
The process that begins with spermatogonia and ends with mature sperm.
A process of nuclear division that results in two identical daughter cells with the same number of chromosomes as the parent cell.
A special type of cell division that occurs only in the sperm and ovum.
Undergoes a process of development to become a more specialized cell type.
A diploid male germ cell that undergoes the first meiotic division to form secondary spermatocytes.
Haploid cells produced from the first meiotic division of primary spermatocytes that quickly undergo the second meiotic division to form spermatids.
New haploid cells.
A process that transforms early spermatids, beginning the formation of the parts of a true sperm.
Formed sperm.
A cap-like structure on the head of a sperm cell containing enzymes that help the sperm penetrate the egg during fertilization.
A long, whip-like tail that enables a sperm cell to swim.

