14.5 Digestive System Disorders
Digestive System Disorders
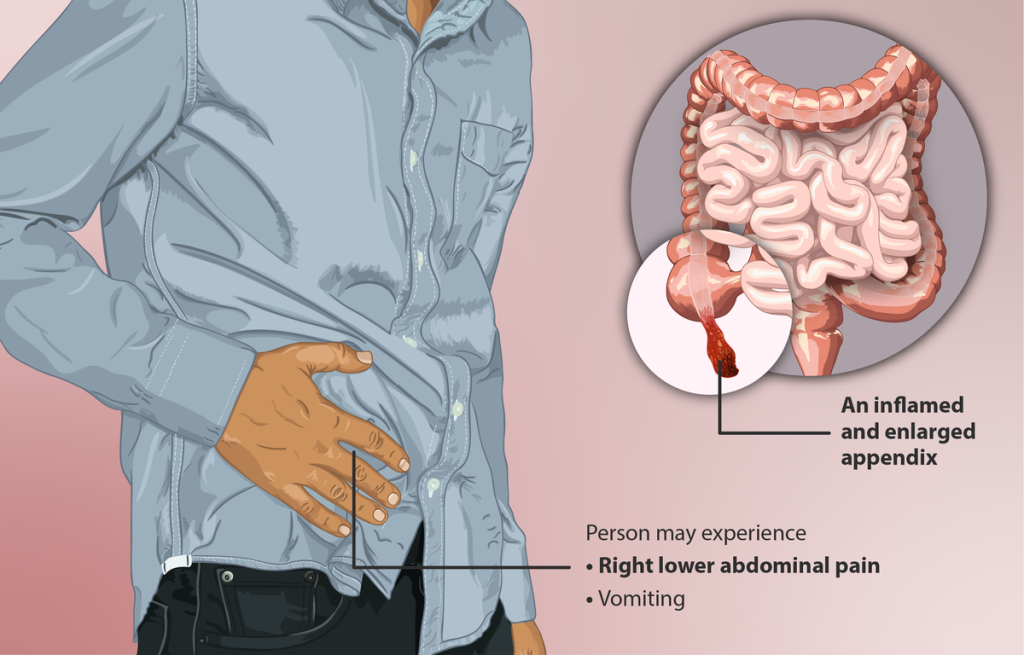
Appendicitis[1]
Appendicitis is a condition in which the appendix becomes inflamed and is a common reason for emergency surgery. Appendicitis occurs when the appendix becomes blocked by feces, a foreign object, a tumor, or, in rare cases, a parasite.
The symptoms of appendicitis can vary. It can be difficult to detect appendicitis in young children, older people, and women of childbearing age. The first symptom is often pain around the navel or mid-upper abdomen. Pain may be minor at first, but becomes more sharp, severe, and localized to the right lower quadrant. The pain focuses on a spot directly above the appendix, called McBurney’s point. This most often occurs 12 to 24 hours after the illness starts. Pain may be worse when walking, coughing, or making sudden movements. There may also be a loss of appetite, nausea, vomiting, and a low-grade fever.
Typically, the appendix is surgically removed as soon as appendicitis is diagnosed. If a CT scan shows an abscess, treatment with antibiotics may occur first, and the appendix will be removed after the infection and swelling have gone away.
See Figure 14.24[2] for an illustration of appendicitis.
Celiac Disease[3]
Celiac disease is an inherited autoimmune disorder that causes the immune system to produce antibodies against the gluten protein. These antibodies damage the mucosal lining of the small intestine, impairing its ability to absorb nutrients from food, resulting in nutritional deficiencies and weight loss. Other common symptoms are diarrhea, abdominal distension or bloating, and nausea and vomiting after consuming food that contains gluten.
Celiac disease is most commonly found in people of Northern European descent and affects 1% of the European and North American population. There is a 10% chance of developing the disease if it is present in a first-degree relative, such as a parent. About 97% of people diagnosed with celiac disease have a gene variant associated with it.
Celiac disease is also more prevalent in people with certain inherited chromosomal disorders, such as Down syndrome. It’s also more frequently seen in people with other autoimmune diseases because these diseases often share similar genes and trigger each other. Like other autoimmune diseases, celiac disease is more common in females than males, with the ratio of affected females to males being at least 2:1.
Gluten is a protein found in grains — particularly wheat, barley, and rye. These grains, especially wheat, make up many of the staple foods of the standard Western diet and are found in breads, cereals, pasta, baked goods, and even beer. Gluten is also a common additive in sauces, soups, and packaged foods. The primary treatment for individuals with celiac disease is adhering to a gluten-free diet.
Cirrhosis[4],[5],[6]
Cirrhosis is advanced scarring of the liver commonly caused by hepatitis or alcoholism. Each time the liver is injured — whether by alcohol or infection — it tries to repair itself. In the process, scar tissue forms. As cirrhosis worsens, more scar tissue forms that decreases the liver’s ability to function. Advanced cirrhosis is life-threatening. See Figure 14.25[7] for an image of a liver damaged by cirrhosis.
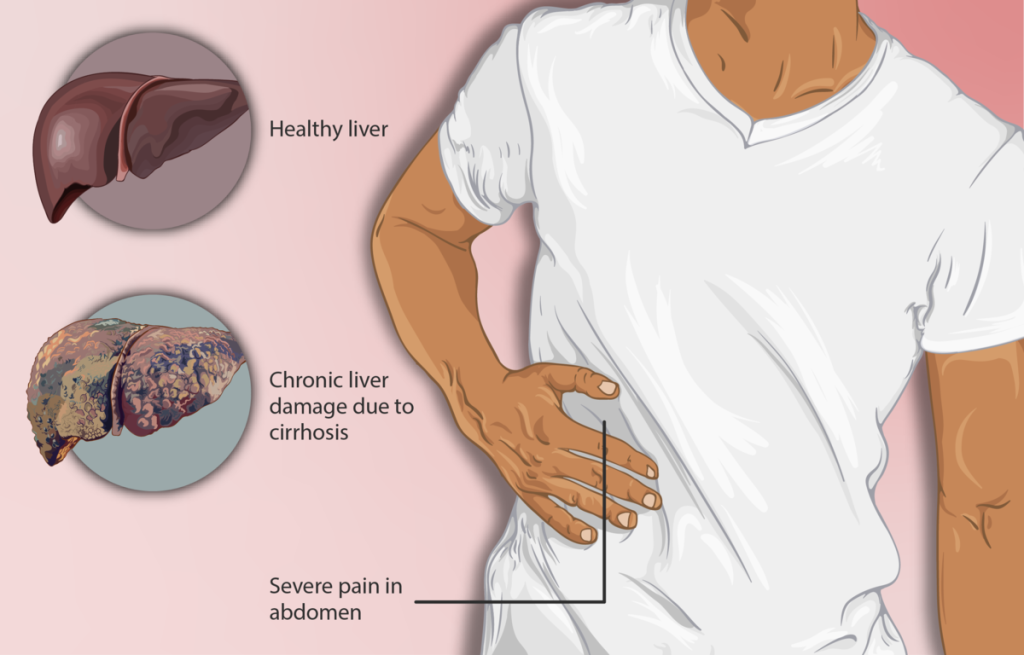
Individuals with cirrhosis may or may not have symptoms depending on the severity of the condition. Common symptoms are an enlarged liver, jaundice (yellowing of the skin and eyes), ascites (accumulation of fluid in the abdominal cavity), and bleeding varices (enlarged veins caused by increased pressure in the portal vein of the liver).
The liver damage caused by cirrhosis generally can't be reversed, but if cirrhosis is diagnosed early and the underlying cause is treated, further damage can be prevented. In some cases, liver transplantation may be a treatment option.
Cholelithiasis[8]
The medical condition of having gallstones is cholelithiasis. A gallstone is a piece of hardened bile residue that can form for a variety of reasons, including elevated cholesterol levels. Gallstones are often asymptomatic, but when a gallstone gets stuck in a bile duct, it can cause bile to back up into the gallbladder, causing sudden severe upper right abdominal pain, back pain, nausea, vomiting, and fever. To remove gallstones, a surgical procedure called an endoscopic retrograde cholangiopancreatography (ERCP) may be performed. See Figure 14.26[9] for an image of a gallstone in the gallbladder on an ultrasound.

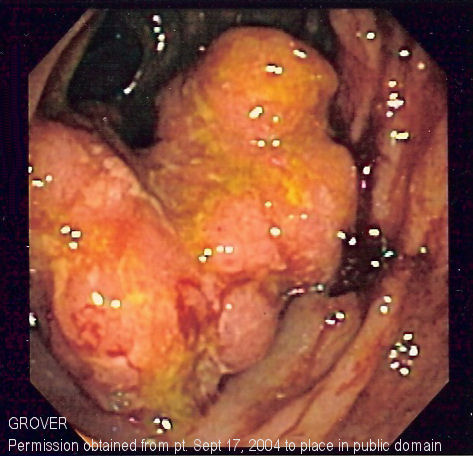
Colorectal Cancer[10],[11]
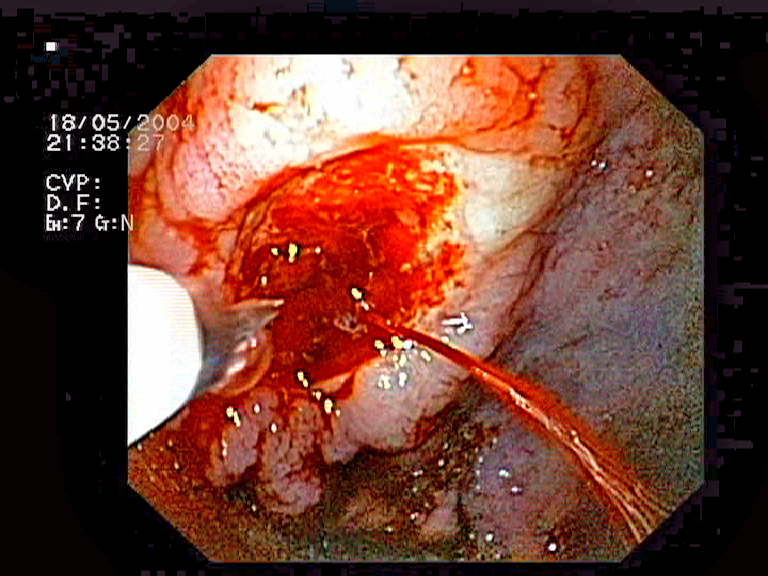
Each year, approximately 140,000 Americans are diagnosed with colorectal cancer, and another 49,000 die from it, making it one of the deadliest cancers. A family history of colorectal cancer, smoking, excessive alcohol consumption, and a diet high in animal fat and protein increase the risk for colorectal cancer. Screening for colorectal cancer is recommended at 45 years of age for people who have an average risk of developing colorectal cancer. For those considered high risk for colorectal cancer, screenings may start younger. Screening is performed using stool tests and colonoscopy.
Colorectal cancer may be asymptomatic in its early stages or include symptoms such as rectal bleeding or unusual constipation, diarrhea, or abdominal pain. Rectal bleeding may be obvious or occult (hidden in feces). Most colon cancers arise from benign mucosal growths called polyps, so cancer prevention is focused on identifying these polyps early via colonoscopy. A colonoscopy not only allows identification of precancerous polyps but also enables them to be removed before they become malignant. See Figure 14.27[12] for an image depicting colorectal cancer detected via colonoscopy.
Crohn’s Disease[13],[14]
Crohn's disease is a type of inflammatory bowel disease (IBD) that causes swelling and irritation of the tissues in the digestive tract. This inflammation can lead to abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition. Inflammation caused by Crohn's disease can affect different areas of the digestive tract in different people. Crohn's most commonly affects the end of the small intestine and the beginning of the large intestine. The inflammation often spreads into the deeper layers of the bowel. In some cases, the inflammation of Crohn’s disease can also be systemic and lead to inflammation of the eyes, kidneys, liver, skin, and joints. Crohn's disease can be both painful and debilitating. Sometimes, it may lead to serious or life-threatening complications.
There's no known cure for Crohn's disease, but medical treatment can greatly reduce its symptoms and bring about long-term remission of symptoms and healing of inflammation.
Diarrhea[15]
Diarrhea is a common problem with frequent passage of loose or watery stool. It may be associated with other symptoms, such as nausea, vomiting, abdominal pain, or weight loss.
A number of diseases and conditions can cause diarrhea, including the following:
- Viruses: Viruses that can cause diarrhea include Norwalk virus, also known as norovirus, enteric adenoviruses, astrovirus, cytomegalovirus, and viruses that cause hepatitis. Rotavirus is a common cause of sudden childhood diarrhea. The virus that causes coronavirus disease (COVID-19) also has been linked to gastrointestinal symptoms, including nausea, vomiting, and diarrhea.
- Bacteria and parasites: Exposure to certain bacteria, such as Escherichia coli, or parasites through contaminated food or water can lead to diarrhea. When traveling in developing countries, diarrhea caused by bacteria or parasites is often called traveler's diarrhea. Clostridium difficile, also known as C. diff, is another bacterium that causes diarrhea, and it can occur after a course of antibiotics or during a hospital stay.
- Medications: Many medications, such as antibiotics, can cause diarrhea. Antibiotics get rid of infections by killing bacteria that cause illness, but they also kill good bacteria that are helpful in the body. This disturbs the natural balance of bacteria in the intestines, leading to diarrhea or an infection such as C. diff. Other medicines that cause diarrhea are anticancer drugs and antacids with magnesium.
- Lactose intolerance: Lactose is a sugar found in milk and other dairy products. People who have trouble digesting lactose often have diarrhea after eating dairy products. Lactose intolerance can increase with age because levels of the enzyme that helps digest lactose become lower as people get older.
- Fructose: Fructose is a sugar found naturally in fruits and honey. It's sometimes added as a sweetener to certain beverages. Fructose can lead to diarrhea in people who have trouble digesting it.
- Artificial sweeteners: Sorbitol, erythritol and mannitol — non absorbable sugars used as artificial sweeteners in chewing gum and other sugar-free products — can cause diarrhea in some otherwise healthy people.
- Surgery: Partial intestine or gallbladder removal surgeries can sometimes cause diarrhea.
- Other digestive disorders: Chronic diarrhea has a number of other causes, such as IBS, Crohn's disease, ulcerative colitis, celiac disease, microscopic colitis, and small intestinal bacterial overgrowth (SIBO).
Diverticulosis and Diverticulitis[16],[17],[18]
Diverticulosis is a condition that occurs when small pouches, or sacs, form and push outward through weak spots in the wall of the colon. These pouches form mostly in the lower part of the colon, called the sigmoid colon. One pouch is called a diverticulum. Multiple pouches are called diverticula. Most people who have diverticula in their colon do not have symptoms or problems. Diverticulosis is quite common, especially as people age. More than 30% of U.S. adults between the ages of 50 and 59 and more than 70% of those older than age 80 have diverticulosis. Most people with diverticulosis will never develop symptoms or problems.
Diverticulitis occurs when diverticula become inflamed. Diverticulitis can come on suddenly and may lead to serious complications. Less than 5% of people with diverticulosis develop diverticulitis.
Most people first notice symptoms when they develop complications, such as diverticular bleeding or diverticulitis. Some people have chronic symptoms related to diverticula, even when diverticulitis is not present. Chronic symptoms may include bloating, constipation or diarrhea, and cramping or pain in the lower abdomen.
Diverticulitis may cause acute symptoms such as abdominal pain, most often in the lower left side of the abdomen, constipation or diarrhea, fevers and chills, and nausea or vomiting. The pain caused by diverticulitis is typically severe and comes on suddenly, although the pain may also be mild and worsen over several days. The intensity of the pain may change over time.
Treatments are based on whether an individual has chronic symptoms of diverticula, diverticulitis, or other complications of diverticular disease.
Gastroenteritis[19]
Gastroenteritis is an inflammation of the lining of the stomach and intestines. The main symptoms include vomiting and diarrhea. It is usually not serious in healthy people, but it can sometimes lead to dehydration or cause severe symptoms. There can be many different causes of gastroenteritis, including viruses, bacteria, parasites, chemicals, and reactions to certain medications and food
Viral gastroenteritis is the most common type. It can be caused by many different viruses, including noroviruses and rotaviruses. Some people call viral gastroenteritis the "stomach flu." But this name is not medically correct. It is not caused by flu viruses. The flu is a respiratory infection that affects your nose, throat, and lungs. When gastroenteritis is caused by consuming foods or drinks contaminated with viruses, bacteria, parasites, or chemicals, this is called food poisoning.
The viruses, bacteria, and parasites that cause gastroenteritis can also spread from person to person or picked up when touching something that has the germs on it and then touching the eyes, mouth, or nose.
The symptoms of gastroenteritis include diarrhea, pain or cramping in the abdomen, nausea, vomiting, and sometimes fever. Usually, people with gastroenteritis get better on their own, with rest and plenty of fluids and electrolytes.
Gastroesophageal Reflux Disease (GERD)[20]
Gastroesophageal reflux disease (GERD) is a condition in which stomach acid repeatedly flows back up into the esophagus due to an incompetent lower esophageal sphincter, as shown in Figure 14.28.[21] This backflow is known as acid reflux, and it can irritate the lining of the esophagus.
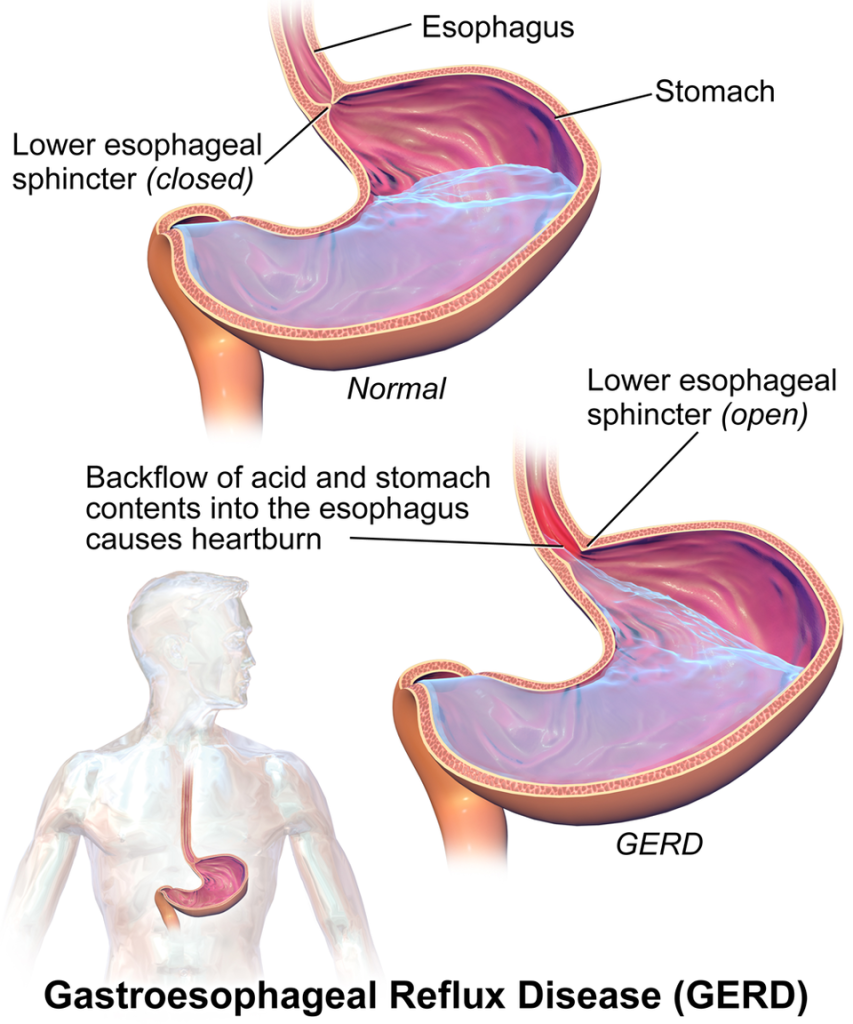
Common symptoms of GERD include a burning sensation in the chest, often called heartburn, backflow of food or sour liquid in the throat, upper abdominal or chest pain, trouble swallowing (dysphagia), and a sensation of a lump in the throat. Heartburn usually happens after eating and might be worse at night or while lying down. Nighttime acid reflux might also cause an ongoing cough, inflammation of the vocal cords (laryngitis), and new or worsening asthma.
Conditions that can increase the risk of GERD include obesity; bulging of the top of the stomach up above the diaphragm (hiatal hernia); pregnancy; connective tissue disorders, such as scleroderma; and delayed stomach emptying. Factors that can aggravate acid reflux include smoking, eating large meals or eating late at night, eating fatty or fried foods, drinking alcohol or coffee, and taking certain medicines such as aspirin. Most people can manage the discomfort of GERD with lifestyle changes and medications, although some may require surgery on the lower esophageal sphincter.
Hemorrhoids[22]
Hemorrhoids, also called piles, are swollen veins in the anus and lower rectum. Hemorrhoids can develop inside the rectum, called internal hemorrhoids. Hemorrhoids can also develop under the skin around the anus, called external hemorrhoids. See Figure 14.29[23] for a depiction of internal versus external hemorrhoids.
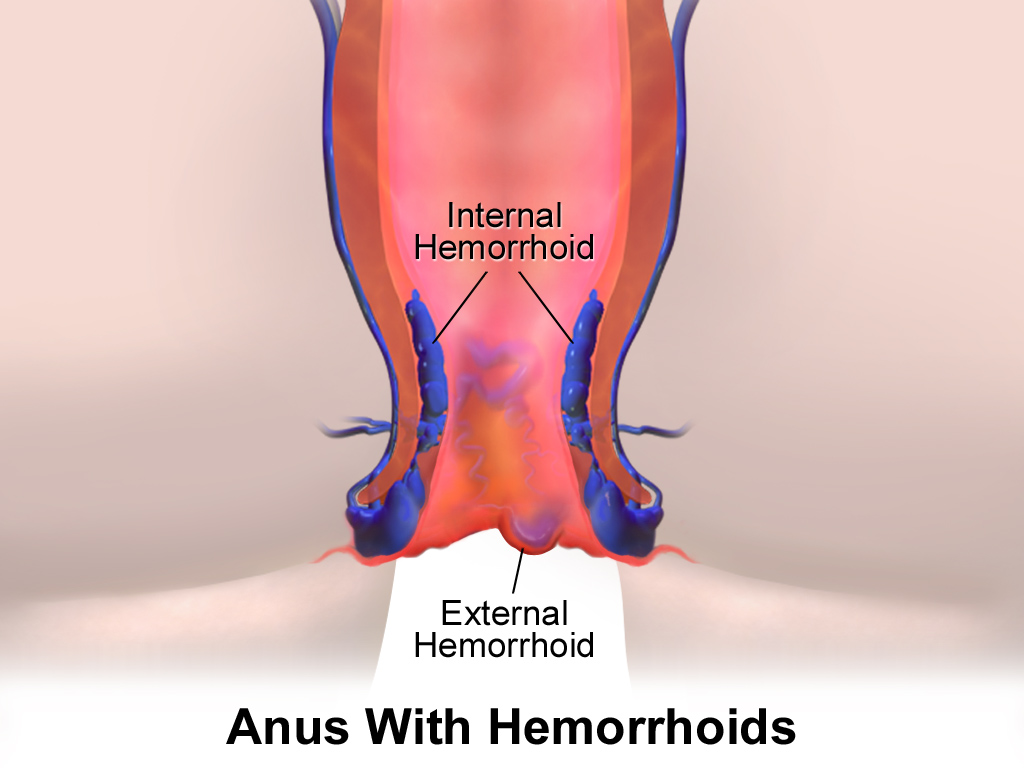
Symptoms of hemorrhoids may include itching or irritation in the anal region, pain or discomfort, swelling around the anus, and bleeding. If bleeding occurs, it can pool in an external hemorrhoid and form a clot, called a thrombosed hemorrhoid. Thrombosed hemorrhoids can result in severe pain; swelling; inflammation; and a hard, discolored lump near the anus.
Hemorrhoids can develop from increased pressure in the lower rectum due to straining during bowel movements; sitting for long periods of time, especially on the toilet; having chronic diarrhea or constipation; being obese; being pregnant; or having anal intercourse. As people age, the risk of hemorrhoids increases because the tissues that support the veins in the rectum and anus can weaken and stretch. This stretching can also happen during pregnancy because there is added pressure on the anal region.
There are several options available to treat hemorrhoids, including lifestyle changes and medications. However, if conservative management is not effective or a thrombosed hemorrhoid occurs, surgical treatment may be needed.
Hepatitis[24],[25]
Hepatitis refers to inflammation of the liver. When the liver is inflamed or damaged, it cannot do its job effectively. Heavy alcohol use, toxins, some medications, and certain medical conditions can cause hepatitis. However, hepatitis is often caused by one of the hepatitis viruses that can range from mild to severe, with many people not realizing they are infected. Nonspecific signs and symptoms include poor appetite, nausea, vomiting, and fatigue that progress to specific signs of liver dysfunction such as jaundice, clay-colored stools, dark urine, abdominal pain, and enlargement of the liver.
Tens of thousands of people are newly infected with viral hepatitis every year in the US. The most common types of viral hepatitis are hepatitis A, hepatitis B, and hepatitis C:
- Hepatitis A: Hepatitis A is caused by the hepatitis A virus (HAV). It spreads through close person-to-person contact or by eating or drinking contaminated food or drink and typically causes a mild, short-term illness. Vaccination is the best way to prevent infection.
- Hepatitis B: Hepatitis B is caused by the hepatitis B virus (HBV) and spreads through infected body fluids. Infection can result in acute (short-term) or chronic (long-term) illness. Vaccination is the best way to prevent infection.
- Hepatitis C: Hepatitis C is caused by the hepatitis C virus (HCV) and spreads through infected body fluids. It is commonly caused by sharing contaminated needles during illicit drug use. Many people with hepatitis C don't look or feel sick, so they might not know they have the virus. If left untreated, hepatitis C can lead to serious liver problems, like damage, scarring, or cancer. There is no vaccine for hepatitis C, but it can be treated with oral medication.
Irritable Bowel Syndrome (IBS)[26],[27],[28]
Irritable bowel syndrome (IBS) is a group of gastrointestinal symptoms that include changes in bowel movements, such as chronic diarrhea, constipation, or both. These symptoms occur without visible signs of damage or disease in the digestive tract. There is no known cause of IBS, but psychological stress may contribute to the development of IBS. Irritable bowel syndrome (IBS) is treated with diet and lifestyle changes, medications, probiotics, and mental health counseling.
Jaundice[29]
Jaundice, also called icterus, causes the skin and the whites of the eyes to turn yellow. See Figure 14.30[30] for an image of a patient with jaundice. The condition is caused by too much bilirubin, a yellow chemical from the breakdown of hemoglobin. As red blood cells break down, they are processed by the liver. However, if the liver cannot process these cells effectively, bilirubin levels build up in the body and cause jaundice.

Many healthy babies have a form of jaundice during the first week of life that typically resolves on its own. The cause of this type of jaundice is due to their immature livers. Premature babies are more likely to be jaundiced and may need light therapy to treat it. Other types of jaundice can occur at any age and can indicate a liver disorder or other medical disorder. Conditions that can cause jaundice include liver disease like hepatitis or cirrhosis, blockage of bile ducts, blood disorders, genetic syndromes, infections, and side effects of certain medications.
Lactose Intolerance[31]
Lactose intolerance is a condition characterized by an inability to digest lactose, the sugar found in dairy products. It occurs when the absorptive cells of the small intestine do not produce enough lactase, the enzyme that digests the milk sugar lactose. In most mammals, the incidence of lactose intolerance increases with age. In contrast, some human populations are able to maintain the ability to produce lactase as adults.
In people experiencing lactose intolerance, the lactose in chyme is not digested. Bacteria in the large intestine ferment the undigested lactose and produce gas. In addition to gas, symptoms include abdominal cramps, bloating, and diarrhea. Symptom severity ranges from mild discomfort to severe pain, but symptoms resolve once the lactose is eliminated.
The hydrogen breath test is used to help diagnose lactose intolerance. Lactose-tolerant people have very little hydrogen in their breath. Those with lactose intolerance exhale hydrogen, which is one of the gases produced by the bacterial fermentation of lactose in the colon. After the hydrogen is absorbed from the intestine, it is transported through blood vessels into the lungs. People with lactose intolerance can purchase lactose-free dairy products available in grocery stores or take dietary supplements that provide lactase to help digest lactose.
Malnutrition[32]
Malnutrition is a condition that develops when the body is deprived of vitamins, minerals, and other nutrients it needs to maintain healthy tissues and organ function. It occurs in people who are either undernourished or overnourished. In the United States, more children suffer from malnutrition due to dietary imbalances than due to nutritional deficiencies. About one percent of children in the United States suffer from chronic malnutrition.
Undernutrition occurs when not enough essential nutrients are consumed or when they are excreted more rapidly than they can be replaced. Overnutrition occurs in people who eat too much, eat the wrong things, don't exercise enough, or take too many vitamins or other dietary replacements. Risk of overnutrition is increased by being more than 20 percent overweight or consuming a diet high in fat and salt.
Malnourished children may be short for their age, thin or bloated, listless, and have weakened immune systems. Nutritional disorders can affect any system in the body and the senses of sight, taste, and smell. They may also produce anxiety, changes in mood, and other psychiatric symptoms. Other symptoms include pale, thick and dry skin, bruising easily, rashes, changes in skin pigmentation, thin hair that is tightly curled and pulls out easily, achy joints, bones that are soft and tender, gums that bleed easily, a tongue that may be swollen or shriveled and cracked, night blindness, and increased sensitivity to light and glare.
Patients who cannot or will not eat or who are unable to absorb nutrients taken by mouth may be fed intravenously (parenteral nutrition) or through a tube inserted into the gastrointestinal tract (enteral nutrition). Tube feeding is often used to provide nutrients to patients who have suffered burns or who have inflammatory bowel disease.
Peptic Ulcers[33]
A peptic ulcer is an open sore or raw area in the lining of the stomach or intestine. There are two types of peptic ulcers: gastric ulcers (that occur in the stomach) and duodenal ulcers (that occur in the initial portion of the small intestine). The inside wall of the stomach (and duodenum) is protected from acid and enzymes by a mucous lining. Ulcers are caused when there is an imbalance between the digestive juices produced by the stomach and the various factors that protect the lining of the stomach (and/or duodenum). On rare occasions, an ulcer may completely erode the stomach or duodenal wall.
Risk factors for peptic ulcers include regular use of aspirin, ibuprofen, naproxen, or other nonsteroidal anti-inflammatory drugs (NSAIDs); excessive alcohol intake; smoking cigarettes or chewing tobacco; or stress from severe illness or surgery. A rare condition called Zollinger-Ellison syndrome causes the stomach to produce too much acid, leading to stomach and duodenal ulcers.
Small ulcers may not cause symptoms and may heal without treatment, whereas larger ulcers can cause serious bleeding. See Figure 14.31[34] for an image of a bleeding gastric ulcer. A common symptom of ulcers is abdominal pain (often in the upper mid-abdomen). Other symptoms include a feeling of fullness; problems drinking as much fluid as usual; nausea and vomiting (possibly bloody); bloody or dark, tarry stools; chest pain; fatigue; and weight loss. Symptoms may vary based on the severity of the ulcer and whether it is located in the stomach versus the duodenum.
A major cause of peptic ulcers is infection with the bacteria called Helicobacter pylori. Treatment for ulcers caused by this bacterium usually includes antibiotics to eradicate the infection, as well as medications to suppress stomach acid. Peptic ulcers tend to recur if left untreated.
Peritonitis[35]
Inflammation of the peritoneum is called peritonitis. Chemical peritonitis can develop any time the wall of the gastrointestinal tract is breached, allowing the contents of the lumen to enter into the peritoneal cavity. For example, when an ulcer perforates the stomach wall, gastric juices spill into the peritoneal cavity. Hemorrhagic peritonitis occurs if the peritoneal cavity fills with blood, such as after a traumatic injury to the liver or spleen or a ruptured tubal pregnancy. Severe peritonitis is associated with bacterial infections seen with appendicitis, colonic diverticulitis, and pelvic inflammatory disease.
Peritonitis is life-threatening and often results in emergency surgery to correct the underlying problem, along with intensive antibiotic therapy. Aggressive surgery and antibiotics have greatly improved the mortality rate from this condition, but even so, the mortality rate still ranges from 30 to 40 percent.
Ulcerative Colitis[36]
Ulcerative colitis is a type of inflammatory bowel disease (IBD) that causes inflammation and sores, called ulcers, in part of the digestive tract. Ulcerative colitis affects the innermost lining of the large intestine, called the colon, and rectum. Symptoms usually develop over time, rather than coming on suddenly.
Ulcerative colitis symptoms can vary, depending on how serious the inflammation is and where it happens. Symptoms may include diarrhea, often with blood or pus; rectal bleeding — passing a small amount of blood with stool; abdominal pain and cramping; rectal pain; urgency to pass stool; not being able to pass stool despite urgency; weight loss; fatigue; fever; and in children, failure to grow. About half of the people with ulcerative colitis have mild to moderate symptoms. The course of ulcerative colitis may vary, with some people having long periods of remission.
The exact cause of ulcerative colitis isn't known. Previously, diet and stress were suspected, but now health care professionals know that these factors may worsen but don't cause ulcerative colitis. Possible causes may include immune system malfunction or genetics. When the immune system tries to fight off an invading virus or bacterium, an irregular immune response causes the immune system to attack the cells in the digestive tract too. Several genetic markers have been associated with ulcerative colitis. Heredity also seems to play a role in that the condition is more common in people who have family members with the disease.
Ulcerative colitis can weaken the body and can sometimes lead to life-threatening complications. While it has no known cure, treatment can greatly reduce and relieve symptoms of the disease and may bring about long-term remission. Ulcerative colitis treatment usually involves either drug therapy or surgery.
- Phillips, M. M. (2023). Appendicitis. MedlinePlus [Internet]. https://medlineplus.gov/ency/article/000256.htm ↵
- “Depiction_of_a_person_suffering_from_Appendicitis” by https://www.myupchar.com/en is licensed under CC BY 4.0 ↵
- Cleveland Clinic. (2022). Celiac disease. https://my.clevelandclinic.org/health/diseases/14240-celiac-disease[/footenote][footnote]Daley, S. F., & Haseeb, M. (2025). Celiac disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441900/ ↵
- Mayo Clinic. (2025). Cirrhosis. https://www.mayoclinic.org/diseases-conditions/cirrhosis/symptoms-causes/syc-20351487 ↵
- American Cancer Society. (2024). American Cancer Society guideline for colorectal cancer screening. https://www.cancer.org/cancer/types/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html ↵
- Sharma, B., & John, S. (2022). Hepatic cirrhosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482419/ ↵
- “Depiction_of_a_Cirrhosis_patient” by https://www.myupchar.com/en is licensed under CC BY 4.0 ↵
- Mayo Clinic. (2025). Gallstones. https://www.mayoclinic.org/diseases-conditions/gallstones/symptoms-causes/syc-20354214 ↵
- “Gallstone_in_neck_of_Gallbladder_on_CT.jpg” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- American Cancer Society. (2024). American Cancer Society guideline for colorectal cancer screening. https://www.cancer.org/cancer/types/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html ↵
- “Colorectal_cancer_endo_2” by unknown author is licensed under CC BY 3.0 ↵
- Mayo Clinic. (2024). Crohn’s disease. https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304 ↵
- Ranasinghe, I. R., Tian, C., & Hsu, R. (2024). Crohn disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK436021/ ↵
- Mayo Clinic. (n.d.). Diarrhea. https://www.mayoclinic.org/diseases-conditions/diarrhea/symptoms-causes/syc-20352241?p=1 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2021). Definition & facts for diverticular disease. https://www.niddk.nih.gov/health-information/digestive-diseases/diverticulosis-diverticulitis/definition-facts ↵
- MedlinePlus [Internet]. (n.d.). Gastroenteritis. https://medlineplus.gov/gastroenteritis.html ↵
- Mayo Clinic. (2024). Gastroesophageal reflux disease. https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940 ↵
- “GERD” by BruceBlaus is licensed under CC BY 4.0 ↵
- Mayo Clinic. (2024). Hemorrhoids. https://www.mayoclinic.org/diseases-conditions/hemorrhoids/symptoms-causes/syc-20360268 ↵
- “Hemorrhoids” by BruceBlaus is licensed under CC BY 4.0 ↵
- Centers for Disease Control and Prevention. (2025). Viral hepatitis basics. https://www.cdc.gov/hepatitis/about/index.html ↵
- Mehta, P., Grant, L. M., & Reddivari, A. K. R. (2024). Viral hepatitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK554549/ ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2017). Irritable bowel syndrome (IBS). National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome ↵
- Qin, H. Y., Cheng, C. W., Tang, X. D., & Bian, Z. X. (2014). Impact of psychological stress on irritable bowel syndrome. World Journal of Gastroenterology, 20(39), 14126–14131. https://doi.org/10.3748/wjg.v20.i39.14126 ↵
- Glazier, E., & Ko, E. (2023). Study links stress to onset of IBS. UCLA Health. https://www.uclahealth.org/news/article/study-links-stress-onset-ibs#:~:text=Study%20links%20stress%20to%20onset,Patient%20Resources ↵
- John Hopkins Medicine. (n.d.). Jaundice. https://www.hopkinsmedicine.org/health/conditions-and-diseases/jaundice-in-children ↵
- “Scleral_Icterus” by Sheila J. Toro is licensed under CC BY 4.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- John Hopkins Health. (n.d.). Malnutrition. https://www.hopkinsmedicine.org/health/conditions-and-diseases/malnutrition ↵
- Phillips, M. M. (2023). Peptic ulcer disease. Penn Medicine. https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/peptic-ulcer-disease ↵
- “Bleeding_gastric_ulcer” by Jeremias is licensed under CC BY 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Mayo Clinic. (2024). Ulcerative colitis. https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/diagnosis-treatment/drc-20353331 ↵
A condition in which the appendix becomes inflamed and is a common reason for emergency surgery.
An inherited autoimmune disorder that causes the immune system to produce antibodies against the gluten protein.
Advanced scarring of the liver commonly caused by hepatitis or alcoholism.
Medical condition of having gallstones.
A type of inflammatory bowel disease (IBD) that causes swelling and irritation of the tissues in the digestive tract.
A condition in which waste moves too quickly through the intestines, preventing adequate water absorption and resulting in loose, watery stools.
A condition that occurs when small pouches, or sacs, form and push outward through weak spots in the wall of the colon.
A condition in which diverticula become inflamed, often suddenly, and may lead to serious complications.
An inflammation of the lining of the stomach and intestines.
A chronic condition where stomach acid flows backward into the esophagus, causing irritation and heartburn.
Also called piles, are swollen veins in the anus and lower rectum.
Inflammation of the liver.
A group of gastrointestinal symptoms that include changes in bowel movements, such as chronic diarrhea, constipation, or both.
Yellowing of the skin and eyes due to excess bilirubin.
A condition characterized by an inability to digest lactose, the sugar found in dairy products.
Occurs when not enough essential nutrients are consumed or when they are excreted more rapidly than they can be replaced.
Occurs in people who eat too much, eat the wrong things, don't exercise enough or take too many vitamins or other dietary replacements.
An open sore or raw area in the lining of the stomach or intestine.
Inflammation of the peritoneum.
A type of inflammatory bowel disease (IBD) that causes inflammation and sores, called ulcers, in part of the digestive tract.

