14.3 Anatomy of the Gastrointestinal System
Anatomy of the Gastrointestinal System[1]
Layers of the Gastrointestinal (GI) Tract
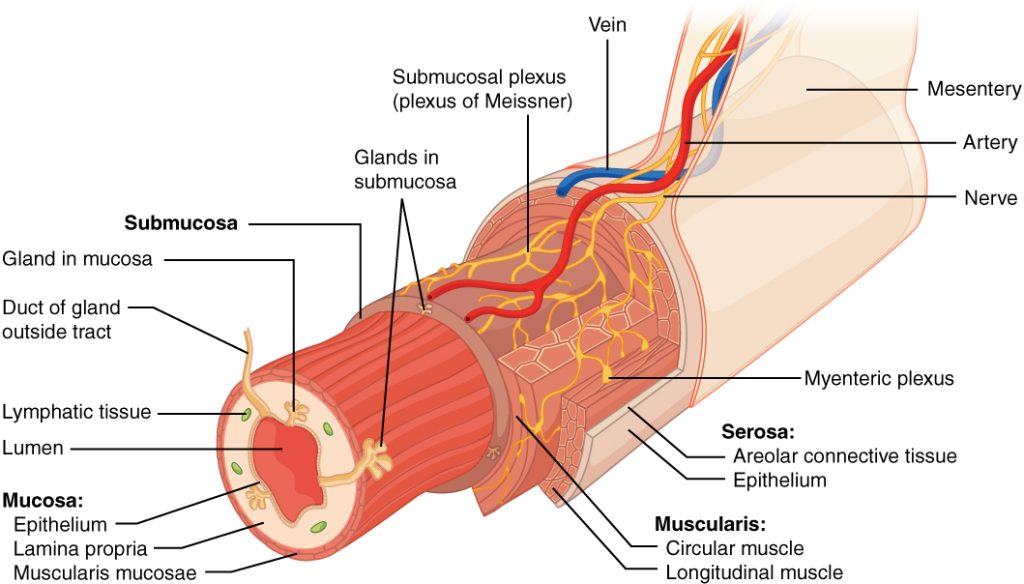
The entire length of the gastrointestinal tract is composed of the same four tissue layers. Starting from the deep inside the lumen (the hollow, tubular portion of the GI tract) and moving out to the superficial layer, these layers are the mucosa, submucosa, muscularis, and serosa, which is continuous with the mesentery. The mesentery is the membrane that connects the intestines to the abdominal wall. See Figure 14.4[2] for an illustration of the layers of the GI tract.
Mucosa
The mucosa is referred to as a mucous membrane because mucus production is a characteristic feature. The membrane consists of epithelial cells, which are in direct contact with ingested food. Located among these epithelial cells are goblet cells, which secrete mucus and fluid into the lumen. In the mouth, pharynx, esophagus, and anal canal, the epithelium is primarily a non-keratinized, stratified squamous epithelium. In the stomach and intestines, it is a simple columnar epithelium.
Epithelial cells have a very brief life span, averaging only a couple of days in the mouth to about a week in the gut. This process of rapid renewal helps preserve the health of the GI tract, despite the wear and tear resulting from continued contact with food.
In addition, the mucosa has a thin, smooth muscle layer, called the muscularis mucosae (not to be confused with the muscularis layer, as described below), and the lamina propria, a layer of connective tissue similar to the dermis.
The muscularis mucosae is in a constant state of tension, pulling the mucosa of the stomach and small intestine into rippling folds. These folds dramatically increase the surface area available for digestion and absorption.
The lamina propria contains numerous blood and lymphatic vessels that transport nutrients absorbed through the GI tract to other parts of the body. The lamina propria also houses clusters of lymphocytes, making up the mucosa-associated lymphoid tissue (MALT). These lymphocyte clusters are substantial in the distal small intestine where they are known as Peyer’s patches. When considering the gastrointestinal tract is exposed to foodborne bacteria and other pathogens, it is easy to understand why the immune system has evolved a means of defending it.
Submucosa
The submucosa is superficial to the mucosa. It is composed of a broad layer of dense connective tissue that connects the overlying mucosa to the underlying muscularis. It includes blood and lymphatic vessels that transport absorbed nutrients and a scattering of submucosal glands that release digestive secretions.
Muscularis
The third layer of the GI tract is the muscularis (also called the muscularis externa). In the mouth, pharynx, anterior part of the esophagus, and external anal sphincter, the muscularis is made up of skeletal muscle, giving voluntary control over swallowing and defecation. The stomach is equipped for its churning function by the addition of a third layer, the oblique muscle. The muscularis in the small intestine is made up of a double layer of smooth muscle: an inner circular layer and an outer longitudinal layer. The contractions of these layers promote mechanical digestion, expose more of the food to digestive chemicals, and move the food along the canal. While the colon has two layers like the small intestine, its longitudinal layer is segregated into three narrow parallel bands, the tenia coli, which make it look like a series of pouches rather than a simple tube.
Serosa
The serosa is the portion of the alimentary canal superficial to the muscularis. Present only in the region of the GI tract within the abdominal cavity, it consists of a layer of visceral peritoneum overlying a layer of loose connective tissue.
Instead of serosa, the mouth, pharynx, and esophagus have a dense sheath of collagen fibers called the adventitia to hold them in place.
The Peritoneum
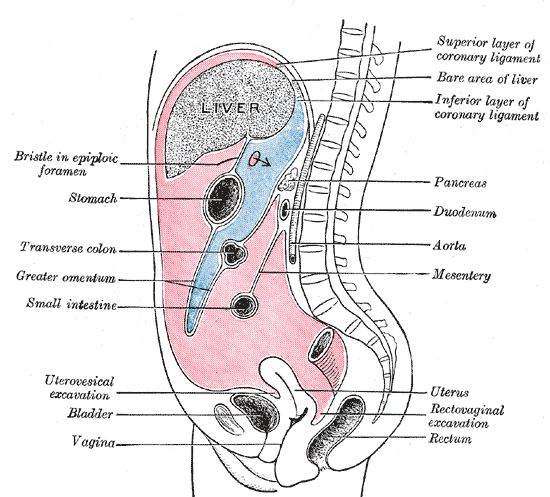
The digestive organs in the abdominal cavity are held in place by the peritoneum, a broad serous membrane made up of squamous epithelial tissue surrounded by connective tissue. It is composed of two different regions: the parietal peritoneum, which lines the abdominal wall, and the visceral peritoneum, which covers the abdominal organs.
The visceral peritoneum includes multiple large folds that envelope various abdominal organs, holding them to the dorsal surface of the body wall. Within these folds are blood vessels, lymphatic vessels, and nerves that innervate the organs with which they are in contact, supplying their adjacent organs. The five major peritoneal folds are described in Table 14.3. Note that during fetal development, certain digestive structures, including the first portion of the small intestine (called the duodenum), the pancreas, and portions of the large intestine (the ascending and descending colon, and the rectum) remain completely or partially posterior to the peritoneum. Thus, the location of these organs is described as retroperitoneal. See Table 14.3 for an overview of the five major peritoneal folds.
Table 14.3. Major Peritoneal Folds[3]
| Fold | Description |
|---|---|
| Greater Omentum | Apron-like structure that lies superficial to the small intestine and transverse colon; a site of fat deposition in people who are overweight |
| Falciform Ligament | Anchors the liver to the anterior abdominal wall and inferior border of the diaphragm |
| Lesser Omentum | Suspends the stomach from the inferior border of the liver; provides a pathway for structures connecting to the liver |
| Mesentery | Vertical band of tissue anterior to the lumbar vertebrae and anchoring all of the small intestine except the initial portion (the duodenum) |
| Mesocolon | Attaches two portions of the large intestine (the transverse and sigmoid colon) to the posterior abdominal wall |
The peritoneal cavity is the space between the visceral and parietal peritoneal layers. A few milliliters of watery fluid called peritoneal fluid act as a lubricant to minimize friction between the layers of the peritoneum.
See Figure 14.5[4] for an illustration of the peritoneal cavity colored in pink.
Digestive System Organs
The easiest way to understand the digestive system is to divide its organs into two main categories. The first group is the organs that make up the GI tract or alimentary canal. The second group includes accessory digestive organs that are important for the breakdown of food and the absorption and digestion of nutrients into the body. Food does not travel through accessory organs.
Gastrointestinal Tract Organs
The Mouth
The cheeks, tongue, and palate frame the mouth, which is also called the oral cavity (or buccal cavity). The structures of the mouth are illustrated in Figure 14.6.[5] See the subsection on “Accessory Organs of the Digestive System” for information on the teeth, tongue, and salivary glands.
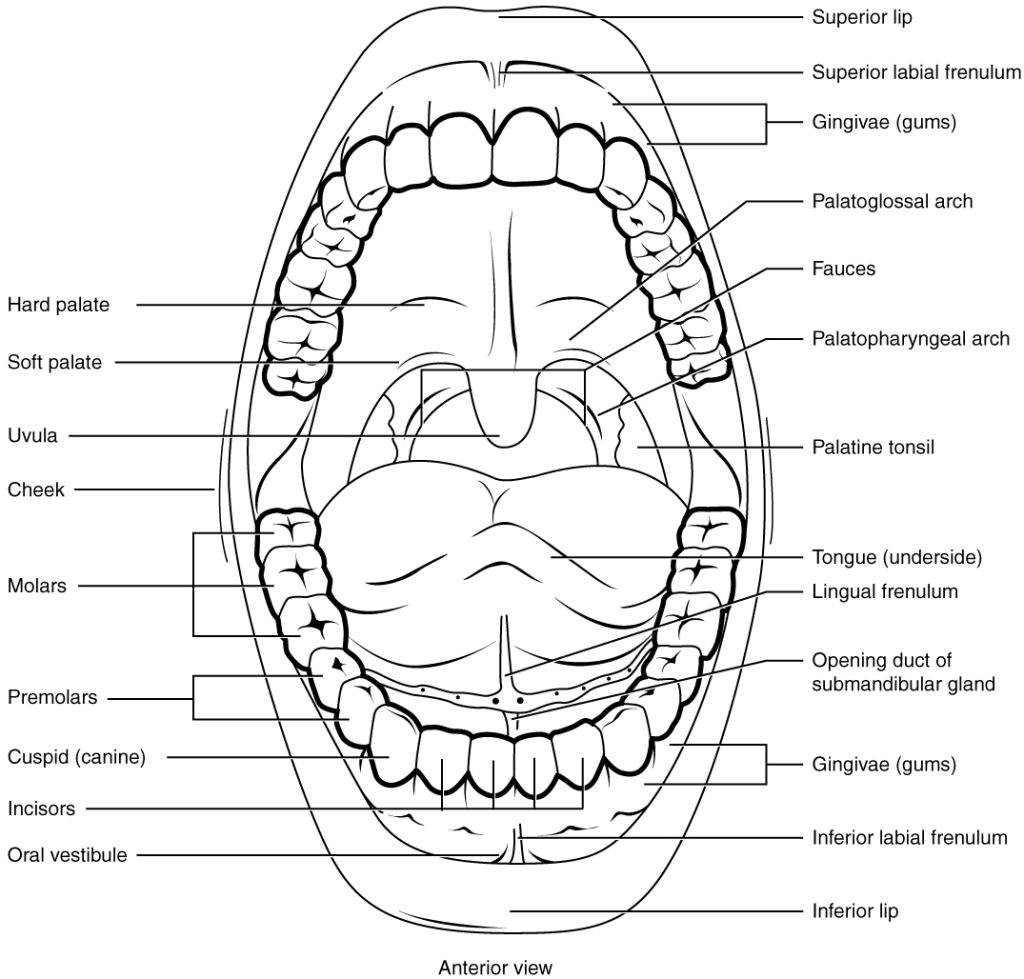
At the entrance to the mouth are the lips, also called the labia (singular = labium). Their outer covering is skin, which transitions to a mucous membrane inside the mouth. Lips are very vascular with a thin layer of keratin, which is the reason they are “red.” The lips cover the orbicularis oris muscle, which functions to control the opening and closing of the mouth, playing a key role in regulating what enters or exits the oral cavity.
The cheeks make up the lateral walls of the oral cavity. While their outer covering is skin, their inner covering is a mucous membrane. This membrane is made up of non-keratinized, stratified squamous epithelium. Between the skin and mucous membranes are connective tissue and buccinator muscles.
Chewing and breathing can occur simultaneously due to the arched shape of the palate, which allows the mouth to support both digestion and respiration. This arch is called the palate and is divided into an anterior portion made of bone (hard palate) and a posterior portion made of muscle (soft palate).
The anterior region, or hard palate, serves as a wall (septum) between the oral and nasal cavities, as well as a rigid surface against which the tongue can push food. It is formed by the maxillary and palatine bones of the skull.
If you run your tongue along the roof of your mouth, you’ll notice that the hard palate ends in the posterior oral cavity, and the tissue becomes fleshier. This part of the palate, known as the soft palate, is composed mainly of skeletal muscle. During swallowing, the soft palate pushes superiorly so food cannot go into the nasal cavity.
A fleshy mass of tissue called the uvula hangs down from the center of the posterior edge of the soft palate. When you swallow, the uvula moves upward, helping to keep foods and liquid from entering the nasal cavity. Unfortunately, it can also contribute to the sound produced by snoring.
The Pharynx
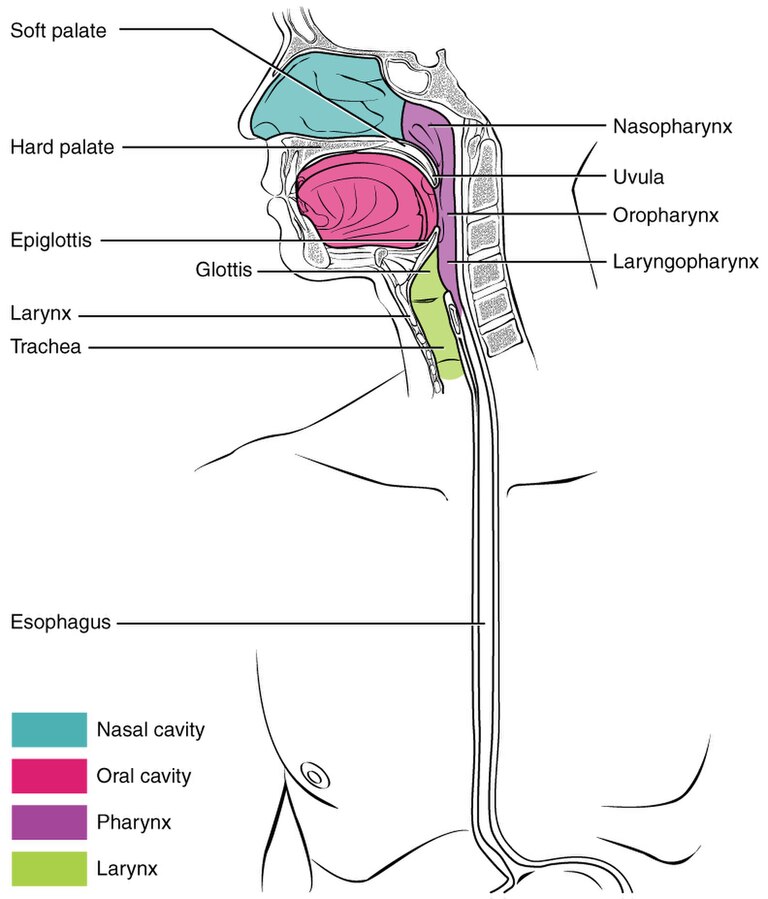
The pharynx (throat) is involved in both digestion and respiration. It receives food and air from the mouth and air from the nasal cavity.
The pharynx is a short tube of skeletal muscle lined with a mucous membrane. It runs from the posterior nasal and oral cavities to the opening of the esophagus and larynx. It has three subdivisions: the nasopharynx, oropharynx and laryngopharynx.
The most superior portion of the pharynx, the nasopharynx, is involved only in breathing and speech. It is located posterior to the nasal cavity. During swallowing, the entrance to the nasopharynx is closed off by the soft palate and uvula to prevent food and liquids from moving upward and into the nasal cavity.
The oropharynx is used for both breathing and digestion and is located posterior to the oral cavity. It is inferior to the nasopharynx and superior to the laryngopharynx.
The laryngopharynx is also used for both breathing and digestion. The anterior portion connects to the larynx, allowing air to flow into the bronchial tree. The inferior border of the laryngopharynx is continuous with the esophagus.
During swallowing, the larynx is pulled up and the epiglottis, a cartilaginous structure, covers the glottis (the opening to the larynx) to prevent food and liquids from going into the trachea and bronchi, which are located inferior to the larynx. If food somehow does enter the trachea, the reaction is to cough, which usually forces the food up and out of the trachea, and back into the pharynx. See Figure 14.7[6] for an illustration of the subdivisions of the pharynx and the epiglottis.
The Esophagus
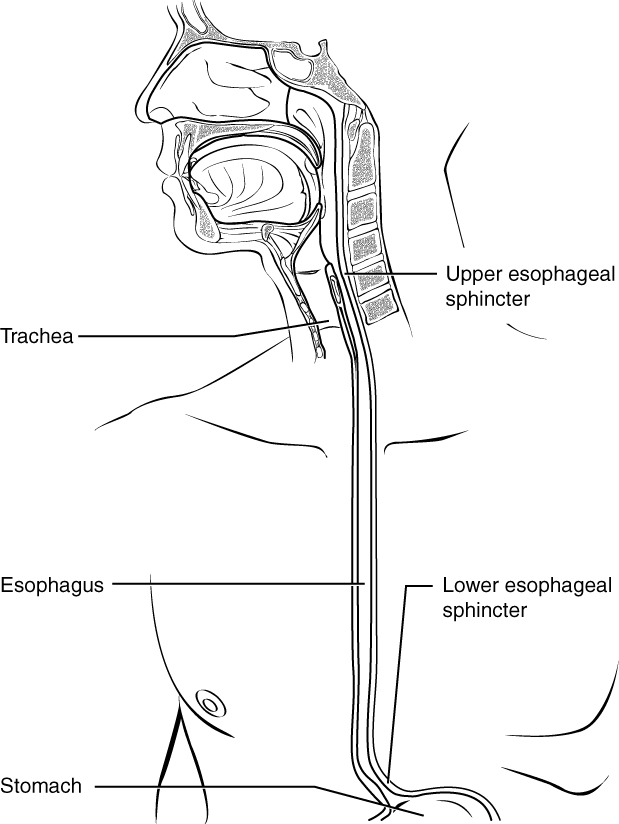
The esophagus is a muscular tube that connects the pharynx to the stomach. It is approximately ten inches in length, located posterior to the trachea, and remains in a collapsed form when not swallowing.
The upper esophageal sphincter (UES) controls the movement of food from the pharynx into the esophagus. Sphincters are circular muscles that surround openings to tubes and regulate the movement of materials, closing the tube when the sphincters contract and opening it when they relax.
The upper two thirds of the esophagus consists of both smooth and skeletal muscle, with the amount of skeletal muscle decreasing in the bottom third of the esophagus. Rhythmic waves of peristalsis, which begin in the upper esophagus, move the bolus toward the stomach. At the same time, secretions from the esophageal mucosa lubricate the esophagus and food. To enter the abdomen, the esophagus goes through an opening in the diaphragm called the esophageal hiatus.
Food passes from the esophagus into the stomach at the lower esophageal sphincter (LES) (also called the gastroesophageal or cardiac sphincter). The lower esophageal sphincter relaxes to let food pass into the stomach and then contracts to prevent stomach acid from backing up into the esophagus.
Surrounding the lower esophageal sphincter is the muscular diaphragm, which helps close the sphincter when no food is being swallowed. When the lower esophageal sphincter does not completely close, stomach contents can reflux (back up into the esophagus), causing heartburn or gastroesophageal reflux disease (GERD). Read more about GERD in the “Digestive Systems Disorders” section.
See Figure 14.8[7] for an illustration of the esophagus.
Stomach
The stomach is an expansion of the gastrointestinal tract located inferior to the esophagus. The stomach links the esophagus to the first part of the small intestine (the duodenum) and is relatively fixed in place.
The stomach can be a highly active structure, contracting and continually changing position and size. These muscular contractions provide mechanical assistance to digestion. The stomach, normally about the size of a fist when empty, can expand to hold up to 4 liters of food and fluid – over 75 times its resting volume – then shrink back after emptying. Although one might think that the size of a person’s stomach is related to how much food that individual consumes, body weight does not correlate with stomach size. Rather, when greater quantities of food are eaten—such as at holiday dinner—the stomach stretches more than when less is eaten.
An important function of the stomach is to serve as a temporary holding chamber. Eating a meal happens much more quickly than it can be digested and absorbed by the small intestine. The stomach holds food and passes only small amounts into the small intestine at a time. Food is mixed together with digestive juices in the stomach until they are converted into a soupy liquid called chyme, which is released into the small intestine.
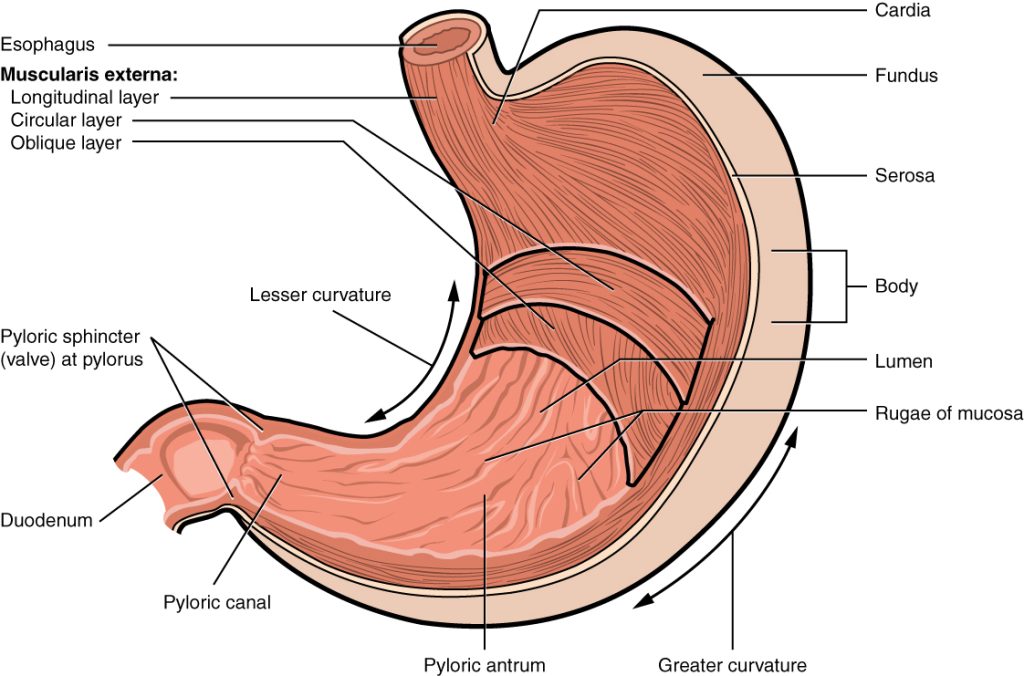
There are four main regions in the stomach: the cardia, fundus, body, and pylorus.
The cardia (or cardiac region) is the point where the esophagus connects to and through which food passes into the stomach. Located inferior to the diaphragm, above and to the left of the cardia, is the dome-shaped fundus. Below the fundus is the body, the main part of the stomach. The funnel-shaped pylorus connects the stomach to the duodenum.
The smooth muscle pyloric sphincter is located between the pylorus and the duodenum (the first part of the small intestine) and controls stomach emptying.
In the absence of food, the stomach deflates inward, and its mucosa and submucosa form large folds called rugae (singular = ruga).
See Figure 14.9[8] for an illustration of the regions of the stomach.
The stomach plays several important roles in chemical digestion, including the continued digestion of carbohydrates and the initial digestion of proteins and triglycerides. Salivary amylase, an enzyme in saliva, begins the chemical digestion of starches in the mouth. Little, if any, absorption occurs in the stomach, with the exception of alcohol and some medications such as aspirin.
Within a few minutes after food enters your stomach, mixing waves begin to occur at intervals of approximately 20 seconds. A mixing wave is a unique type of peristalsis that mixes and softens the food with gastric juices to create a soupy mixture called chyme.
The pylorus acts as a filter, permitting only liquids and small food particles to pass through the mostly, but not fully, closed pyloric sphincter. In a process called gastric emptying, rhythmic mixing waves force only about 3 mL of chyme at a time through the pyloric sphincter and into the duodenum. Release of a greater amount of chyme at one time would overwhelm the capacity of the small intestine to handle it. The rest of the chyme is pushed back into the body of the stomach, where it continues mixing. This process is repeated when the next mixing waves force more chyme into the duodenum.
The fundus of the stomach plays an important role because it stores both undigested food and gases that are released during the process of chemical digestion. Food may sit in the fundus of the stomach for a while before being mixed with the chyme. While the food is in the fundus, the digestive activities of salivary amylase continue until the food begins mixing with the acidic chyme. Ultimately, mixing waves incorporate this food with the chyme, the acidity of which inactivates salivary amylase and activates lingual lipase, an enzyme released from the glands of the tongue. Lingual lipase then begins breaking down triglycerides. The breakdown of protein begins in the stomach through the actions of HCl and the enzyme pepsin.
In addition to its numerous digestive functions, the stomach also produces intrinsic factor that is essential for the intestinal absorption of vitamin B12. This vitamin is necessary for both the production of mature red blood cells and normal neurological functioning. People who have their stomach removed (gastrectomy), such as for advanced stomach cancer, can survive with minimal digestive issues if they receive vitamin B12 injections.
Most contents of the stomach are completely emptied into the duodenum within two to four hours after eating a meal. Different types of food take different amounts of time to process. Foods high in carbohydrates empty fastest, followed by high-protein foods. Meals with a high-fat content remain in the stomach the longest. Because enzymes in the small intestine digest fats slowly, food can stay in the stomach for six hours or longer when the duodenum is processing fatty chyme. However, note that this is still a fraction of the 24 to 72 hours that full digestion typically takes from start to finish.
The Small Intestine
Chyme released from the stomach enters the small intestine, which is the primary digestive organ in the body. Additionally, the small intestine is the site of most nutrient absorption.
The longest part of the gastrointestinal tract, the small intestine, is about 3.05 meters (10 feet) long in a living person. Despite being significantly longer than the large intestine, the small intestine is named for its narrower diameter – approximately 1 inch compared with the 3-inch diameter of the large intestine.
In addition to length, the folds and projections of the small intestine’s lining work to give it an enormous surface area, which is approximately 200 square meters (m2), more than 100 times the surface area of your skin. This large surface area is necessary for the complex processes of digestion and absorption that occur within it. See Figure 14.10[9] for an illustration of the small intestine.
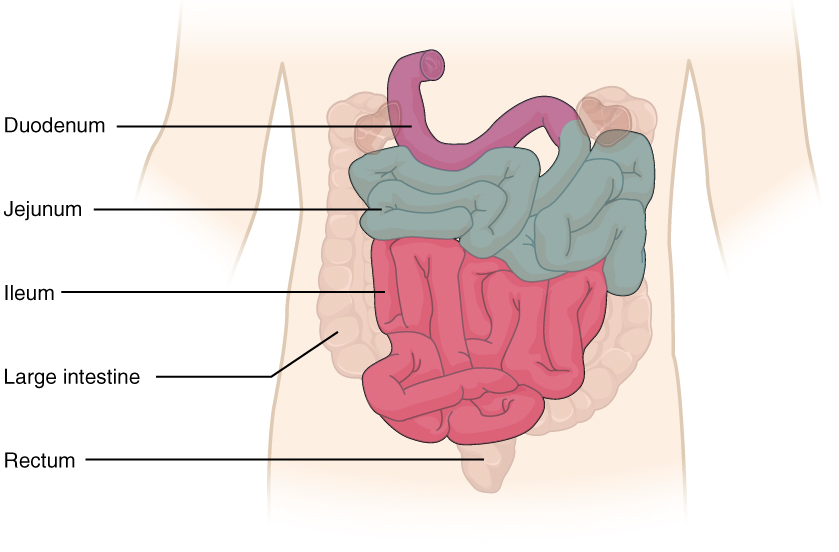
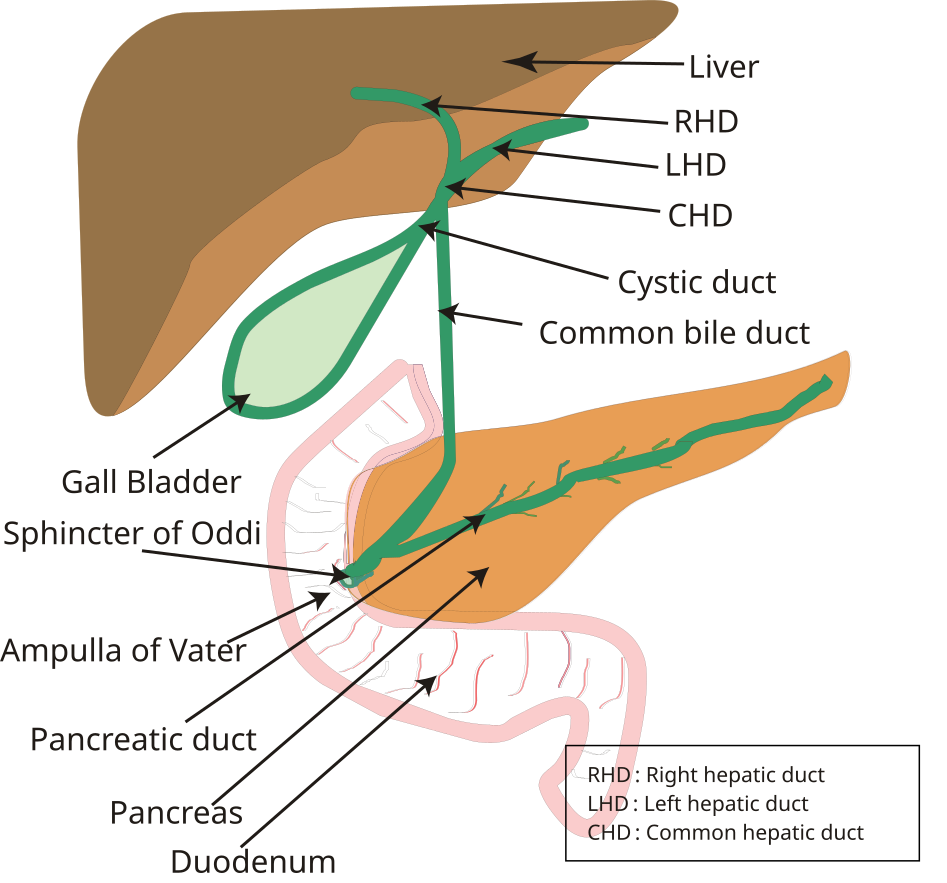
The small intestine is subdivided into three regions: the duodenum, jejunum, and ileum (proximal to distal starting at the stomach). The duodenum is the shortest part of the small intestine. It is 25.4 cm (10 inches) long and begins at the pyloric sphincter. Located in the duodenal wall is the hepatopancreatic ampulla (ampulla of Vater). The ampulla is where the bile duct (through which bile passes from the liver) and the main pancreatic duct (through which pancreatic juice passes from the pancreas) join. This ampulla opens into the duodenum. The hepatopancreatic sphincter (sphincter of Oddi) regulates the flow of both bile and pancreatic juice from the ampulla into the duodenum. See Figure 14.11[10] for an illustration of the ducts.
The jejunum is about 3 feet long and runs from the duodenum to the ileum. Jejunum means “empty” in Latin and supposedly was so named by the ancient Greeks who noticed it was always empty at death. No clear line exists between the jejunum and the final segment of the small intestine, the ileum.
The ileum is the longest part of the small intestine, measuring about 6 feet in length. It is thicker, more vascular, and has more developed mucosal folds than the jejunum. The ileum joins the cecum, the first portion of the large intestine, at the ileocecal sphincter (or valve).
Recall the four layers present in the walls of the gastrointestinal tract. The small intestine has structural modifications in these layers that increase the surface area for absorption more than 600-fold. These special features include circular folds, villi, and microvilli. These adaptations are most abundant in the proximal two thirds of the small intestine, where the majority of absorption occurs.
Circular folds (also called plicae circulares) are deep ridges in the mucosa and submucosa that facilitate absorption. Their shape causes the chyme to spiral rather than move in a straight line through the small intestine. Spiraling slows the movement of chyme and provides the time needed for nutrients to be fully absorbed.
Within the circular folds are small (0.5–1 mm long) hairlike projections called villi (singular = villus) that give the mucosa a fuzzy appearance. There are about 20 to 40 villi per square millimeter, greatly increasing the surface area of the epithelium. The mucosal epithelium, primarily composed of absorptive cells, covers the villi. In addition to muscle and connective tissue to support its structure, each villus contains a capillary bed composed of one arteriole and one venule, as well as a lymphatic capillary called a lacteal. The breakdown products of carbohydrates and proteins (monosaccharides and amino acids) can enter the bloodstream directly, but lipid breakdown products are absorbed by the lacteals and transported to the bloodstream via the lymphatic system.
As their name suggests, microvilli (singular = microvillus) are much smaller (1 µm) than villi. They are surface extensions of the plasma membrane of the mucosa’s epithelial cells. Although their small size makes it difficult to see each microvillus, their combined microscopic appearance suggests a mass of bristles, which is termed the brush border. Fixed to the surface of the microvilli membranes are enzymes that finish digesting carbohydrates and proteins. There are an estimated 200 million microvilli per square millimeter of small intestine, greatly expanding the surface area of the plasma membrane and, therefore, enhancing absorption.
See Figure 14.12[11] for an illustration of the small intestine with the circular folds, villi, and microvilli.

In addition to the three specialized absorptive features, the mucosa between the villi has deep crevices that lead to intestinal glands. These intestinal glands produce intestinal juice, a slightly alkaline (pH 7.4 to 7.8) mixture of water and mucus. Each day, about 0.95 to 1.9 liters (1 to 2 quarts) are secreted in response to the distention of the small intestine or the irritating effects of chyme on the intestinal mucosa.
Intestinal juice combines with pancreatic juice to facilitate absorption. The small intestine is also where most water is absorbed via osmosis.
The digestion of proteins and carbohydrates begins in the mouth with salivary amylase and is completed in the small intestine. Intestinal and pancreatic juice continue to digest proteins into peptides and then amino acids and carbohydrates into disaccharides and then monosaccharides.
Lipids arrive in the small intestine largely undigested. Bile and the enzyme pancreatic lipase are added to the small intestine, which is primarily responsible for digesting lipids.
The Large Intestine
The large intestine is the last part of the gastrointestinal tract. The primary function of this organ is to finish absorption of water, synthesize certain vitamins, form feces, and eliminate feces from the body.
The large intestine runs from the appendix to the anus and frames the small intestine on three sides. The large intestine is subdivided into four main regions: the cecum, the colon, the rectum, and the anus. The ileocecal valve, located at the opening between the ileum and the large intestine, regulates the flow of chyme from the small intestine to the large intestine.
The first part of the large intestine is the cecum, a pouch-like structure that is suspended below the ileocecal valve. It is about 2.4 inches long. The cecum receives the contents of the ileum and continues the absorption of water and salts.
The appendix (or vermiform appendix) is a winding tube that attaches to the cecum and is about 3 inches long. The appendix contains lymphatic tissue, suggesting an immune function, but this organ is generally considered vestigial or no longer functional. However, at least one recent report proposes a survival advantage provided by the appendix: in diarrheal illness, the appendix may serve as a bacterial reservoir to repopulate the intestinal bacteria for those surviving the initial phases of the illness.
Upon entering the colon, the food residue first travels superiorly through the ascending colon on the right side of the abdomen. At the inferior surface of the liver, the colon bends to form the right colic flexure (hepatic flexure) and becomes the transverse colon. Food residue passing through the transverse colon travels across to the left side of the abdomen, where the colon angles sharply immediately inferior to the spleen, at the left colic flexure (splenic flexure). From there, food residue passes through the descending colon, which runs inferiorly on the left side of the posterior abdominal wall. After entering the pelvis inferiorly, it becomes the s-shaped sigmoid colon. See Figure 14.13[12] for an illustration of the parts of the colon.
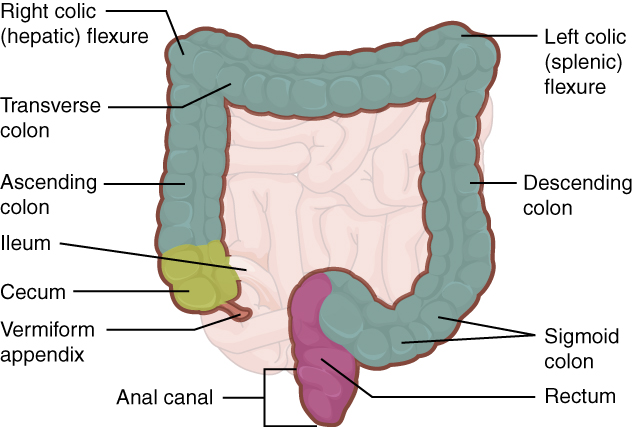
Food residue leaving the sigmoid colon enters the rectum, the final eight inches of the gastrointestinal tract. Even though rectum is Latin for “straight,” this structure follows the curved contour of the sacrum and has three lateral bends that create a trio of internal transverse folds called the rectal valves. These valves help separate the feces from gas to prevent the simultaneous passage of feces and gas.
Finally, food residue reaches the last part of the large intestine, the anal canal. This structure is about 1.5–2 inches long and opens to the exterior of the body at the anus. The anal canal includes two sphincters, the internal anal sphincter and the external anal sphincter. The internal anal sphincter is made of smooth muscle, and its contractions are involuntary. The external anal sphincter is made of skeletal muscle, which is under voluntary control after a child is potty trained. Except when defecating, both usually remain closed.
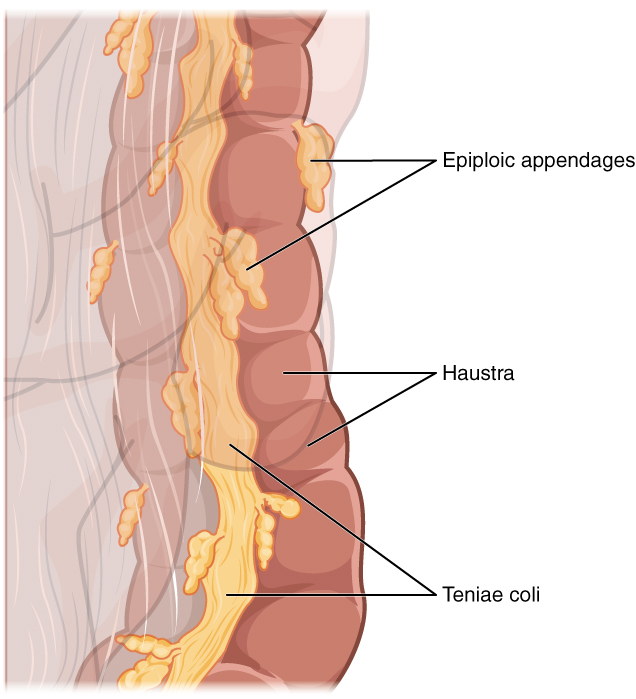
Three features are unique to the large intestine: teniae coli, haustra, and epiploic appendages. The teniae coli are three bands of smooth muscle that make up the longitudinal muscle layer of the muscularis of the large intestine, except at its terminal end. Contractions of the teniae coli bunch up the colon into a succession of pouches called haustra (singular = haustrum), which are responsible for the wrinkled appearance of the colon. Attached to the teniae coli are small, fat-filled sacs of visceral peritoneum called epiploic appendages. The purpose of these is unknown. The rectum and anal canal have neither teniae coli nor haustra, but they do have well-developed layers of muscularis that create the strong contractions needed for defecation.
See Figure 14.14[13] for an illustration of these features of the large intestine.
Most bacteria that enter the GI tract are killed by lysozyme, hydrochloric acid (HCl), or protein-digesting enzymes. However, trillions of bacteria live within the large intestine that are referred to as normal flora. Most of the 700 species of these bacteria are nonpathogenic organisms that cause no harm as long as they stay inside the gut lumen. In fact, many facilitate chemical digestion and absorption, and some make certain vitamins, mainly biotin, pantothenic acid, and vitamin K. Some are linked to the immune response.
The chyme entering the large intestine contains few nutrients aside from water, which is gradually reabsorbed as the residue remains there for 12 to 24 hours. Because of this, the large intestine can be completely removed without significantly affecting digestive functioning. For example, in severe cases of inflammatory bowel disease, the large intestine can be removed by a procedure known as a colectomy. Often, a new fecal pouch can be crafted from the small intestine and sutured to the anus, but if not, an ileostomy can be created by bringing the distal ileum through the abdominal wall, allowing the watery chyme to be collected in an adhesive pouch.
Although the glands of the large intestine secrete mucus, they do not secrete digestive enzymes. Therefore, chemical digestion in the large intestine occurs exclusively from bacteria in the lumen of the colon. Bacteria break down some of the remaining carbohydrates, resulting in the discharge of hydrogen, carbon dioxide, and methane gases that create flatus (gas) in the colon; flatulence is excessive flatus. Each day, up to 1500 mL of gas is produced in the colon. More is produced when you eat foods such as beans, which are rich in otherwise indigestible sugars and complex carbohydrates like soluble dietary fiber.
Feces Formation and Defecation
The small intestine absorbs about 90 percent of the water ingested (either as liquid or within solid food). The large intestine absorbs most of the remaining water, a process that converts the liquid chyme residue into semi-solid feces (“stool”).
Feces is composed of undigested food residues, unabsorbed digested substances, millions of bacteria, old epithelial cells from the GI mucosa, inorganic salts, and enough water to let it pass smoothly out of the body. Of every 500 mL (17 ounces) of food residue that enters the cecum each day, about 150 mL (5 ounces) become feces.
Feces are eliminated through contractions of the rectal muscles. You help this process by a voluntary procedure called Valsalva’s maneuver, in which you increase intraabdominal pressure by contracting your diaphragm and abdominal wall muscles and closing your glottis.
The process of defecation begins when mass movements force feces from the colon into the rectum, stretching the rectal wall and provoking the defecation reflex, which eliminates feces from the rectum. It contracts the sigmoid colon and rectum, relaxes the internal anal sphincter, and initially contracts the external anal sphincter.
The presence of feces in the anal canal sends a signal to the brain, which gives you the choice of voluntarily opening the external anal sphincter (defecating) or keeping it temporarily closed. If you decide to delay defecation, it takes a few seconds for the reflex contractions to stop and the rectal walls to relax. The next mass movement will trigger additional defecation reflexes until you defecate.
If defecation is delayed for an extended time, additional water is absorbed, making the feces firmer and potentially leading to constipation. On the other hand, if the waste matter moves too quickly through the intestines, not enough water is absorbed, and diarrhea can result. Diarrhea can also be caused by the ingestion of foodborne pathogens. In general, diet, health, and stress determine the frequency of bowel movements. The number of bowel movements varies greatly between individuals, ranging from two or three per day to three or four per week.
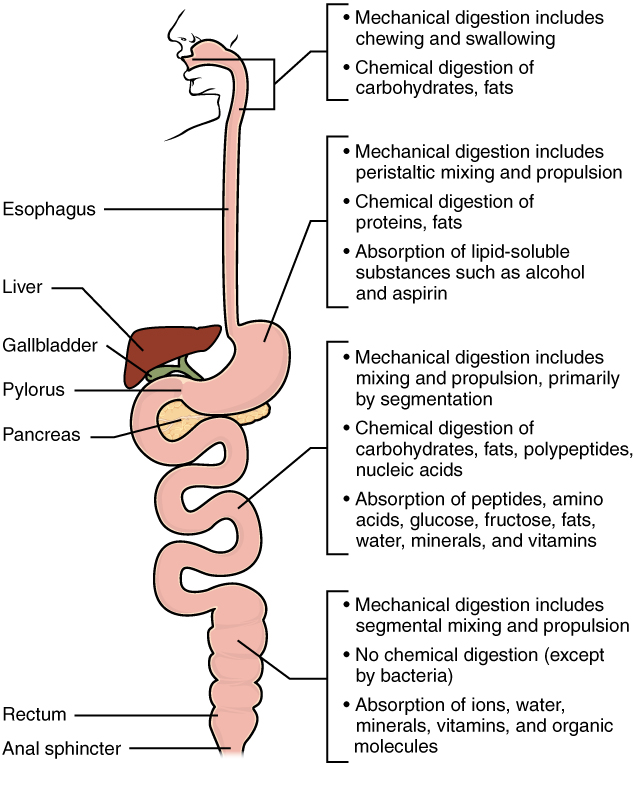
See Figure 14.15[14] for an illustration of digestion and absorption through the digestive tract.
Accessory Organs of the Digestive System
While food travels through the GI tract, each accessory digestive organ also aids in the breakdown of food. Within the mouth, the teeth and tongue begin mechanical digestion, whereas the salivary glands begin chemical digestion. Once food products enter the small intestine, the gallbladder, liver, and pancreas release secretions—such as bile and enzymes—essential for digestion to continue.
Salivary Glands
Many small salivary glands are located in the mucous membranes of the mouth and tongue. These exocrine glands are constantly secreting saliva, either directly into the oral cavity or indirectly through ducts, even while you sleep. An average of 1 to 1.5 liters of saliva is secreted each day. Usually, just enough saliva is present to moisten the mouth and teeth.
Saliva secretion increases when you eat because saliva is necessary to moisten food and start the chemical breakdown of carbohydrates. Small amounts of saliva are also secreted by glands in the lips. In addition, the buccal glands in the cheeks, palatal glands in the palate, and lingual glands in the tongue help make sure that all areas of the mouth are supplied with adequate saliva.
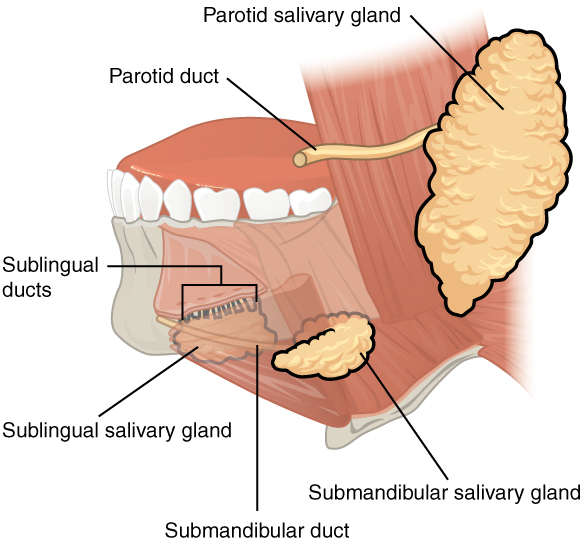
There are three pairs of major salivary glands that secrete the majority of saliva into ducts that open into the mouth: the parotid glands, the sublingual glands, and the submandibular glands:
- The parotid glands lie between the skin and the masseter muscle anterior to the ears. They secrete saliva into the mouth through the parotid duct, which is located near the second upper molar tooth.
- The sublingual glands, which lie inferior to the tongue, use the lesser sublingual ducts to secrete saliva.
- The submandibular glands, which are in the floor of the mouth inferior to the mandible, secrete saliva into the mouth through the submandibular ducts.
See Figure 14.16[15] for an illustration of the major salivary glands.
Saliva is mostly (99.4 percent) water. The remaining 0.6 percent is a mixture of ions, glycoproteins, enzymes, growth factors, and waste products. The most important ingredient in saliva for digestion is the enzyme salivary amylase, which begins the chemical breakdown of carbohydrates. Food does not spend enough time in the mouth to allow all the carbohydrates to break down, but salivary amylase continues working until it is inactivated by stomach acid.
Saliva is slightly acidic with a pH between 6.35 and 6.85. Salivary mucus helps lubricate food, facilitating movement in the mouth, bolus (mass of chewed food) formation, and swallowing.
Tongue
It has been said that the tongue is the strongest muscle in the body. Those who make this claim cite its strength proportionate to its size. Although it is difficult to quantify the relative strength of different muscles, it remains indisputable that the tongue is a workhorse, facilitating ingestion, mechanical digestion, chemical digestion (lingual lipase), sensation (taste, texture, and temperature of food), swallowing, and vocalization.
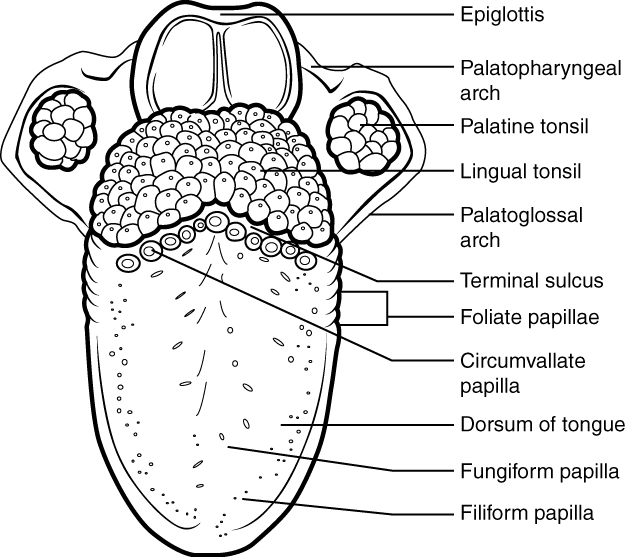
The superior and lateral regions of the tongue are covered with papillae, extensions of the lamina propria of the mucosa, which are covered in stratified squamous epithelium. A special type of papillae is called fungiform papillae, which are mushroom shaped and cover a large area of the tongue. These fungiform papillae contain taste buds. See Figure 14.17[16] for an illustration of papillae. Read more about the sensation of taste in the “Senses” section of the “Nervous System” chapter.
Deglutition is another word for swallowing—the movement of food from the mouth to the stomach. The entire process takes about four to eight seconds for solid or semisolid food and about one second for very soft food and liquids. Although this sounds quick and effortless, deglutition is a complex process that involves both the skeletal muscle of the tongue and the muscles of the pharynx and esophagus. It is aided by the presence of mucus and saliva.
Teeth
The teeth, or dentes (singular = dens), are organs similar to bones that are used to tear, grind, and otherwise mechanically break down food.
The teeth are secured in the alveolar processes (sockets) of the maxilla and the mandible. Gingivae (commonly called the gums) are soft tissues that line the alveolar processes and surround the necks of the teeth.
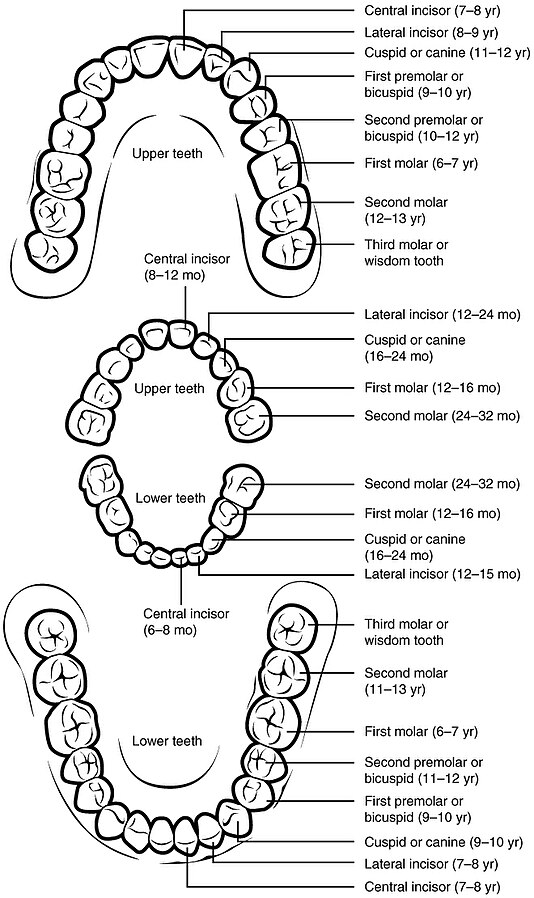
During the course of a lifetime, most individuals have two sets of teeth (one set of teeth is a dentition). Your 20 deciduous teeth, also known as primary or baby teeth, first begin to appear at about six months of age. Between approximately age 6 and 12, these teeth are replaced by 32 permanent teeth. Moving from medial to lateral in the mouth, the teeth are as follows:
- The eight incisors, four top and four bottom, are the sharp front teeth you use for biting into food.
- The four cuspids (or canines) are lateral to the incisors and have a pointed edge (cusp) to tear up food. These fang-like teeth are excellent for piercing tough or fleshy foods.
- Posterior to the cuspids are the eight premolars (or bicuspids), which have an overall flatter shape with two rounded cusps useful for mashing foods.
- The most posterior and largest are the 12 molars, which have several pointed cusps used to crush food, so it is ready for swallowing. The third of each set of three molars, top and bottom, are commonly referred to as the wisdom teeth because their eruption is commonly delayed until early adulthood. It is not uncommon for wisdom teeth to fail to erupt; that is, they remain impacted. In these cases, the teeth are typically removed by oral surgery.
See Figure 14.18[17] for an illustration of the deciduous and permanent teeth.
The two main parts of a tooth are the crown, which is the visible portion above the gum line, and the root, which is embedded within sockets of the maxilla and mandible. Both parts contain an inner pulp cavity, containing loose connective tissue with nerves and blood vessels. The region of the pulp cavity that runs through the root of the tooth is called the root canal.
Surrounding the pulp cavity is dentin, a bone-like tissue. In the root of each tooth, the dentin is covered by a layer of modified bone called cementum. In the crown of each tooth, the dentin is covered by an outer layer of enamel, the hardest substance in the body. See Figure 14.19[18] for an illustration of tooth structure.
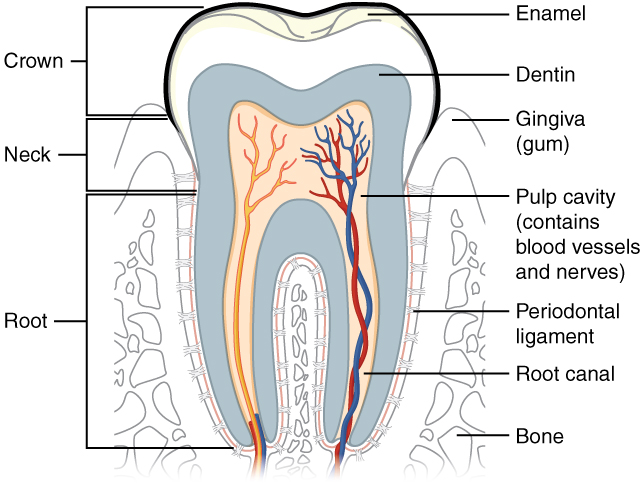
Although enamel protects the underlying dentin and pulp cavity, it is still susceptible to mechanical and chemical erosion, or what is known as tooth decay. The most common form, dental caries (cavities), develops when colonies of bacteria feeding on sugars in the mouth release acids that cause soft tissue inflammation and breakdown of the calcium crystals of the enamel.
Pancreas
The soft, oblong, glandular pancreas lies transversely posterior to the stomach and in the posterior region of the peritoneum (retroperitoneal). Its head is nestled into the “c-shaped” curvature of the duodenum of the small intestine with the body extending to the left about 6 inches and ending as a tapering tail in the hilum of the spleen. The pancreas has both exocrine (secreting digestive enzymes) functions and endocrine (releasing hormones into the blood) functions. See Figure 14.20[19] for an illustration of the pancreas.
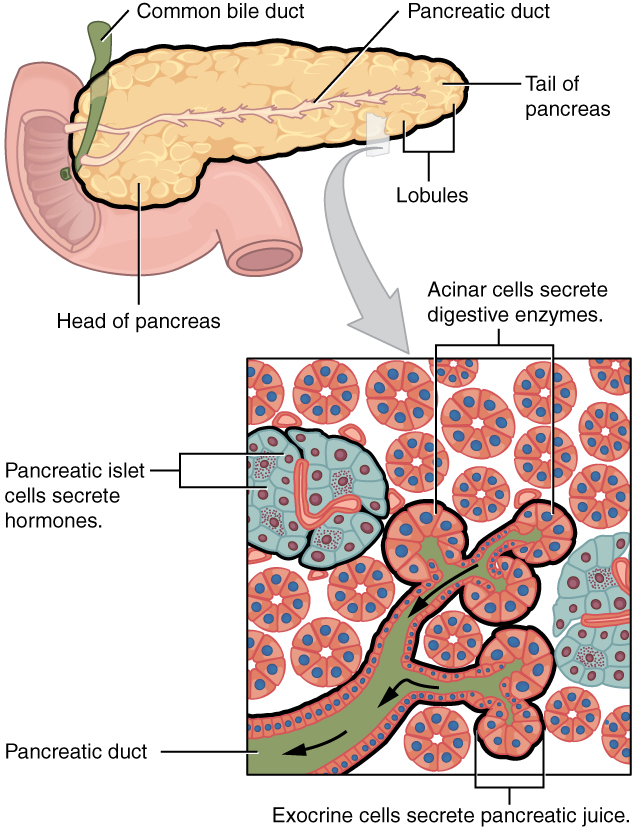
The exocrine part of the pancreas arises as little grape-like cell clusters, each called an acinus (plural = acini) and located at the ends of pancreatic ducts. These acinar cells secrete enzyme-rich pancreatic juice. Scattered among the acini are small islands of endocrine cells, the pancreatic islets. These cells produce the hormones insulin, glucagon, somatostatin, and pancreatic polypeptide.
Pancreatic Juice
The pancreas produces over a liter of pancreatic juice each day. It is clear and made mostly of water, along with some salts, sodium bicarbonate, and several digestive enzymes. Sodium bicarbonate is responsible for the slight alkalinity of pancreatic juice (pH 7.1 to 8.2), which buffers the acidic gastric juice in chyme, inactivates pepsin from the stomach, and creates an optimal environment for the activity of pH-sensitive digestive enzymes in the small intestine. Pancreatic enzymes are active in the digestion of sugars, proteins, nucleic acids, and fats.
The pancreas produces protein-digesting enzymes in their inactive forms, which are then activated in the duodenum. If produced in an active form, they would digest the pancreas (which is exactly what occurs in the disease pancreatitis).
The enzymes that digest starch (pancreatic amylase), fat (pancreatic lipase), and nucleic acids (nucleases) are secreted in their active forms because they do not attack the pancreas.
See Table 14.3a for a summary of digestive enzymes and their functions.
Table 14.3a. Digestive Enzymes
| Enzyme Category | Enzyme Name | Source | Substrate | Product |
|---|---|---|---|---|
| Salivary Enzymes | Lingual lipase | Lingual glands | Triglycerides | Free fatty acids and mono- and diglycerides |
| Salivary Enzymes | Salivary amylase | Salivary glands | Polysaccharides | Disaccharides and trisaccharides |
| Gastric Enzymes | Gastric lipase | Chief cells | Triglycerides | Fatty acids and monoacylglycerides |
| Gastric Enzymes | Pepsin | Chief cells | Proteins | Peptides |
| Brush Border Enzymes | α-Dextrinase | Small intestine | α-Dextrins | Glucose |
| Brush Border Enzymes | Enteropeptidase | Small intestine | Trypsinogen | Trypsin |
| Brush Border Enzymes | Lactase | Small intestine | Lactose | Glucose and galactose |
| Brush Border Enzymes | Maltase | Small intestine | Maltose | Glucose |
| Brush Border Enzymes | Nucleosidases and phosphatases | Small intestine | Nucleotides | Phosphates, nitrogenous bases, and pentoses |
| Brush Border Enzymes | Peptidases | Small intestine | Aminopeptidase: amino acids at the amino end of peptides
Dipeptidase: dipeptides |
Aminopeptidase: amino acids and peptides
Dipeptidase: amino acids |
| Brush Border Enzymes | Sucrase | Small intestine | Sucrose | Glucose and fructose |
| Pancreatic Enzymes | Carboxy-peptidase | Pancreatic acinar cells | Amino acids at the carboxyl end of peptides | Amino acids and peptides |
| Pancreatic Enzymes | Chymotrypsin | Pancreatic acinar cells | Proteins | Peptides |
| Pancreatic Enzymes | Elastase | Pancreatic acinar cells | Proteins | Peptides |
| Pancreatic Enzymes | Nucleases | Pancreatic acinar cells |
|
Nucleotides |
| Pancreatic Enzymes | Pancreatic amylase | Pancreatic acinar cells | Polysaccharides (starches) | α-Dextrins, disaccharides (maltose), trisaccharides (maltotriose) |
| Pancreatic Enzymes | Pancreatic lipase | Pancreatic acinar cells | Triglycerides that have been emulsified by bile salts | Fatty acids and monoacylglycerides |
| Pancreatic Enzymes | Trypsin | Pancreatic acinar cells | Proteins | Peptides |
Liver
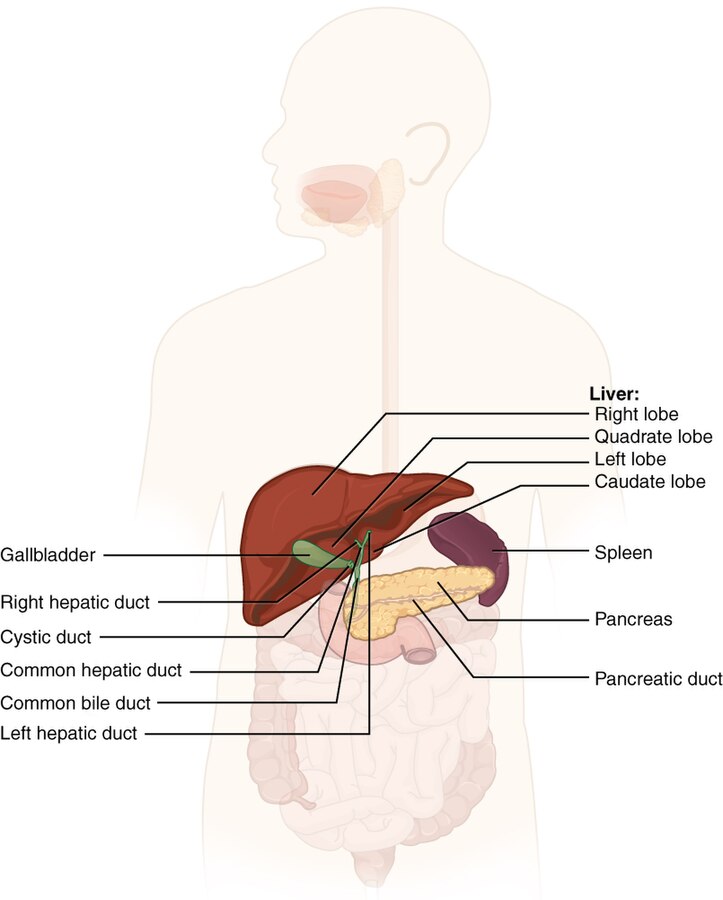
The liver is the largest internal organ in the body, weighing about three pounds in an adult. The liver is divided into two primary lobes: a right lobe and a much smaller left lobe. In the right lobe, some anatomists also identify an inferior quadrate lobe and a posterior caudate lobe that are defined by internal features.
In addition to being an accessory digestive organ, the liver plays important roles in metabolism and regulation. It processes and detoxifies drugs and alcohol, recycles old blood cells, produces plasma proteins, activates vitamin D, and stores glycogen and some vitamins and minerals. The liver lies inferior to the diaphragm in the right upper quadrant of the abdominal cavity and receives protection from the surrounding ribs. See Figure 14.21[20] for an illustration of the liver and other accessory organs.
The hepatic portal vein delivers partially deoxygenated blood containing nutrients absorbed from the small intestine and actually supplies more oxygen to the liver than do the much smaller hepatic arteries. In addition to nutrients, drugs and toxins are also absorbed. After processing the bloodborne nutrients and toxins, the liver releases nutrients needed by other cells back into the blood, which drains into the central vein and then through the hepatic vein to the inferior vena cava. With this hepatic portal circulation, all blood from the GI tract passes through the liver. This largely explains why the liver is the most common site for the metastasis of cancers that originate in the alimentary canal.
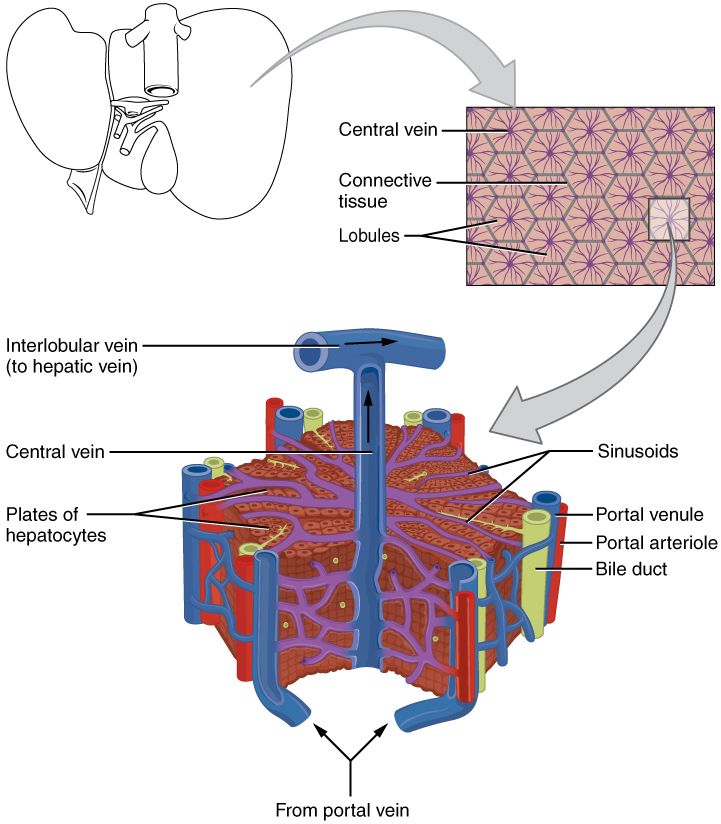
The liver has three main components: hepatocytes, bile canaliculi, and hepatic sinusoids. A hepatocyte is the liver’s main cell type and makes up around 80 percent of the liver’s volume. These cells play a role in a wide variety of secretory, metabolic, and endocrine functions.
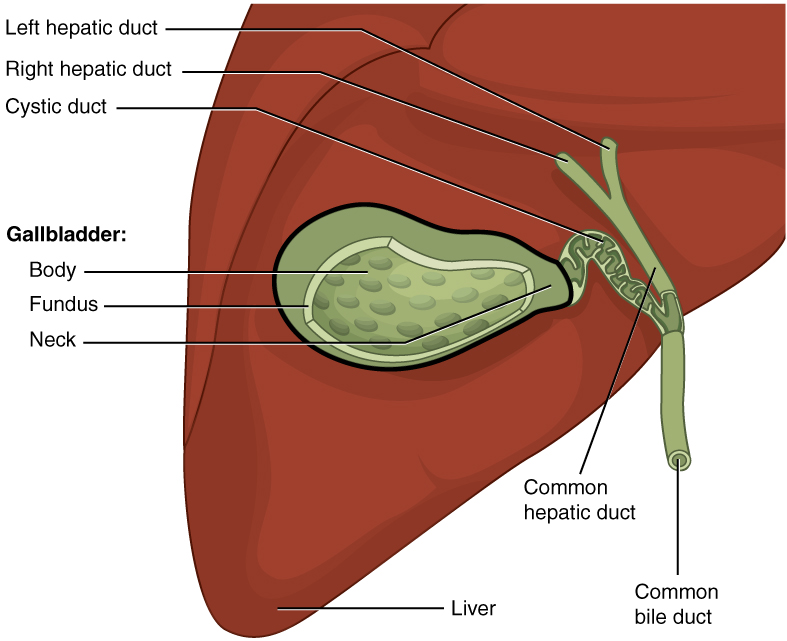
These hepatocytes are arranged into hexagonal units called hepatic lobules. Between adjacent hepatocytes, grooves in the cell membranes provide room for each bile canaliculus (plural = canaliculi). These small ducts collect the bile produced by hepatocytes. From here, bile flows first into bile ductules and then into bile ducts. The bile ducts unite to form the larger right and left hepatic ducts, which themselves merge and exit the liver as the common hepatic duct. This duct then joins with the cystic duct from the gallbladder, forming the common bile duct through which bile flows into the duodenum of the small intestine.
A hepatic sinusoid is an open, porous blood space formed by fenestrated capillaries from nutrient-rich hepatic portal veins and oxygen-rich hepatic arteries. Hepatocytes are tightly packed around the fenestrated endothelium of these spaces, giving them easy access to the blood. From their central position, hepatocytes process the nutrients, toxins, and waste materials carried by the blood. Materials such as bilirubin are processed and excreted into the bile canaliculi. Other materials, including proteins, lipids, and carbohydrates, are processed and secreted into the sinusoids or just stored in the cells until called upon. The hepatic sinusoids combine and send blood to a central vein. Blood then flows through a hepatic vein to the inferior vena cava. This means that blood and bile flow in opposite directions. The hepatic sinusoids also contain star-shaped reticuloendothelial cells (Kupffer cells), phagocytes that remove dead red and white blood cells, bacteria, and other foreign material that enter the sinusoids. The portal triad is a distinctive arrangement around the perimeter of hepatic lobules, consisting of three basic structures: a bile duct, a hepatic artery branch, and a hepatic portal vein branch. See Figure 14.22[21] for an illustration of the microscopic anatomy of the liver.
Bile
Recall that lipids are hydrophobic, that is, they do not dissolve in water. Thus, before they can be digested in the watery environment of the small intestine, large lipid globules must be broken down into smaller lipid globules, a process called emulsification. Bile is a mixture secreted by the liver to accomplish the emulsification of lipids in the small intestine.
Hepatocytes secrete about one liter of bile each day. A yellow-brown or yellow-green alkaline solution (pH 7.6 to 8.6), bile is a mixture of water, bile salts, bile pigments, phospholipids (such as lecithin), electrolytes, cholesterol, and triglycerides.
Bile salts act as emulsifying agents, so they are also important for the absorption of digested lipids. While most constituents of bile are eliminated in feces, bile salts are reclaimed and returned to the liver in the hepatic portal blood. The hepatocytes then excrete the bile salts into newly formed bile.
Bilirubin, the main bile pigment, is a waste product produced when the spleen removes old or damaged red blood cells from the circulation. These breakdown products, including proteins, iron, and toxic bilirubin, are transported to the liver, where proteins and iron are recycled, but bilirubin is excreted in the bile, accounting for the green color of bile. Bilirubin is eventually transformed by intestinal bacteria into stercobilin, a brown pigment that gives your stool its characteristic color.
Hepatocytes work continuously, but bile production increases when fatty chyme enters the duodenum. Between meals, bile is produced but conserved. The valve-like hepatopancreatic ampulla closes, allowing bile to divert to the gallbladder, where it is concentrated and stored until the next meal.
Gallbladder
The gallbladder is 3–4 inches long and is nested in a shallow area on the posterior aspect of the right lobe of the liver. This muscular sac stores, concentrates, and, when stimulated, releases the bile into the duodenum via the cystic and common bile ducts. The gallbladder is divided into three regions. The fundus is the widest portion and tapers medially into the body, which, in turn, narrows to become the neck. The cystic duct is 1–2 cm (less than 1 inch) long and connects the neck and common hepatic duct. When the smooth muscle of the gallbladder contracts, the contents are ejected through the cystic duct and into the common bile duct. See Figure 14.23[22] for an illustration of the gallbladder.
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2402_Layers_of_the_Gastrointestinal_Tract” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “Gray1035” by Henry Gray (1918) Anatomy of the Human Body is in the Public Domain. ↵
- “2406_Structures_of_the_Mouth” by OpenStax College is licensed under CC BY 3.0 ↵
- “2411_Pharynx” by OpenStax College is licensed under CC BY 3.0 ↵
- “2412_The_Esophagus” by OpenStax College is licensed under CC BY 3.0 ↵
- “2414_Stomach” by OpenStax College is licensed under CC BY 3.0 ↵
- “2417_Small_IntestineN” by OpenStax College is licensed under CC BY 3.0 ↵
- “Biliary_system_new” by Vishnu2011 is in the Public Domain. ↵
- “2418_Histology_Small_IntestinesN” by OpenStax College is licensed under CC BY 3.0 ↵
- “2420_Large_Intestine” by OpenStax College is licensed under CC BY 3.0 ↵
- “2433_Teniae_Coli_Haustra_Epiploic_Appendage” by OpenStax College is licensed under CC BY 3.0 ↵
- “2426_Mechanical_and_Chemical_DigestionN” by OpenStax College is licensed under CC BY 3.0 ↵
- “2408_Salivary_Glands” by OpenStax College is licensed under CC BY 3.0 ↵
- “2407_Tongue” by OpenStax College is licensed under CC BY 3.0 ↵
- “2410_Permanent_and_Deciduous_TeethN” by OpenStax College is licensed under CC BY 3.0 ↵
- “2409_Tooth” by OpenStax College is licensed under CC BY 3.0 ↵
- “2424_Exocrine_and_Endocrine_Pancreas” by OpenStax College is licensed under CC BY 3.0 ↵
- “2422_Accessory_Organs” by OpenStax College is licensed under CC BY 3.0 ↵
- “2423_Microscopic_Anatomy_of_Liver” by OpenStax College is in the Public Domain. ↵
- “2425_Gallbladder” by OpenStax College is licensed under CC BY 3.0 ↵
- Michigan Medicine. (2013, February 13). The digestive process - University of Michigan Health System [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=lm3oIX6jjn4 ↵
- Amoeba Sisters. (2021, January 31). Digestive system [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=1UvuBYUbFk0 ↵
The innermost layer of the gastrointestinal tract that secretes mucus and absorbs nutrients.
Secrete mucus and fluid into the lumen.
A thin layer of smooth muscle within the mucosa that helps move the mucosal surface to enhance secretion and absorption.
Underlying layer of connective tissue which helps to support the epithelial layer.
A layer of dense connective tissue beneath the mucosa that contains blood vessels, lymphatics, and nerves, providing support and nourishment to the surrounding tissues.
A layer of the gastrointestinal tract composed of smooth muscle responsible for peristalsis and segmentation, typically organized into an inner circular layer and an outer longitudinal layer.
The outermost layer of the alimentary canal, superficial to the muscularis, consisting of a thin layer of connective tissue and a layer of simple squamous epithelium.
The serous membrane that surrounds several organs in the abdominopelvic cavity, reducing friction between the organs and the abdominal wall.
Refers to organs located behind the peritoneum, the lining of the abdominal cavity, meaning they lie between the peritoneum and the posterior abdominal wall.
Space between the visceral and parietal peritoneal layers.
Acts as a lubricant to minimize friction between the layers of the peritoneum.
The arched shape of the palate allows chewing and breathing to occur simultaneously by separating the oral and nasal cavities, supporting both digestion and respiration.
The hard palate is the bony, anterior part of the palate that provides a rigid floor for the nasal cavity and a surface against which the tongue can press food during chewing.
The soft palate is the muscular, flexible posterior part of the palate that closes off the nasal passages during swallowing and speech.
The uvula is the small, conical projection that hangs from the posterior edge of the soft palate and helps prevent food from entering the nasal cavity during swallowing.
Involved in both digestion and respiration, receiving food and air from the mouth and air from the nasal cavity.
The upper section of the throat behind the nasal cavity that allows air to pass from the nose to the lungs.
The middle section of the throat located behind the mouth that serves as a passageway for both food and air.
The lower part of the throat that directs air to the voice box and food to the swallowing tube, serving as a pathway for both respiration and digestion.
A flap of cartilage that closes over the windpipe during swallowing to prevent food and liquids from entering the airway.
The opening to the larynx.
A muscular tube that connects the pharynx to the stomach.
Controls the movement of food from the pharynx into the esophagus.
Circular muscles that encircle and control the opening of various passages in the body.
Opening in the diaphragm through which the esophagus passes from the thoracic cavity into the abdominal cavity.
Relaxes to let food pass into the stomach and then contracts to prevent stomach acid from backing up into the esophagus.
Helps close the sphincter when no food is being swallowed.
A chronic condition where stomach acid flows backward into the esophagus, causing irritation and heartburn.
Acidic “soup”.
The point where the esophagus connects to and through which food passes into the stomach.
The dome-shaped upper part of the stomach, positioned below the diaphragm and above and to the left of the cardia.
The narrow, funnel-shaped lower end of the stomach that connects to the small intestine.
Large folds formed by the mucosa and submucosa of the stomach when it deflates in the absence of food (singular = ruga).
The process by which stomach contents gradually pass into the small intestine.
An enzyme released from the glands of the tongue.
Necessary for both the production of mature red blood cells and normal neurological functioning.
The shortest part of the small intestine.
A dilated chamber where the pancreatic duct and common bile duct merge and empty their secretions into the duodenum.
The tube that transports bile from the liver and gallbladder to the duodenum.
The channel that carries pancreatic juice from the pancreas to the duodenum.
Regulates the flow of both bile and pancreatic juice from the ampulla into the duodenum.
The middle section of the small intestine, approximately 3 feet long, connecting the duodenum to the ileum.
The longest part of the small intestine, measuring about 6 feet in length.
Deep ridges in the mucosa and submucosa that facilitate absorption.
Located at the opening between the ileum and the large intestine, regulates the flow of chyme from the small intestine to the large intestine.
A pouch-like structure about 2.4 inches long, located below the ileocecal valve, which receives contents from the ileum and continues absorption of water and salts.
A winding, approximately 3-inch-long tube attached to the cecum that contains lymphatic tissue and is generally considered vestigial with a possible immune role.
The final 8 inches of the gastrointestinal tract.
The final 1.5–2 inches of the large intestine that opens to the exterior at the anus and contains both internal and external sphincters to regulate defecation.
Three bands of smooth muscle that make up the longitudinal muscle layer of the muscularis of the large intestine, except at its terminal end.
Pouches formed by the contraction of the teniae coli that give the colon its wrinkled appearance and aid in the movement of fecal material.
Small, fat-filled sacs of visceral peritoneum attached to the teniae coli of the colon.
A surgical procedure involving the removal of all or part of the colon.
Composed of undigested food residues, unabsorbed digested substances, millions of bacteria, old epithelial cells from the GI mucosa, inorganic salts, and enough water to let it pass smoothly out of the body.
A voluntary process of contracting your diaphragm and abdominal wall muscles and closing your glottis to aid in defecation.
A condition characterized by infrequent, difficult, or painful bowel movements, often caused by slow movement of stool through the colon.
A condition in which waste moves too quickly through the intestines, preventing adequate water absorption and resulting in loose, watery stools.
Exocrine structures in the mouth and tongue that continuously secrete saliva, aiding in digestion and oral hygiene.
The largest salivary glands located near the ears that secrete a watery saliva rich in enzymes to begin starch digestion.
Smallest salivary glands located beneath the tongue that produce mostly mucus-rich saliva to lubricate the mouth and food.
Salivary glands located beneath the lower jaw that produce a mixture of serous (watery) and mucus saliva to aid in digestion and oral lubrication.
Composed mostly of water (99.4%), with the remaining 0.6% containing ions, glycoproteins, enzymes, growth factors, and waste products, where the key digestive enzyme is salivary amylase.
An enzyme in saliva that begins the chemical digestion of starches by breaking them down into simpler sugars.
The strongest muscle in the body.
Small, raised structures on the tongue's surface that enhance grip and contain taste buds.
Mushroom shaped and cover a large area of the tongue.
Another word for swallowing—the movement of food from the mouth to the stomach.
Organs similar to bones that are used to tear, grind, and otherwise mechanically break down food.
Soft tissues that line the alveolar processes and surround the necks of the teeth.
Primary or baby teeth.
The sharp front teeth you use for biting into food.
(Or canines) teeth located next to the incisors with pointed edges designed to tear and pierce tough or fleshy foods.
Teeth located behind the cuspids that have broad, flat surfaces for crushing and grinding food.
Large teeth located at the back of the mouth with broad, flat surfaces designed for grinding and chewing food thoroughly.
The part of a tooth that is embedded within sockets of the upper and lower jaw bones, containing a pulp cavity with nerves and blood vessels.
A layer of modified bone tissue that covers the dentin in the root portion of each tooth.
The mechanical and chemical erosion of tooth enamel that can damage the underlying dentin and pulp cavity.
A long, thin organ located mostly behind the lower part of the stomach that produces hormones and digestive enzymes.
A small, grape-like cluster of cells in the pancreas that produces and secretes digestive enzymes as part of its exocrine function.
A digestive fluid produced by the pancreas containing enzymes and bicarbonate that aid in digestion and neutralize stomach acid.
Clusters of cells in the pancreas that produce hormones like glucagon, insulin, somatostatin, and pancreatic polypeptide.
The largest internal organ in the body, weighing about three pounds in an adult.
Delivers nutrient-rich, partially deoxygenated blood from the small intestine to the liver, supplying more oxygen to the liver than the smaller hepatic arteries.
The liver’s main cell type, comprising about 80% of its volume, responsible for diverse secretory, metabolic, and endocrine functions.
An open, porous blood space formed by fenestrated capillaries from nutrient-rich hepatic portal veins and oxygen-rich hepatic arteries.
The process where large fat globules are broken down into smaller droplets, increasing their surface area for easier digestion by enzymes.
A mixture secreted by the liver to accomplish the emulsification of lipids in the small intestine.
The main bile pigment and a waste product produced when the spleen removes old or damaged red blood cells from the circulation.
A small, 3–4 inch-long organ located on the posterior side of the liver’s right lobe that stores and concentrates bile.

