13.3 Anatomy of the Respiratory System
Anatomy of the Respiratory System[1]
Anatomically, the respiratory system can be divided into upper and lower respiratory systems. The upper respiratory system consists of the nose and pharynx, while the lower respiratory system includes the larynx, trachea, bronchial tree, and alveoli.
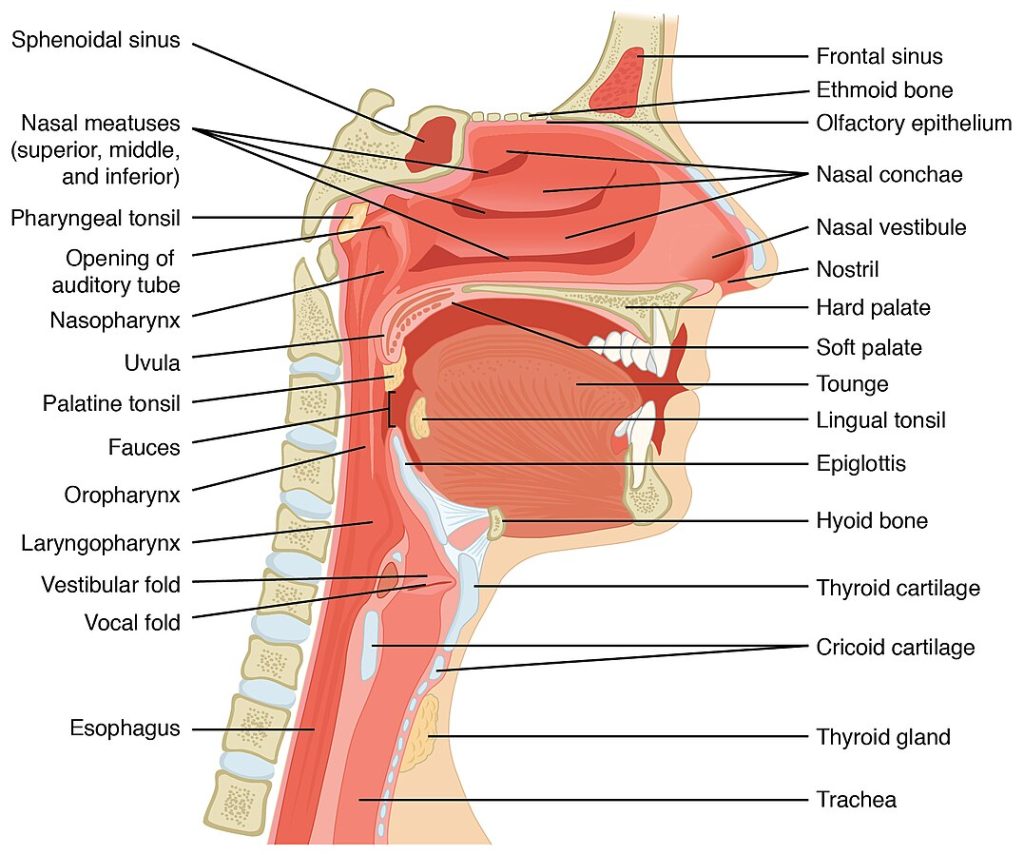
See Figure 13.1[2] for an illustration of the major structures of the respiratory system.

Upper Respiratory System
See Figure 13.2[3] for an illustration of the structures of the upper airway.
Nose
The main entrance and exit for the respiratory system is the nose. The nose can be divided into two major sections: the external nose (outward projection) and the internal nose (the nasal cavity or the space inside the nose).
The nares (nostrils) allow air into the nasal cavity, which is separated into left and right sections by the nasal septum. The floor of the nasal cavity (and the roof of the mouth) is composed of the palate. The anterior hard palate is composed of bone. The posterior soft palate consists of muscle tissue.
Each lateral wall of the nasal cavity has three bony projections called the superior, middle, and inferior nasal conchae. Nasal conchae serve to increase the surface area of the nasal cavity and to disrupt the flow of air as it enters the nose, causing air to bounce along the epithelium, where it is cleaned, warmed, and humidified.
At the posterior region of the nasal cavity, air exits through the internal nares, the openings between the nasal cavity and the nasopharynx.
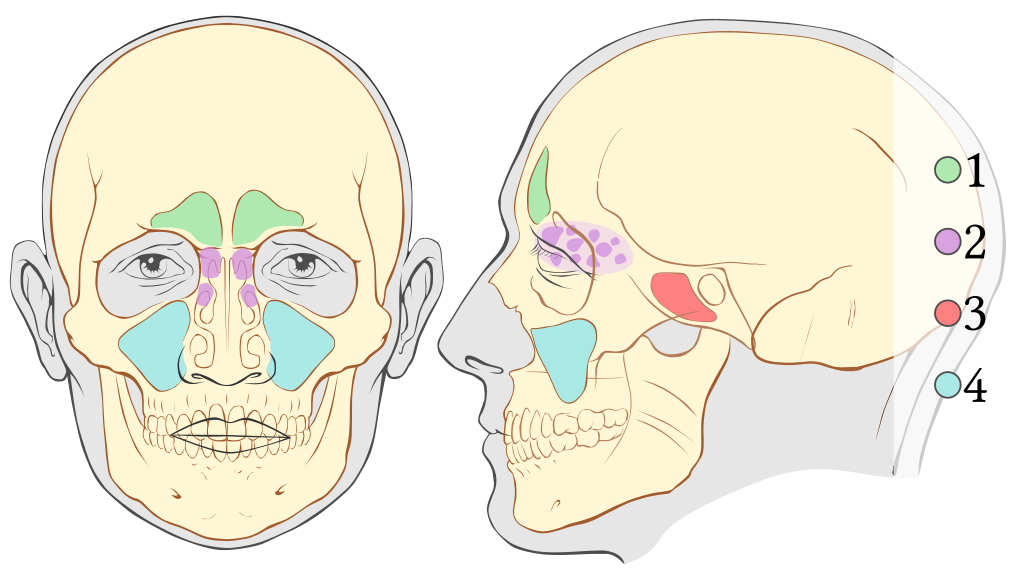
Several bones that form the walls of the nasal cavity have air-containing spaces called the paranasal sinuses, which serve to warm and humidify incoming air. Sinuses are lined with a mucous membrane. Each paranasal sinus is named for its associated bone: frontal sinus, maxillary sinus, sphenoidal sinus, and ethmoidal sinus. The sinuses produce mucus and lighten the weight of the skull.
The nares and the anterior portion of the nasal cavity are lined with mucous membranes containing sebaceous glands and hairs to prevent the passage of large debris, such as dirt, through the nasal cavity. An olfactory epithelium used to detect odors is found deeper in the nasal cavity.
See Figure 13.3[4] for an illustration of the sinuses.
Pharynx
The pharynx (throat) is a tube formed by skeletal muscle and lined by a mucous membrane that is continuous with that of the nasal cavities. The pharynx is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx. See Figure 13.4[5] for an illustration of these three regions of the pharynx.
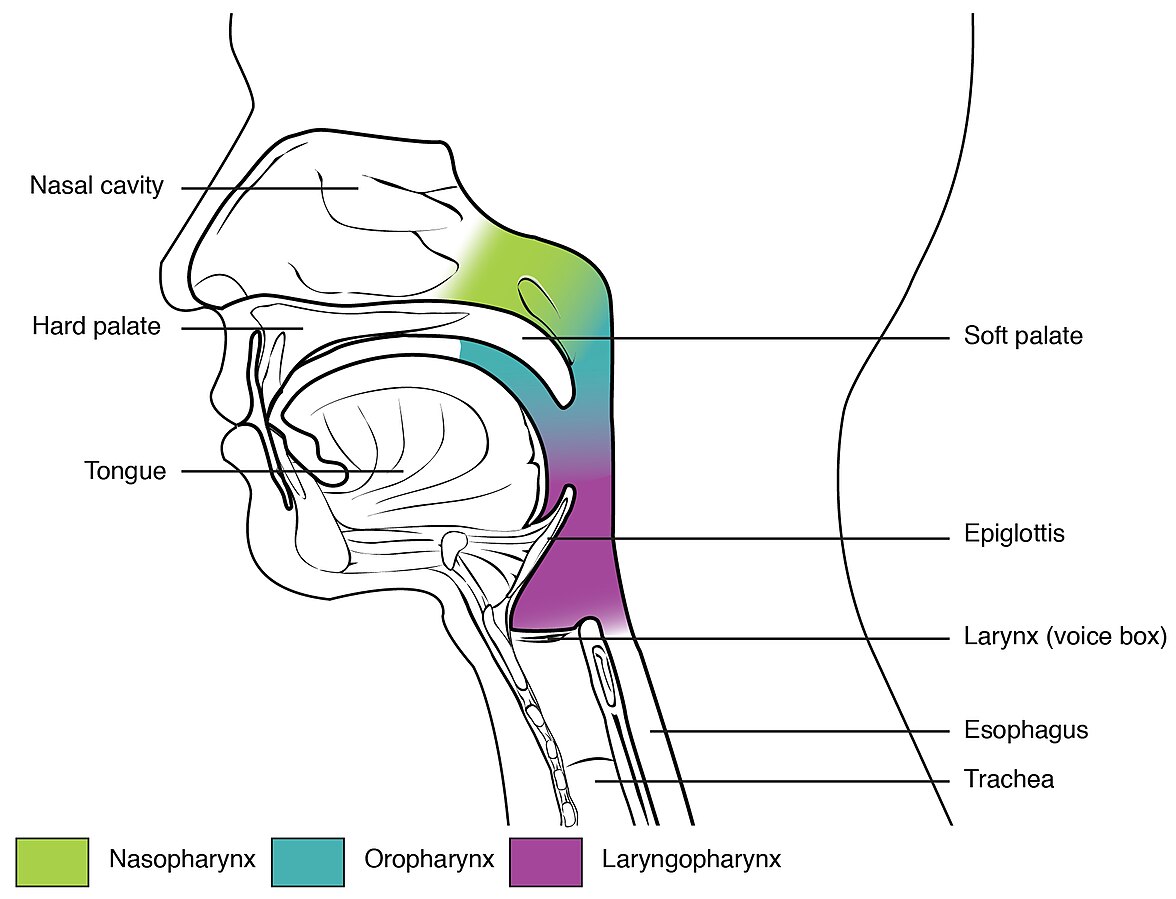
The nasopharynx is posterior to the nasal cavity, and it serves only as an airway. At the posterior aspect of the nasopharynx is the pharyngeal tonsil. A pharyngeal tonsil, also called an adenoid, is a mass of lymphoid tissue similar to a lymph node. The function of the pharyngeal tonsil is not well understood, but it contains a rich supply of lymphocytes and is covered with ciliated epithelium that traps and destroys pathogens that enter during inhalation. The pharyngeal tonsil is large in children but tends to get smaller with age and may even disappear.
The uvula is a small, teardrop-shaped structure located at the apex of the soft palate. Both the uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx to prevent ingested materials from entering the nasal cavity. In addition, auditory (eustachian) tubes from the ear open into the nasopharynx. This connection is why colds often lead to ear infections. Refer back to Figure 13.2 to view the uvula.
The inferior nasopharynx leads into the oropharynx, a passageway for both air, liquids, and food. The oropharynx contains two distinct sets of tonsils, the palatine and lingual tonsils. The palatine tonsils are a pair of structures located on each side of the oropharynx. The lingual tonsils are located at the base of the tongue. Similar to the pharyngeal tonsil, the palatine and lingual tonsils are composed of lymphoid tissue and trap and destroy pathogens entering the body through the oral or nasal cavities.
The laryngopharynx (also known as the hypopharynx) is inferior to the oropharynx and posterior to the larynx. It continues the passageway for food and air until the digestive and respiratory systems split. Anteriorly, the laryngopharynx opens into the larynx, and posteriorly, it enters the esophagus.
Lower Respiratory System
Larynx
The larynx (also known as the voice box) is a cartilaginous structure that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs. The larynx is composed of nine pieces of cartilage. The three largest cartilage pieces form the major structure of the larynx—the thyroid cartilage (anterior), epiglottis (superior), and cricoid cartilage (inferior).
The thyroid cartilage is the largest piece of cartilage that makes up the larynx. The thyroid cartilage consists of the laryngeal prominence, or “Adam’s apple,” which tends to be more prominent in males due to the effects of testosterone. The thick cricoid cartilage forms a ring, with a wide posterior region and a thinner anterior region. Both these structures are made of hyaline cartilage. The cricothyroid ligament (or membrane) is a structure located between these two cartilages. It is the structure that is cut during a cricothyrotomy for emergency airway access if the upper airway is obstructed.
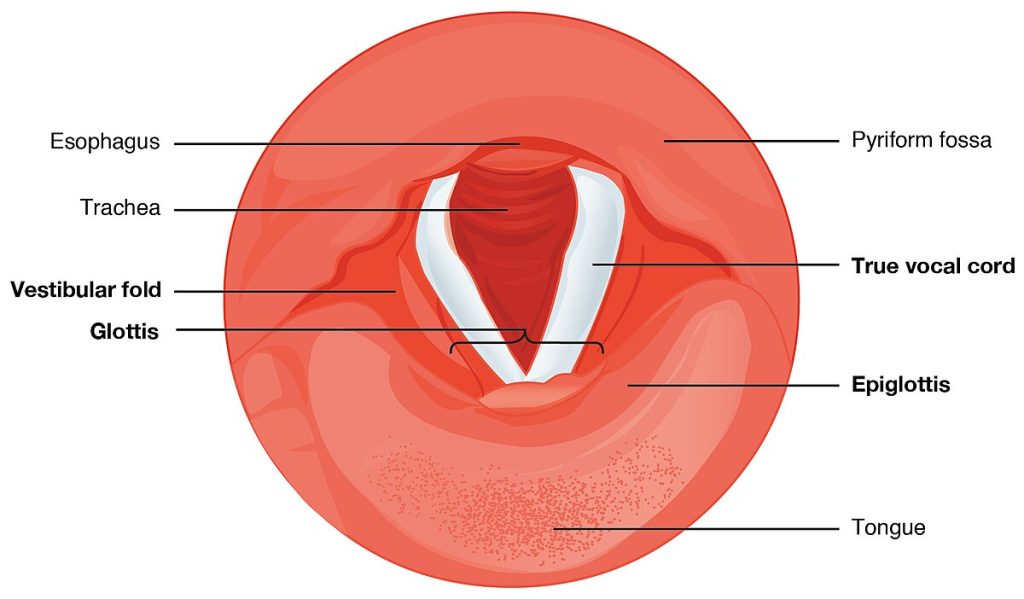
The epiglottis is a very flexible piece of elastic cartilage that covers the opening of the larynx during swallowing to prevent food and drink from entering the lower airway. The glottis is the opening inside the larynx, which also contains the vocal folds or cords. Air passes through this opening when breathing and making speech.
See Figure 13.5[6] for an illustration of the larynx.

The true vocal cords (also called vocal folds) are a pair of white, membranous ligaments attached to cartilage pieces of the larynx. The inner edges of the true vocal cords are free, allowing vibrations to produce sound when muscles inside the larynx contract. The size of the vocal cords differs between individuals, producing voices with different pitch ranges. Folds in males tend to be larger than those in females and create a deeper voice. See Figure 13.6[7] for an illustration of the vocal cords and the glottis.
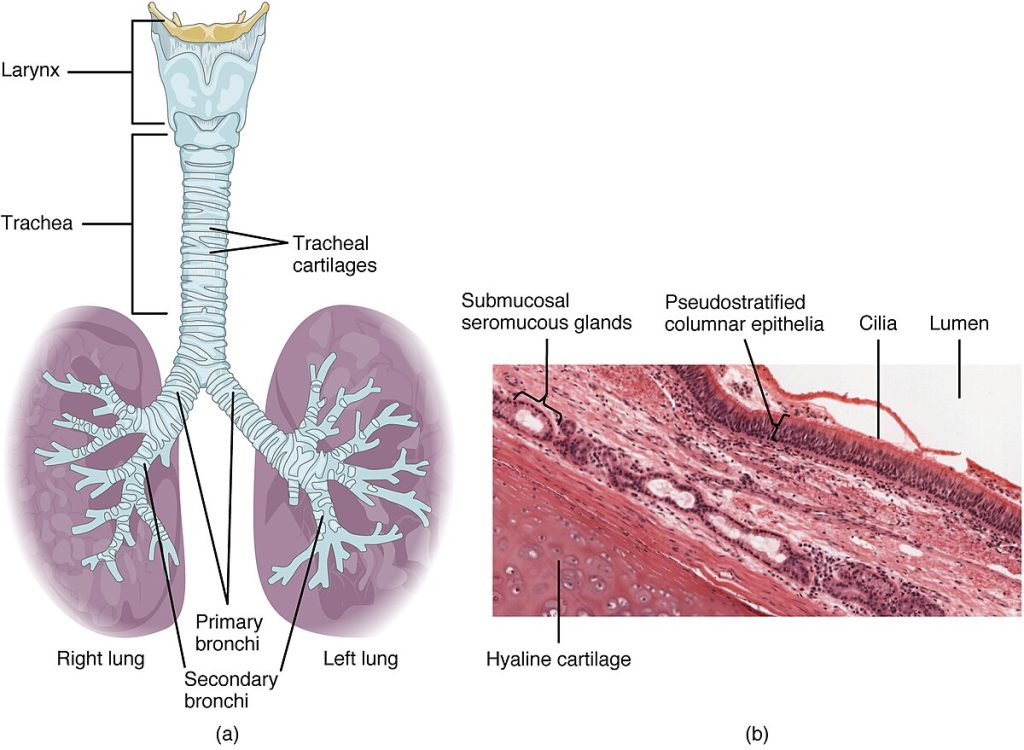
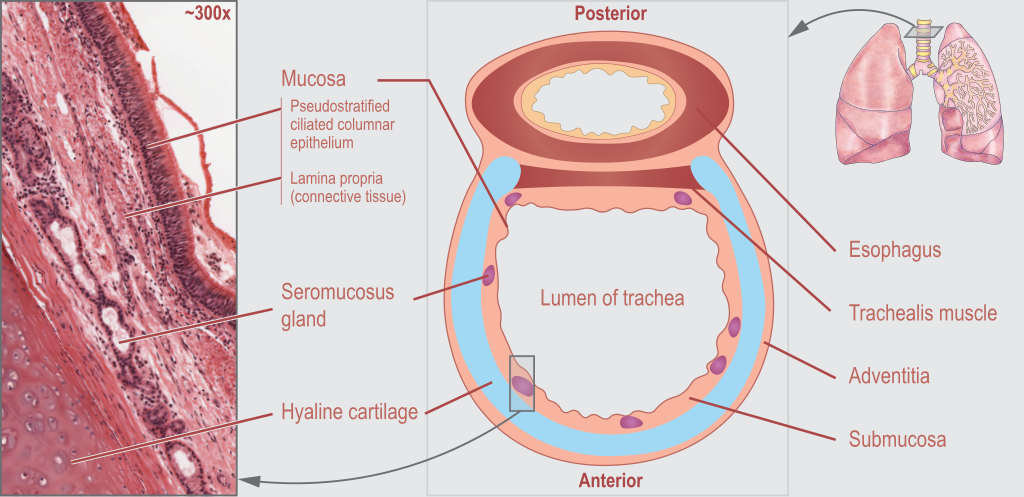
Trachea
The trachea (windpipe) is an approximately 5-inch-long tubular airway that extends from the larynx inferiorly toward the lungs. The trachea is formed by 16-20 C-shaped pieces of hyaline cartilage that are connected by dense connective tissue. The rings of cartilage provide structural support and prevent the trachea from collapsing when breathing. The esophagus borders the trachea posteriorly.
The trachea is lined with a mucous membrane containing ciliated pseudostratified columnar epithelial cells. Cilia help move mucus and debris with a constant beating motion, sweeping materials up towards the throat to be swallowed.
See Figure 13.7[8] for an illustration of the trachea and Figure 13.8[9] for a cross section of the trachea and the esophagus.
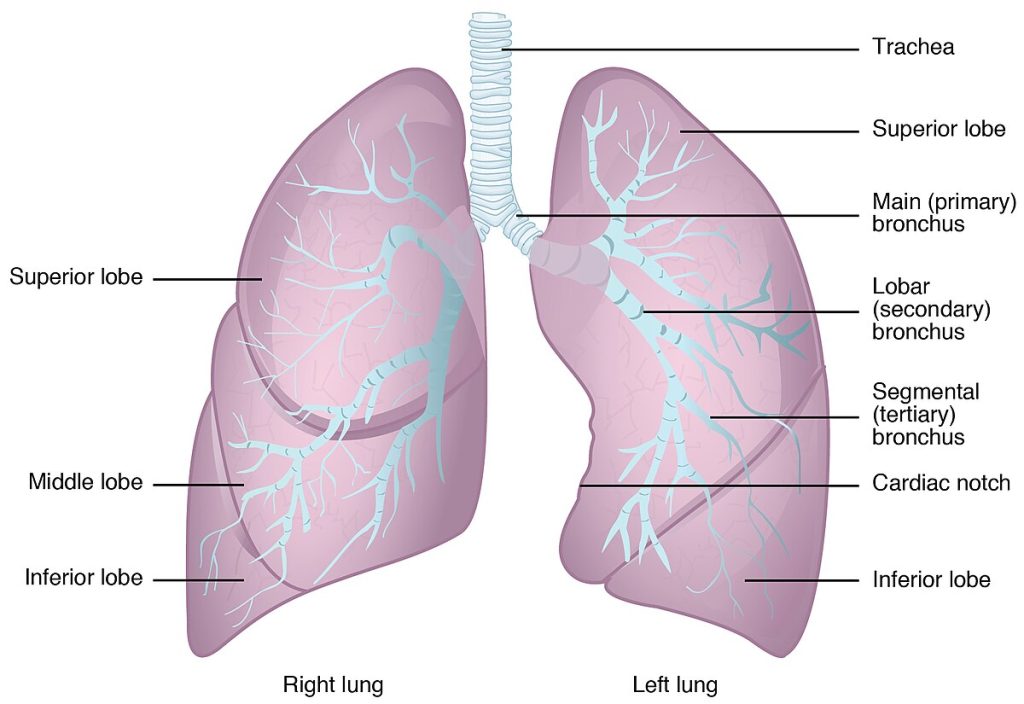
Lungs
The lungs are a pair of pyramid-shaped organs connected to the trachea by the right and left primary bronchi. The inferior surface of the lungs is bordered by the diaphragm.
The right lung is shorter and wider than the left lung, and the left lung occupies a smaller volume than the right. The cardiac notch is an indentation on the surface of the left lung that allows space for the heart.
Each lung is composed of smaller units called lobes. The right lung consists of three lobes: the superior, middle, and inferior lobes. The left lung consists of two lobes: the superior and inferior lobes. See Figure 13.9[10] for an illustration of the lungs.
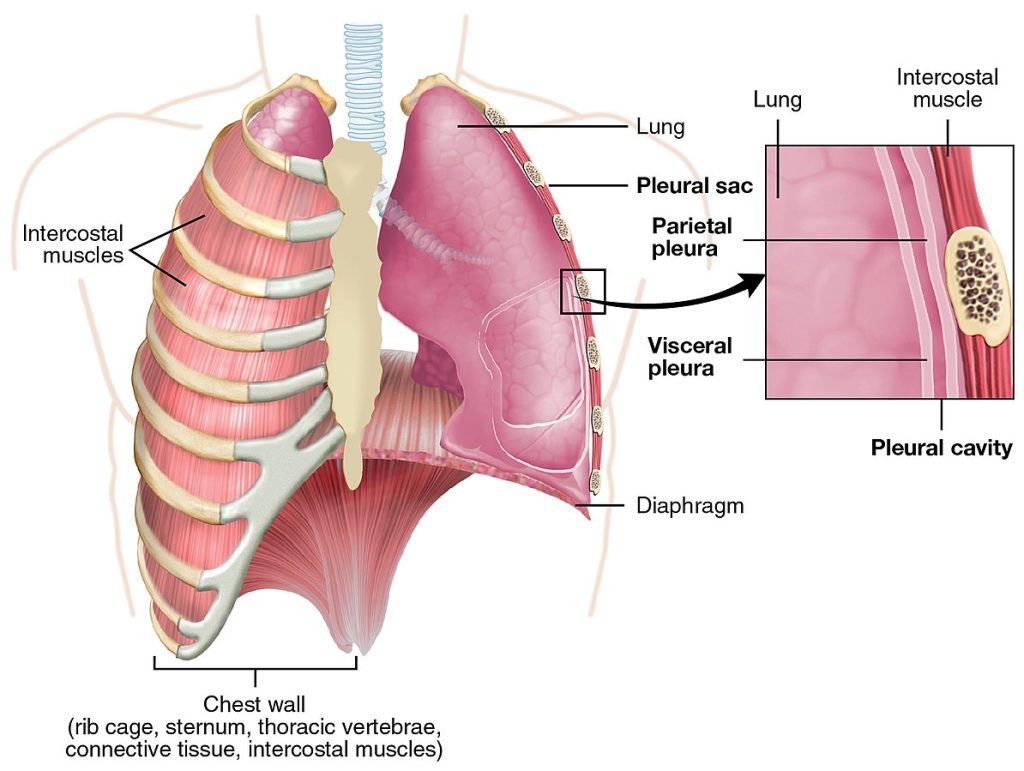
Pleural Membrane (Pleura)
Each lung is enclosed within a cavity that is surrounded by a pleural membrane (also known as the pleura). The pleura (plural = pleurae) is a serous membrane that surrounds each lung. The pleurae consist of two layers. The visceral pleura is the layer that directly covers the lungs, and the parietal pleura is the outer layer that lines the thoracic cavity, the mediastinum, and the diaphragm.
The pleural cavity is the space between the visceral and parietal layers that contains pleural fluid. Pleural fluid is secreted by both pleural layers and acts to lubricate their surfaces. This lubrication reduces friction between the two layers. See Figure 13.10[11] for an illustration of the pleurae and pleural cavity.
Bronchial Tree
The trachea branches into the right and left primary bronchi (singular = bronchus) at the carina. The carina is a raised structure that contains specialized nervous tissue that causes violent coughing if a foreign body, such as food, is present. The right primary bronchus enters the right lung, and the left primary bronchus enters the left lung. Refer back to Figure 13.6 for an illustration of the right and left primary bronchi.
The primary bronchi enter the lungs at the hilum, a concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs. The bronchi continue to branch into a bronchial tree. A bronchial tree (or respiratory tree) is the collective term used for these multiple-branched bronchial tubes. Rings of cartilage, similar to those of the trachea, support the structure of the bronchi and prevent their collapse.
Primary bronchi branch into secondary bronchi, which enter each lobe of the lung. The right lung typically has three lobes, so there are three secondary bronchi. The left lung typically has two lobes, so there are two secondary bronchi. The secondary bronchi then divide again into several tertiary bronchi. These bronchi branch several more times before they turn into bronchioles.
Bronchioles, which are about 1 mm in diameter, further branch until they become the tiny terminal bronchioles, which lead to the alveoli, the air sacs which perform gas exchange. In total there are roughly 26 branches of bronchi.
An important distinction between bronchi and bronchioles is that the walls of bronchi contain cartilage whereas the walls of bronchioles do not. Because the bronchioles don’t contain cartilage, the smooth muscle walls of them can constrict and dilate to change the diameter of the bronchioles to increase or decrease airflow. See Figure 13.11[12] for an illustration of a terminal bronchiole and alveoli.
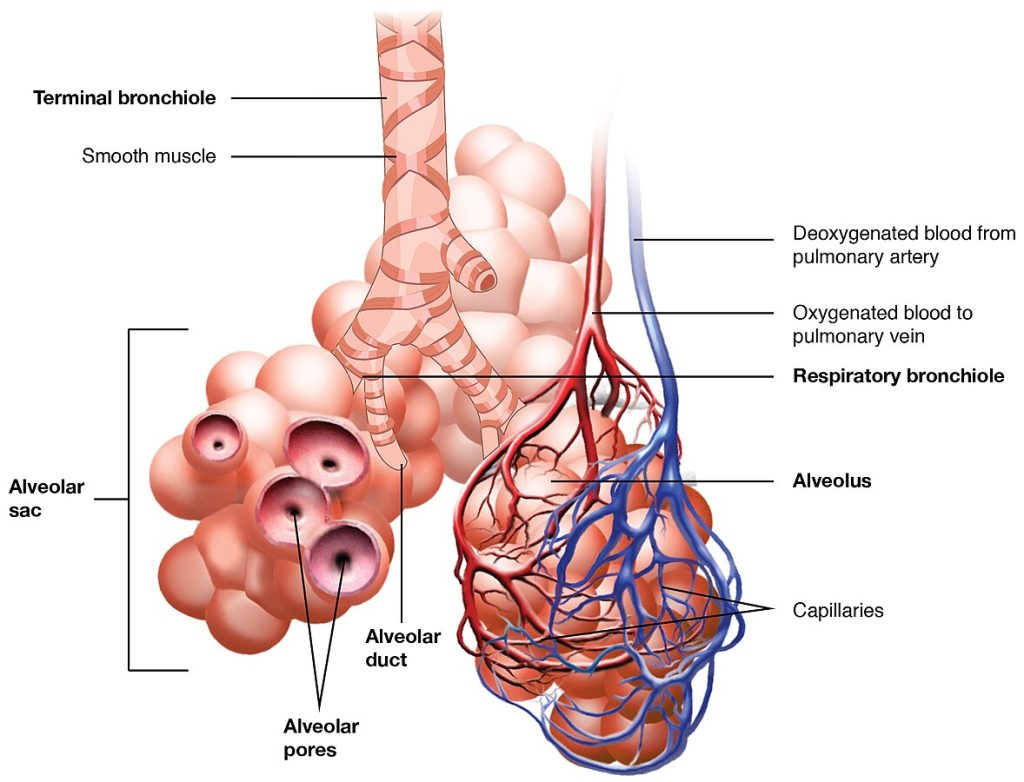
Alveoli
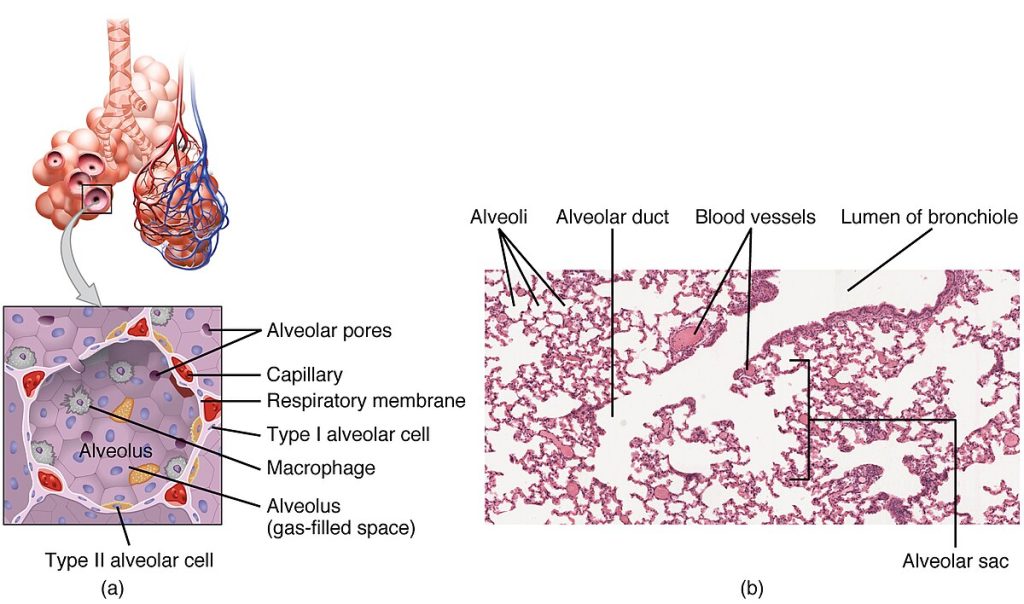
Alveoli (singular = alveolus) are small, grape-like air sacs surrounded by pulmonary blood capillaries. The alveoli and capillary membranes form a very thin respiratory membrane. The thinness of the respiratory membrane allows for simple diffusion of oxygen and carbon dioxide. After inhalation, oxygen diffuses from the alveolus into the pulmonary capillary, and carbon dioxide diffuses from the pulmonary capillary into the alveolus to then be exhaled. Alveoli have elastic walls that allow them to stretch during inhalation, which greatly increases the surface area available for gas exchange.
The wall of each alveolus consists of three major cell types: type I alveolar cells, type II alveolar cells, and alveolar macrophages. A type I alveolar cell is a simple squamous epithelial cell of the alveoli, which constitute up to 97 percent of the alveolar surface area. These cells are highly permeable to gases. Type II alveolar cells are scattered among the type I cells and secrete pulmonary surfactant, a slippery fluid that reduces the surface tension of the alveoli and prevents them from collapsing. Roaming around the alveolar wall are alveolar macrophages (also called dust cells), phagocytic cells of the immune system that remove inhaled debris and pathogens that have reached the alveoli.
See Figure 13.12[13] for an illustration of alveoli and their cells.
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2301_Major_Respiratory_Organs” by OpenStax College is licensed under CC BY 3.0 ↵
- “2303_Anatomy_of_Nose-Pharynx-Mouth-Larynx” by OpenStax College is licensed under CC BY 3.0 ↵
- “Paranasal_sinuses_numbers” by Michał Komorniczak is licensed under CC BY-SA 3.0 ↵
- “2305_Divisions_of_the_Pharynx” by OpenStax College is licensed under CC BY 3.0 ↵
- “2306_The_Larynx” by OpenStax College is licensed under CC BY 3.0 ↵
- “2307_Cartilages_of_the_Larynx” by OpenStax College is licensed under CC BY 3.0 ↵
- “2308_The_Trachea” by OpenStax College is licensed under CC BY 3.0 ↵
- “Cross_section_of_a_trachea_and_esophagus” by PBrieux is licensed under CC BY-SA 4.0 ↵
- “2312_Gross_Anatomy_of_the_Lungs” by OpenStax College is licensed under CC BY 3.0 ↵
- “2313_The_Lung_Pleurea” by OpenStax College is licensed under CC BY 3.0 ↵
- “2309_The_Respiratory_Zone” by OpenStax College is licensed under CC BY 3.0 ↵
- “2310_Structures_of_the_Respiratory_Zone” by OpenStax College is licensed under CC BY 3.0 ↵
Allow air into the nasal cavity.
Three bony projections on each lateral wall of the nasal cavity that increase surface area and create turbulence, helping warm, humidify, and filter incoming air.
The openings between the nasal cavity and the nasopharynx.
Hollow, air-filled spaces located within certain bones of the skull.
Involved in both digestion and respiration, receiving food and air from the mouth and air from the nasal cavity.
The upper section of the throat behind the nasal cavity that allows air to pass from the nose to the lungs.
The uvula is the small, conical projection that hangs from the posterior edge of the soft palate and helps prevent food from entering the nasal cavity during swallowing.
The middle section of the throat located behind the mouth that serves as a passageway for both food and air.
The lower part of the throat that directs air to the voice box and food to the swallowing tube, serving as a pathway for both respiration and digestion.
A cartilaginous structure that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs. Also known as the voicebox.
A flap of cartilage that closes over the windpipe during swallowing to prevent food and liquids from entering the airway.
A pair of white, membranous ligaments attached to cartilage pieces of the larynx. Also called vocal folds.
An approximately 5-inch-long tubular airway that extends from the larynx inferiorly toward the lungs. Also called the windpipe.
Short, hair-like projections from the cell surface that are involved in movement of the cell or the movement of substances along the cell surface.
A pair of pyramid-shaped organs connected to the trachea by the right and left primary bronchi.
An indentation on the surface of the left lung that allows space for the heart.
The space between the visceral and parietal layers that contains pleural fluid.
A lubricating fluid secreted by the pleural layers that reduces friction between the lung membranes during breathing.
A raised structure that contains specialized nervous tissue that causes violent coughing if a foreign body, such as food, is present.
The collective term used for these multiple-branched bronchial tubes.
Small airways about 1 mm in diameter that branch extensively and lead to terminal bronchioles and alveoli, where gas exchange occurs.
Small, grape-like air sacs surrounded by pulmonary blood capillaries.
A thin barrier formed by alveolar and capillary walls that allows efficient gas exchange by simple diffusion of oxygen and carbon dioxide.
A slippery fluid that reduces the surface tension of the alveoli and prevents them from collapsing.

