12.4 Immune System
Immune System[1]
The immune system can be divided into two overlapping mechanisms to destroy a wide variety of pathogens: the nonspecific (innate) immune response and the specific (adaptive) immune response. The nonspecific immune response is relatively rapid but nonspecific in that it will respond to any pathogen, but as a drawback, this response does not create a memory of the pathogen. Nonspecific immunity will, however, help to initiate the specific (adaptive) immune response, which is slower in its development during an initial infection with a pathogen, but is highly specific and effective at attacking pathogens. The specific (adaptive) immune response requires exposure to a pathogen for the body to recognize it as a threat and respond. After the adaptive immune system has been exposed to a pathogen, it develops memory cells to recognize this pathogen in the future and quickly mount a defense.
Nonspecific (Innate) Immune Response
The innate immune response begins with physical barriers that prevent pathogens from entering the body, destroy them after they enter, or flush them out before they can establish themselves in the body’s soft tissues. Nonspecific barrier defenses are part of the body’s most basic defense mechanisms. The nonspecific defenses are not a response to infections, but they are continuously working to protect against a broad range of pathogens. The different modes of nonspecific defenses are associated with the external surfaces of the body, where pathogens may try to enter. Barrier defenses are summarized in Table 12.4a.
Table 12.4a. Barrier Defenses[2]
| Structure | Protective Aspect |
|---|---|
| Skin – Epidermal Surface | Keratinized cells of surface, Langerhans cells |
| Skin – Sweat/Oil Glands | Low pH, washing action |
| Mouth – Salivary Glands/Saliva | Lysozymes |
| Stomach – Gastric Juice | Low pH |
| Mucosal Surfaces | Mucus |
| Normal Flora (nonpathogenic bacteria) of Mucosal Tissues | Prevent pathogens from growing on mucosal surfaces |
The skin is the primary barrier to microorganisms entering the body. The skin is covered with multiple layers of dead, keratinized epithelium that is too dry for bacteria to grow on, but as these cells are continuously sloughed off from the skin, they carry bacteria and other pathogens with them. Additionally, sweat and other skin secretions may lower pH, contain toxic lipids, and physically wash microbes away. In the mouth, saliva is rich in lysozyme, an enzyme that destroys bacteria. Furthermore, the acidic environment of the stomach is fatal to many pathogens that enter the gastrointestinal system. Additionally, the mucus layer of the gastrointestinal tract, respiratory tract, reproductive tract, urinary tract, eyes, ears, and nose traps microbes and debris and facilitates their removal. In the upper respiratory tract, ciliated epithelial cells move potentially contaminated mucus upwards to the mouth, where it is swallowed and ends up in the harsh acidic environment of the stomach. Considering how often we breathe compared to how often we eat or perform other activities that expose us to pathogens, it is not surprising that multiple barrier mechanisms have evolved to work together to protect this vital area.
Cells of the Innate Immune Response
A phagocyte is a cell that is able to surround and engulf a particle or cell, a process called phagocytosis. The phagocytes of the immune system engulf other particles or cells, either to clean an area of debris or old cells or to kill pathogenic organisms such as bacteria. The phagocytes are the body’s fast-acting, first line of immunological defense against organisms that have breached barrier defenses and have entered the vulnerable tissues of the body.
Many cells of the immune system have a phagocytic ability, at least at some point during their life cycles. Phagocytosis is an important and effective mechanism of destroying pathogens during innate immune responses. The phagocyte takes the organism inside itself as a phagosome, which subsequently fuses with a lysosome and its digestive enzymes, effectively killing many pathogens. On the other hand, some bacteria, including Mycobacteria tuberculosis, the cause of tuberculosis, may be resistant to these enzymes and are, therefore, much more difficult to clear from the body. Macrophages, neutrophils, and dendritic cells are the major phagocytes of the immune system.
A macrophage is an irregularly shaped phagocyte that is the most versatile of the phagocytes in the body. Macrophages can move through tissues and squeeze through capillary walls. They not only participate in innate immune responses but also have evolved to cooperate with lymphocytes as part of the specific immune response. Macrophages exist in many tissues of the body, either freely roaming or fixed within specific tissues such as lymph nodes. When pathogens breach the body’s barrier defenses, macrophages are the first line of defense. They are called different names, depending on the tissue: Kupffer cells in the liver, histiocytes in connective tissue, and alveolar macrophages in the lungs.
A neutrophil is a phagocytic cell that is attracted to infected tissues. Neutrophils can be thought of as military reinforcements that are called into a battle to hasten the destruction of the enemy. Although usually thought of as the primary pathogen-killing cell of the inflammatory process of the innate immune response, new research has suggested that neutrophils play a role in the adaptive immune response as well, just as macrophages do.
A monocyte is a circulating cell that differentiates into either a macrophage or dendritic cell, which can be rapidly attracted to areas of infection.
See Table 12.4b for a summary of phagocytic cells of the immune system.
Table 12.4b. Phagocytic Cells of the Innate Immune System[3]
| Cell | Cell type | Primary Location | Function in the Innate Immune Response |
|---|---|---|---|
| Macrophage | Agranulocyte | Body cavities/organs | Phagocytosis |
| Neutrophil | Granulocyte | Blood | Phagocytosis |
| Monocyte | Agranulocyte | Blood | Precursor of macrophage/dendritic cell |
Natural Killer Cells
Natural killer (NK) cells are a type of lymphocyte that have the ability to cause apoptosis (programmed cell death) in cells infected with intracellular pathogens such as bacteria or viruses. They also destroy other abnormal cells, such as cancer cells. NK cells recognize these cells by mechanisms that are still not well-understood.
Inflammatory Response
The hallmark of the innate immune response is inflammation. Inflammation is something everyone has experienced when injured. For example, cutting a finger, stubbing a toe, or any injury that causes tissue damage will result in inflammation with four characteristics of heat, redness, pain, and swelling. “Loss of function” is sometimes mentioned as a fifth characteristic of inflammation. Note that inflammation does not have to be initiated by an infection but can also be caused by tissue injuries.
The release of damaged cell contents into the site of injury is enough to stimulate the inflammatory response, even if no pathogens enter. For example, hitting your thumb with a hammer initiates the inflammatory response. The inflammatory reaction brings in phagocytic cells to the damaged area to clear cellular debris and to set the stage for wound repair. See Figure 12.10[4] for an illustration of the inflammatory response.
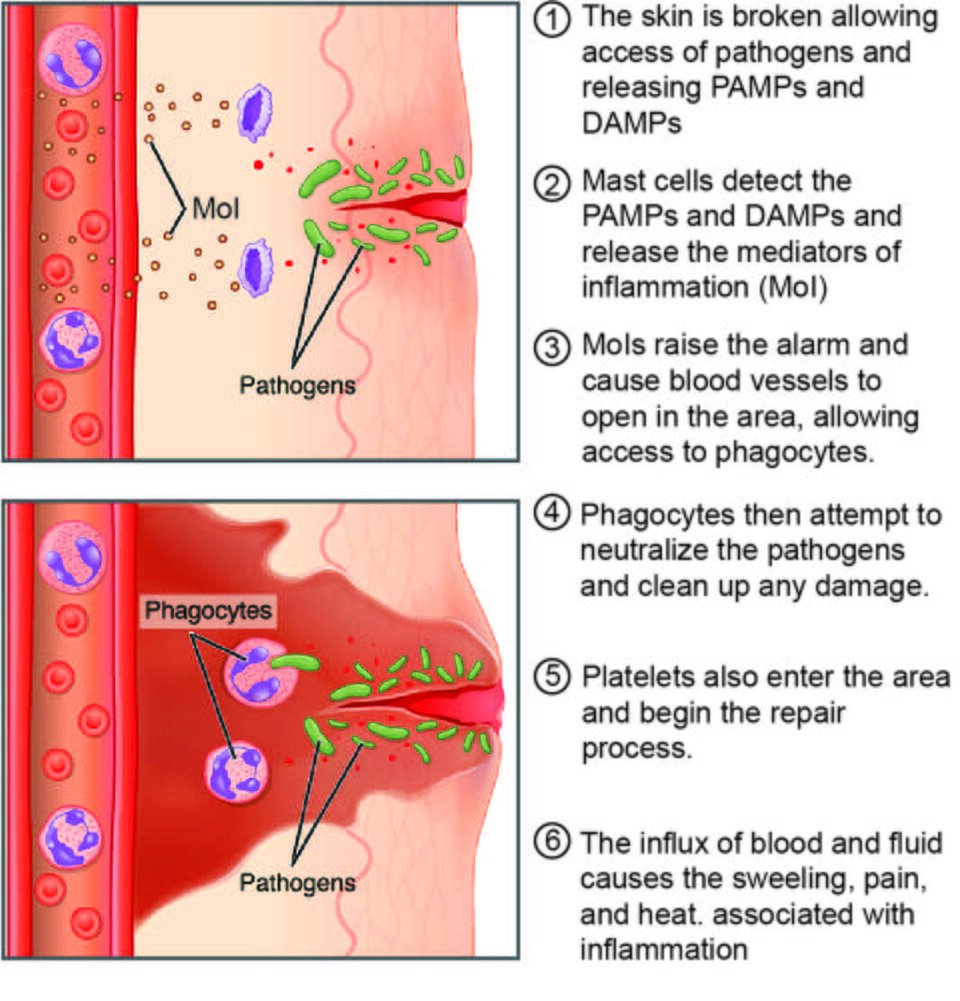
This reaction also brings in the cells of the innate immune system, allowing them to get rid of the sources of a possible infection. Inflammation is part of a very basic form of immune response. The process not only brings fluid and cells into the site to destroy the pathogen and remove it and debris from the site, but also helps to isolate the site, limiting the spread of the pathogen.
Acute inflammation is a short-term inflammatory response. If the cause of the inflammation is not resolved, however, it can lead to chronic inflammation, which is associated with major tissue destruction and fibrosis. Chronic inflammation is ongoing inflammation. It can be caused by foreign bodies, persistent pathogens, and autoimmune diseases such as rheumatoid arthritis.
There are four important parts to the inflammatory response: tissue injury, vasodilation, increased vessel permeability, and recruitment of phagocytes.
Tissue Injury
The released contents of injured cells stimulate the release of mast cell granules and their potent inflammatory chemicals such as histamine, leukotrienes, and prostaglandins. Histamine increases the diameter of local blood vessels (vasodilation), causing an increase in blood flow to the damaged area. Histamine also increases the permeability of local capillaries, causing plasma to leak out and form interstitial fluid. This causes the swelling associated with inflammation.
Additionally, injured cells, phagocytes, and basophils are sources of inflammatory chemicals, including prostaglandins and leukotrienes. Leukotrienes attract neutrophils from the blood and increase vessel permeability. Prostaglandins cause vasodilation and are a major cause of the pain associated with inflammation. Nonsteroidal anti-inflammatory drugs such as aspirin and ibuprofen relieve pain by inhibiting prostaglandin production.
Vasodilation
Many inflammatory chemicals such as histamine are vasodilators that increase the diameters of local capillaries. This causes increased blood flow to the area and is responsible for the heat and redness of inflamed tissue. It allows greater access of the blood to the site of inflammation.
Increased Vessel Permeability
At the same time, inflammatory chemicals increase the permeability of the local vessels, causing leakage of fluid into the interstitial space, resulting in the swelling, or edema, associated with inflammation.
Recruitment of Phagocytes
Any type of invasion or tissue injury attracts neutrophils from the blood to the site of infection. Neutrophils are the first responders, and then macrophages are recruited to clean up the debris left over at the site. When local infections are severe, neutrophils are attracted to the sites of infections in large numbers, and as they phagocytize the pathogens and subsequently die, their accumulated cellular remains are visible as pus at the infection site.
Inflammation is valuable for many reasons. Not only are the pathogens killed and debris removed, but also the increase in vessel permeability encourages the entry of clotting factors, the first step towards wound repair. Inflammation also facilitates the transport of antigens to lymph nodes for the development of the adaptive immune response.
View a supplementary YouTube video[5] on the inflammatory response: The Inflammatory Response HD Animation.
Specific (Adaptive) Immune Response
The slower but more effective specific or adaptive immune response is primarily controlled by lymphocytes, which help control immune responses. There are two main groups of lymphocytes called B cells and T cells, both of which are formed in bone marrow. B cells are involved in humoral immunity, and T cells are involved in cell-mediated defenses. See Figure 12.11[6] for an overview of the specific immune response.
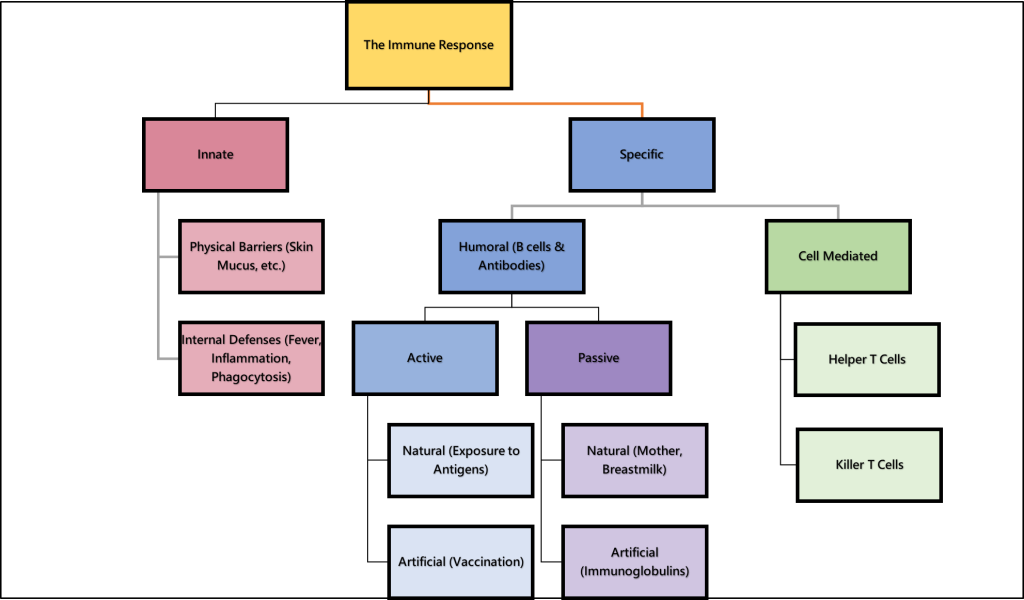
Humoral Immunity (B cells and Antibodies)[7]
Humoral immunity refers to the function of B cells and their production of antibodies. B cells originate and develop in the bone marrow and then migrate in body fluids through the lymph nodes, spleen, and blood to seek out and destroy pathogens in the interstitial spaces. B cells make Y-shaped proteins called antibodies that destroy pathogens based on their antigens. Antigens are markers that tell the immune system whether something in the body is harmful or not. Antigens are found on viruses, bacteria, cancer cells, and even normal cells of the body. Each antigen has a unique shape that the immune system reads like a name tag to know whether or not it belongs in that person’s body. Antibodies are very specific to the antigens they recognize and destroy. They fit onto the antigen like a key to a lock.
When a B cell finds an abnormal cell with an antigen that it has antibodies for, it binds to it and responds by cloning itself into many B cells and also releases thousands of antibodies per second to attack the pathogen. Some B cells become memory B cells that are involved in immunological memory to ensure a stronger and faster antibody response if the body is exposed to the same antigen in the future.
Cell-Mediated Response (T cells)
When innate immunity and humoral immunity are not effective in defending against pathogens or abnormal cells, the cell-mediated response uses lymphocytes called T cells to destroy the abnormal cells. There are two major types of T cells called helper T cells and cytotoxic T cells:
- Helper T (CD4) cells use chemical messengers to activate the specific immune response. They stimulate B cells to make antibodies and help activate the cytotoxic T cells.
- Cytotoxic T (CD8) cells directly kill cells that have been invaded by a virus or are otherwise abnormal.
During a primary specific immune response, both memory T cells and effector T cells are generated. Memory T cells are long-lived and can even persist for a lifetime. Memory cells act rapidly so any subsequent exposure to the pathogen will elicit a very rapid T cell response. This rapid response generates large numbers of effector T cells so fast that the pathogen is often overwhelmed before it can cause any symptoms of disease. This is what is meant by immunity to a disease.
Active Versus Passive Immunity[8]
Immunity to pathogens and the ability to control pathogen growth so that tissue damage is limited can be acquired by (1) the active development of an immune response in the infected individual or (2) the passive transfer of immune components from an immune individual to a nonimmune one. Both active and passive immunity have examples in the natural world and as part of medicine.
Active immunity is the resistance to pathogens acquired during an adaptive immune response within an individual. Active immunity can be acquired naturally through exposure to a pathogen or artificially through the use of vaccines. A vaccine contains a killed or weakened pathogen or its components. When administered to a healthy individual, it causes a weakened primary immune response and the development of immunological memory. With administration of vaccines, one can avoid the damage from disease that results from exposure to a pathogen yet reap the benefits of protection from immunological memory. The advent of vaccines was one of the major medical advances of the twentieth century and led to the eradication of smallpox and the control of many infectious diseases, including polio, measles, and whooping cough.
Passive immunity arises from the transfer of antibodies to an individual without mounting their own active immune response. Naturally acquired passive immunity is seen during fetal development when antibodies are transferred from the maternal circulation to the fetus via the placenta, thus protecting the fetus from infection and protecting the newborn for the first few months of its life. A newborn also benefits from antibodies it obtains from its mother’s milk during breastfeeding. Therefore, the fetus and newborn benefit from the immunological memory based on the pathogens to which the pregnant mother has been exposed.
Artificially acquired passive immunity typically involves injections of immunoglobulins taken from donated human blood previously exposed to a specific pathogen. This treatment is a fast-acting method of temporarily protecting an individual who had a possible exposure to a pathogen or has an immunodeficiency disease and is not capable of creating their own antibodies. The downside to both types of passive immunity is the lack of the development of immunological memory. Once the antibodies are transferred, they are effective for only a limited time before they degrade.
See Table 12.4c for a summary of natural and artificial active and passive immunity.
Table 12.4c. Active Versus Passive Immunity[9]
| Natural | Artificial | |
|---|---|---|
| Active | Adaptive immune response | Vaccine response |
| Passive | Transplacental antibodies and breastfeeding | Immune globulin injections |
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2213_Inflammatory_Process” by OpenStax College is licensed under CC BY 3.0 ↵
- Abdulaziz, A. (2014, September 23). The inflammatory response HD animation [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=fcAAnj4czzo ↵
- “Immune_Response 2” by Open RN is licensed under CC BY-NC 4.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Health alterations. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthalts/ ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
A type of endocytosis where the cell engulfs large particles or microorganisms ("cell eating"), commonly performed by immune cells like macrophages.
A phagocytic cell in the bone marrow, liver, and spleen that removes worn-out red blood cells from circulation.
A type of granular white blood cell that makes up 50–70% of leukocytes and is essential for fighting bacterial infections.
A circulating cell that differentiates into either a macrophage or dendritic cell, which can be rapidly attracted to areas of infection.
A rapid immune response to injury or infection characterized by redness, heat, swelling, pain, and loss of function.
Ongoing inflammation caused by foreign bodies, persistent pathogens, and autoimmune diseases such as rheumatoid arthritis.
A chemical released during inflammation that causes vasodilation and increased capillary permeability, leading to swelling and redness at the injury site.
The body’s targeted defense against specific pathogens, involving activation of lymphocytes (B and T cells) that recognize and remember particular antigens.
Immunity involving B cells that produce antibodies to target and neutralize pathogens.
Proteins produced by B cells that specifically recognize and bind to foreign antigens to help neutralize or destroy them.
Substances that may trigger a defensive response from leukocytes of the immune system if the body does not recognize the antigen as belonging to "self."
An immune response that involves T cells attacking infected or abnormal body cells directly, without using antibodies.
Immunity developed when the body produces its own antibodies after exposure to a pathogen or vaccination.
Immunity gained by receiving antibodies from another source, providing temporary protection without the body producing its own antibodies.

