11.6 Cardiovascular Disorders
Cardiovascular Disorders
Aneurysm
An aneurysm is a weakened blood vessel wall that bulges or balloons. An aneurysm can break open, which is called a rupture. A ruptured aneurysm causes severe internal bleeding and be life threatening. Some aneurysms cause no symptoms. Aneurysms can form in several parts of the body, including the following[1]:
- The body’s main artery, called the aorta (aortic aneurysm)
- The part of the aorta that passes through the abdominal area (abdominal aortic aneurysm)
- The part of the aorta that passes through the chest (thoracic aortic aneurysm)
- Blood vessels that send blood to the brain (brain aneurysm)
- Blood vessels in other parts of the body, such as the legs, groin, or neck (peripheral aneurysm)
Depending on the location, small aneurysms with low risk of rupture may be monitored with regular health checkups and imaging tests. Treatment of aneurysms may involve open surgery, or a less-invasive treatment called endovascular surgery. However, if an aneurysm ruptures, life-threatening hemorrhage can occur requiring emergency surgery for survival.[2]
Arrhythmias[3],[4]
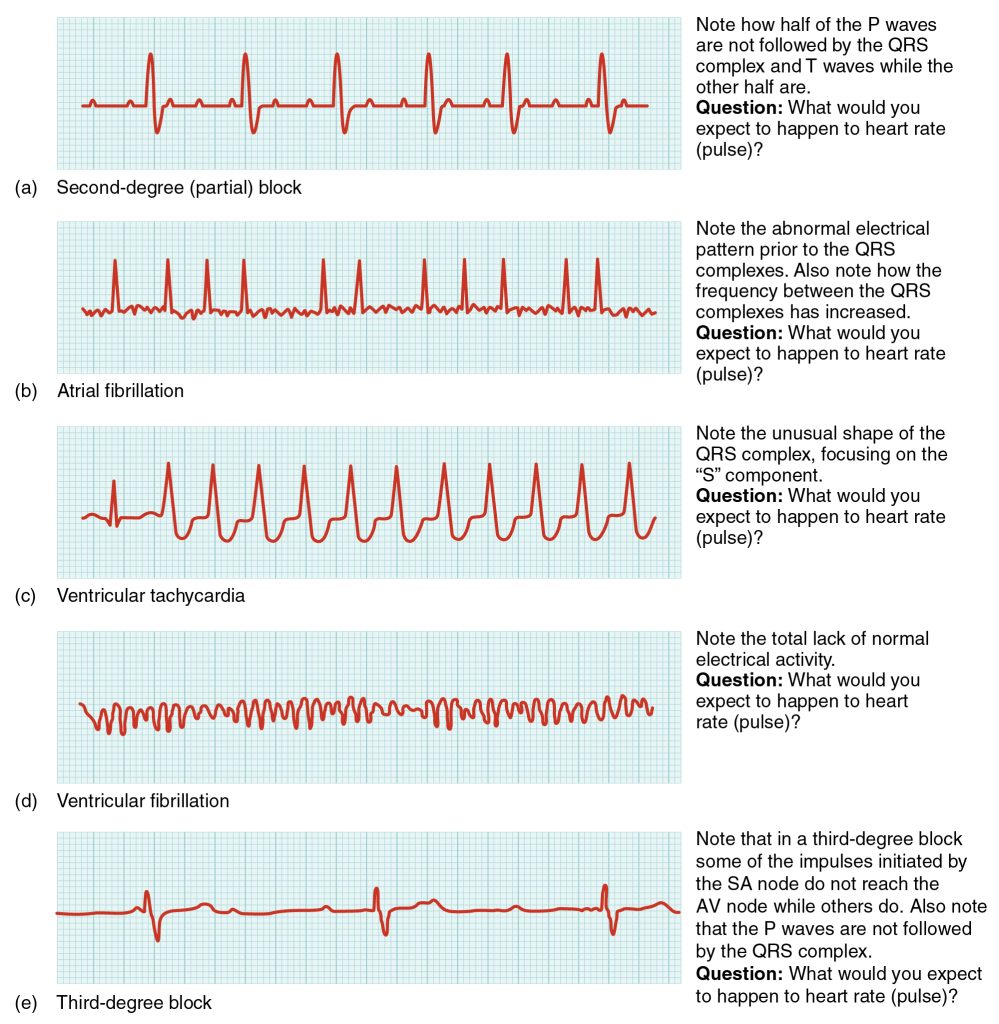
An arrhythmia is an abnormal heart rhythm due to disrupted electrical activity of the conduction system. Arrhythmias can be diagnosed by electrocardiogram or the use of a Holter monitor. Examples of common arrhythmias are atrial fibrillation, heart block, ventricular tachycardia, and ventricular fibrillation.
- Atrial fibrillation (A-Fib) is characterized by atrial quivering instead of contracting. Atrial fibrillation can cause a decrease in the volume of blood leaving the heart with each heartbeat because the ventricles do not completely fill with blood before contracting. Individuals with atrial fibrillation may be asymptomatic or have palpitations, decreased blood pressure, or shortness of breath. Atrial fibrillation also increases the risk of a cerebrovascular accident (stroke).
- Heart block refers to a disruption in the normal conduction pathway of electrical signals through the atria and ventricles. Heart block can vary in severity from first-degree heart block, which is the least severe and often has no symptoms, to third-degree heart block that can be life-threatening. Symptoms of heart block may include bradycardia, missed heart beats, fatigue, dizziness, chest pain, and shortness of breath.
- Ventricular tachycardia (V Tach) refers to a very rapid heartbeat that originates in the ventricles. Ventricular fibrillation (V Fib) is a disorganized heart rhythm that causes the ventricles to quiver instead of contract. Ventricular tachycardia and ventricular fibrillation are life-threatening arrhythmias that require rapid emergency response and the use of a defibrillator to resolve the abnormal rhythm.
See Figure 11.55[5] for EKG tracings of common arrhythmias.
Arteriosclerosis and Atherosclerosis
Arteriosclerosis and atherosclerosis are interrelated cardiovascular conditions that can significantly impact a person’s cardiovascular health. Arteriosclerosis refers to the thickening and stiffening of arterial walls that is commonly associated with normal aging. The subsequent loss of elasticity of blood vessels makes them less responsive to changes in blood flow and can reduce blood flow to organs and tissues within the body.[6]
Atherosclerosis is a condition where cholesterol, low-density lipoprotein (LDL) deposits, and wastes build up within the lining of the arteries. It begins after injury to the endothelium (inner lining) of an artery, often caused by tobacco use, hypertension, high blood glucose levels, infection, excessive blood lipids, or other factors. Artery walls that are constantly stressed by blood flowing at high pressure are more likely to be injured. This buildup of substances within the vessel walls, called plaque, creates inflammation and can cause blockage of the artery[7]
Atherosclerosis of the coronary arteries leads to coronary artery disease. See Figure 11.56[8] for an illustration of atherosclerosis.
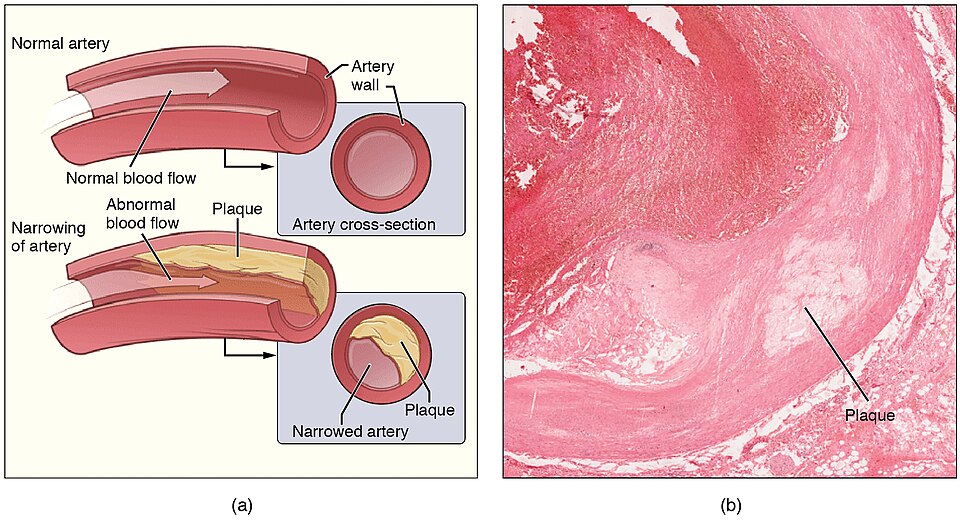
While the two conditions are interrelated, one can occur without the other. For instance, someone may have arteriosclerosis but not have atherosclerosis. However, atherosclerosis is a specific type of arteriosclerosis, meaning that if atherosclerosis is present, there is also thickening and stiffening of arterial walls in addition to the build-up of plaque.[9]
Broken Heart Syndrome
Extreme stress from life events such as the death of a loved one, break up of a relationship, loss of a job, or foreclosure of a home can lead to a condition commonly referred to as broken heart syndrome, also known as Takotsubo cardiomyopathy, transient apical ballooning syndrome, apical ballooning cardiomyopathy, stress-induced cardiomyopathy, and Gebrochenes-Herz syndrome.
The effects on the heart include profound weakening of the myocardium that can lead to lethal arrhythmias, acute heart failure, or rupture of a ventricle. The exact cause of this syndrome is not known, but several factors have been suggested, including transient vasospasm, dysfunction of the cardiac capillaries, or thickening of the myocardium—particularly in the left ventricle—that may lead to lack of critical circulation of blood to this region.
With treatment to restore normal function, many patients survive the initial acute event, but there is a strong correlation with death. Research revealed that within one year of the death of a loved one, women are more than twice as likely to die and men are six times as likely to die than would otherwise be expected. The same study indicated that long-term relationships had a greater incidence of a person dying soon after the death of their spouse.[10]
Cardiac Tamponade
If excess fluid builds up within the pericardial space, it can lead to a condition called cardiac tamponade, also called pericardial tamponade. With each contraction of the heart, more fluid accumulates within the pericardial cavity. To fill with blood for the next contraction, the heart must relax. However, the excess fluid in the pericardial cavity puts pressure on the heart and prevents full relaxation, so the chambers within the heart contain less blood as they begin each heart cycle. Over time, less and less blood is ejected from the heart.
If the fluid builds up slowly, the pericardial cavity may be able to expand gradually to accommodate this extra volume. However, rapid accumulation of as little as 100 mL of fluid following trauma may trigger cardiac tamponade. Common causes of cardiac tamponade include pericarditis, cancer, and cardiac surgery. Usually, a needle is inserted into the pericardial cavity to remove the excess fluid. If left untreated, cardiac tamponade can be fatal.[11]
Congenital Heart Defects
Congenital heart defects are structural abnormalities in the heart or blood vessels that are present at birth and affect how blood flows through the heart and out to the rest of the body. Heart defects can vary from mild (such as a small hole in the heart) to severe (such as missing parts of the heart). In the United States, heart defects affect 1% of births annually, or about 40,000 infants. Of those infants born with a heart defect, about 25% have a severe heart defect requiring surgery or other procedures in the first year of life.[12] Common congenital heart defects are illustrated in Figure 11.57.[13] These conditions are further described in the following subsections.
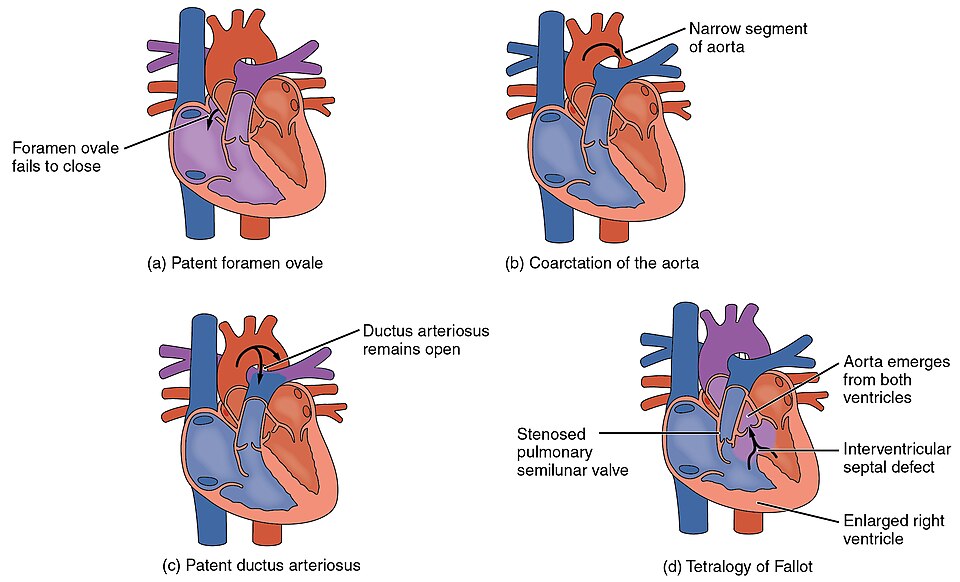
Patent Foramen Ovale and Atrial Septal Defect
Patent foramen ovale (PFO) is a common congenital heart defect that occurs when the fossa ovalis in the interatrial septum that is present during fetal circulation does not fuse after birth. The word patent is from the Latin root patens, meaning “open.” PFO allows oxygenated blood to flow backwards from the left atrium into the right atrium. Small PFOs are typically asymptomatic. As many as 15-25% adults have PFOs that are found incidentally on diagnostic tests for other conditions or on autopsy.[14]
An atrial septal defect (ASD) is an abnormal opening between the atria. ASDs and PFOs are typically detected by auscultation of a heart murmur (a blowing or whooshing sound that signifies turbulent blood flow). The diagnosis is confirmed through diagnostic imaging with an echocardiogram. Benign (asymptomatic) defects are generally monitored while symptomatic defects affecting oxygenation status typically require surgical repair.[15]
Coarctation of the Aorta
Coarctation of the aorta is a congenital abnormal narrowing of the aorta that is normally located at the insertion of the ligamentum arteriosum, the remnant of the fetal shunt called the ductus arteriosus. If severe, this condition drastically restricts blood flow through the aorta and is life-threatening. In some individuals, the condition may be fairly benign and not detected until later in life. Detectable symptoms in an infant include difficulty breathing, poor appetite, trouble feeding, and poor weight gain. In older individuals, symptoms include dizziness, fainting, shortness of breath, chest pain, fatigue, headache, and nosebleeds. Treatment involves surgery to resect (remove) the narrowed region or angioplasty to open the abnormally narrow passageway. Studies have shown that the earlier the surgery is performed, the better the chance of survival.[16]
Patent Ductus Arteriosus
Patent ductus arteriosus (PDA) is a congenital condition in which the ductus arteriosus fails to close at birth. Recall that the ductus arteriosus is a normal shunt in fetal circulation to connect the pulmonary trunk to the aorta, causing most of the circulating oxygenated blood to bypass the fetal lungs. As the newborn takes its first breaths and the lungs expand, the vascular resistance and lung pressure abruptly decrease, normally causing the ductus arteriosus to constrict and close. However, when a PDA is present, the opening continues to exist between the aorta and the pulmonary trunk, causing oxygen-rich blood from the aorta to flow backwards into the pulmonary trunk. This additional fluid moving toward the lungs increases pulmonary pressure and can impact respiration. Small PDAs often close on their own and are asymptomatic. Larger PDAs are often symptomatic and require treatment. Symptoms may include dyspnea (shortness of breath), tachycardia (fast heart rate), enlarged heart, and poor weight gain in infants. Treatments include surgical closure (ligation), manual closure using platinum coils or specialized mesh inserted via the femoral artery or vein, or nonsteroidal anti-inflammatory drugs to block the synthesis of prostaglandin E2, which maintains the vessel in an open position. If untreated, the condition can result in pulmonary congestion and heart failure.[17],[18]
Tetralogy of Fallot
Tetralogy of Fallot (ToF) is a complex set of congenital heart defects that occurs in approximately 400 out of one million live births. The term tetralogy is derived from the four components associated with the condition, although only three may be present to be diagnosed with the disorder. The four components include pulmonary stenosis (rigidity or stenosis of the pulmonary valve), a large ventricular septal defect (opening between the ventricles), an overriding aorta (the aorta is shifted above both ventricles and centered over the ventricular septal defect), and right ventricular hypertrophy (enlargement of the right ventricle). The components of ToF cause multiple effects. Pulmonary stenosis makes it difficult for blood to flow from the right ventricle into the lungs, causing increased pressure inside the right ventricle. This causes the right ventricle to work harder to pump blood, causing right ventricular hypertrophy that can lead to heart failure. It also causes deoxygenated blood from the right ventricle to move through the ventricular septal defect into the left ventricle. Because the aorta is located between the ventricles and over the ventricular septal defect, oxygenated blood from the left atrium mixes with deoxygenated blood from the right ventricle, and this partially oxygenated blood moves through the aorta and to the rest of the body, causing hypoxia and cyanosis.[19],[20]
Symptoms include a distinct heart murmur; low blood oxygen percent saturation; dyspnea or difficulty in breathing; polycythemia; broadening (clubbing) of the fingers and toes; and in children, difficulty in feeding or failure to grow and develop. It is the most common cause of cyanosis following birth. A pulse oximetry screening tool is routinely used in hospitals after birth to detect signs of critical congenital heart defects (CCHD) such as ToF. During this screening test, pulse oximetry is performed at 24 hours of age on the right hand (preductal) and either foot (postductal). If both readings are greater or equal to 95% and there is no more than a 3% difference between the two readings, the infant is at less risk for ToF. ToF is diagnosed by echocardiography (ultrasound of the heart).[21],[22]
Treatment involves extensive surgical repair, including the use of stents to redirect blood flow, replacement of valves, and patches to repair the septal defect. Surgical repair results in excellent long-term survival in the United States, with over 90% survival rates for individuals 25 years after repair. However, heart failure and arrhythmias are common long-term consequences that can lead to death.[23]
Blue Baby
Cyanotic heart defects such as Tetralogy of Fallot involve right to left shunting of blood through the heart, which causes deoxygenated blood from the venous system to bypass transport to the lungs and is pumped through the aorta to the arterial system. Recall that in a normal heart, blood flows from the right ventricle to the lungs where it is oxygenated and then returns back to the left atrium and left ventricle where it is pumped through the aorta to the rest of the body. When a cyanotic defect is present, poorly oxygenated blood is pumped to the body, causing decreased blood oxygen saturation levels, organ and tissue hypoxia, and cyanosis. Because the blood bypasses the lungs, oxygen administration does little to improve oxygen saturation levels. Cyanosis manifests as a bluish color to the lips, fingers, and toes of an infant or child and may occur at rest or with activity, depending on the severity of the heart defect. As such, the term “blue baby” has been used to describe children with cyanotic heart defects.[24],[25]
Coronary Artery Disease
Coronary artery disease (CAD) is the leading cause of death worldwide. It occurs when the buildup of plaque, a fatty material including cholesterol, connective tissue, white blood cells, and smooth muscle cells, obstructs blood flow within coronary arteries and decreases compliance of the vessels. This condition is called atherosclerosis. As the coronary blood vessels become occluded, the flow of oxygenated blood is restricted, resulting in the cardiac muscle cells receiving insufficient oxygen, a condition called ischemia. Some individuals with coronary artery disease report the development of chest pain on exertion called angina pectoris. If left untreated, coronary artery disease can cause a myocardial infarction (heart attack), resulting in the death of cardiac cells that can seriously impair heart function. See Figure 11.58[26] for an image of blockages of coronary arteries highlighted by the injection of dye.
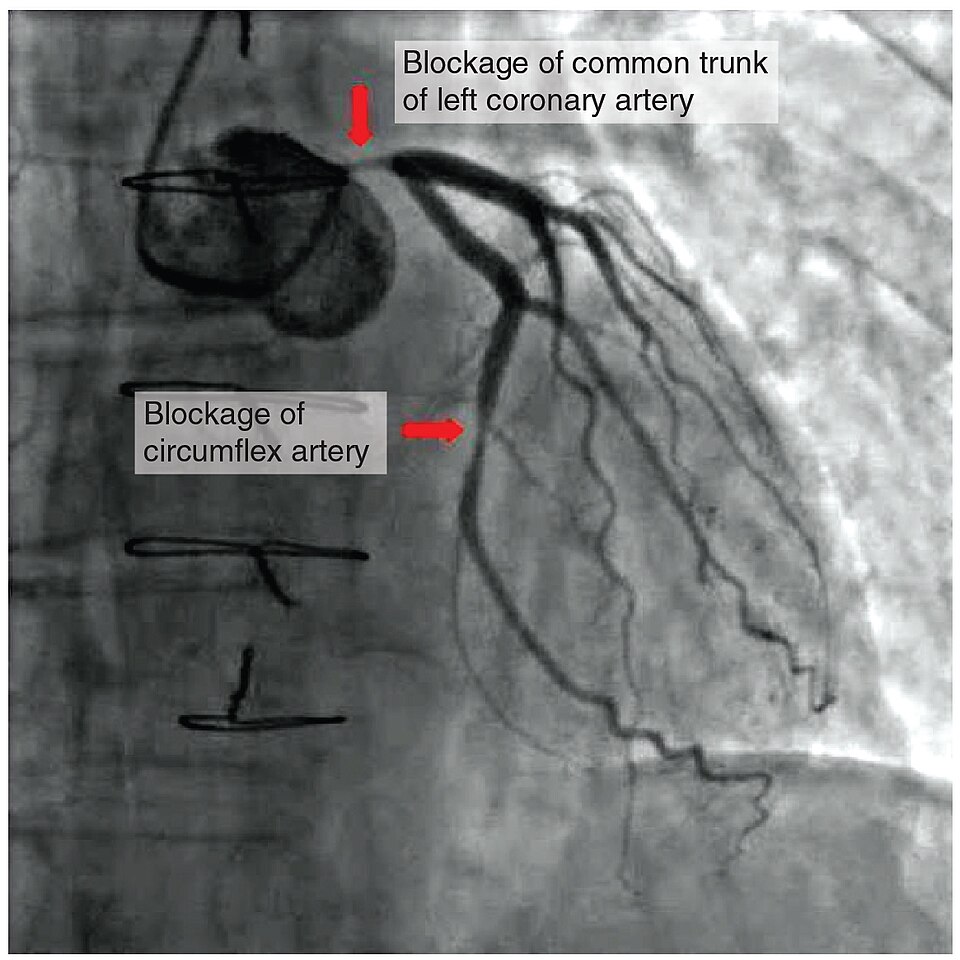
Coronary artery disease develops slowly as fatty “streaks” in the vessels gradually progress throughout life. Risk factors include family history, smoking, hypertension, obesity, diabetes, alcohol consumption, lack of exercise, stress, and hyperlipidemia (high circulating levels of lipids in the blood). Early treatment often begins with lifestyle changes such as making healthy diet choices; stopping smoking, engaging in regular exercise; and taking medications to reduce blood pressure, blood glucose, and lipid levels.[27]
Surgical treatment of coronary artery disease includes angioplasty and insertion of a stent, or coronary artery bypass graft surgery. Angioplasty is a procedure in which the occlusion caused by plaque is mechanically widened with a balloon. A specialized catheter with an expandable tip is inserted into a vessel, in the leg or arm, and then directed to the site of the occlusion where the balloon is inflated to compress the plaque and open the vessel to increase blood flow. A stent consisting of a specialized mesh is typically inserted at the site of occlusion to reinforce the weakened and damaged walls. Coronary artery bypass graft (CABG) surgery uses a replacement vessel to bypass the occluded area.[28]
Edema
Despite the presence of valves in veins, some blood will inevitably pool in the lower limbs over the course of a day due to the pull of gravity. Blood that accumulates in a vein will increase the pressure within it, which is reflected back into the smaller veins, venules, and eventually even the capillaries. Increased pressure promotes the flow of fluids out of the capillaries and into the interstitial fluid. The presence of excess tissue fluid around the cells leads to a condition called edema.[29]
Most people experience a daily accumulation of tissue fluid, especially if they spend much of their work life on their feet (such as health professionals). However, edema goes beyond normal swelling and requires medical treatment. Edema has many potential causes, such as heart failure, kidney failure, and severe protein deficiency. Edema is commonly managed with compression stockings and medications called diuretics that cause the kidneys to excrete additional salt and fluid.[30]
Heart Failure[31]
Heart failure (HF) occurs when the heart loses its effectiveness in pumping blood and is referred to as decreased cardiac output. When the heart is not pumping effectively, classic symptoms of fatigue, shortness of breath, edema, or lung congestion can occur. Signs and symptoms can also vary based on whether the right or left side of the heart is affected.
There are many common causes of HF, including coronary artery disease, myocardial infarction (MI), hypertension, valve disorders, and cardiomyopathy. Common tests used to diagnose heart failure include brain natriuretic peptide (BNP), chest X-ray (CXR), echocardiogram, and electrocardiogram (ECG).
Common medical interventions used to treat HF include medication therapy, lifestyle modifications, cardiac rehabilitation, and surgical interventions.
Hypertension
Normal blood pressure in an adult is defined as less than 120/80 mm Hg. Hypertension refers to chronically elevated blood pressure greater than 120/80 mm Hg. Hypertension is very common, affecting millions of individuals worldwide. There are several classifications of blood pressure based on the systolic and diastolic readings. See Table 11.6 for current classifications of hypertension according to the American Heart Association.[32],[33]
Table 11.6. Classifications of Hypertension
| Blood Pressure Classification | Systolic (mm Hg) |
Diastolic (mm Hg) |
|---|---|---|
| Normal | Less than 120 | Less than 80 |
| Elevated (Prehypertension | 120-129 | Less than 80 |
| Hypertension Stage 1 | 130-139 | 80-89 |
| Hypertension Stage 2 | 140 or higher | 90 or higher |
| Hypertension Stage 3 | Higher than 180 | Higher than 120 |
Primary hypertension is the most common type of hypertension and has no identifiable cause. It typically develops gradually over time and is influenced by various risk factors such as genetics, age, race, diet, lifestyle, and stress. Hypertension is typically a silent disorder, meaning many individuals with hypertension have no symptoms and are unaware of the condition until they have an elevated blood pressure reading. Untreated hypertension can lead to significant health complications such as myocardial infarction (heart attack), heart failure, cerebrovascular accident (stroke), vision loss, and kidney damage.[34]
Lifestyle changes are often the first step in hypertension management and can be effective in lowering blood pressure. Recommendations include a heart-healthy, low-salt diet; regular physical activity; weight loss; and smoking cessation. Antihypertensive medications are prescribed to control blood pressure if lifestyle modifications alone are insufficient.[35],[36]
Heart Valve Disorders[37]
If heart valves do not function properly, they can result in valvular heart disease that can range from asymptomatic to life-threatening. Valvular heart disease can be congenital, meaning the individual was born with the defect, whereas others may be attributed to disease processes or trauma. Valvular disorders are often caused by carditis (inflammation of the heart) that is commonly triggered by rheumatic fever. Rheumatic fever is an autoimmune response to an untreated bacterial infection with Streptococcus pyogenes, the organism that causes a condition commonly called “strep throat.”
When a valve malfunctions, the flow of blood is disrupted and often described as insufficiency. The specific type of insufficiency is named for the valve involved: aortic insufficiency, mitral insufficiency, tricuspid insufficiency, or pulmonary insufficiency.
If one of the cusps of the valve is forced backward by the force of the blood, the condition is referred to as a prolapsed valve. Prolapse may occur if the chordae tendineae are damaged or broken, causing the closure mechanism to fail.
The failure of the valve to close properly disrupts the normal one-way flow of blood and results in regurgitation, when the blood flows backward from its normal path. The disrupted flow of blood produces a heart murmur that can be heard on auscultation with a stethoscope. Mitral regurgitation is the most common valve disorder, detected in approximately 2 percent of the population.
Valvular stenosis is a condition in which the heart valves become rigid and may calcify over time. The loss of flexibility of the valve interferes with normal function and may cause the heart to work harder to propel blood through the valve, which eventually weakens the heart. Aortic stenosis affects approximately 2 percent of the population over 65 years of age, and the percentage increases to approximately 4 percent in individuals over 85 years.
If a heart valve disorder is suspected, an echocardiogram is performed for diagnosis of the disorder. Treatment for heart valve disorders can range from lifestyle changes and medications to surgical repair or replacement, depending on the severity and type of valve disease.
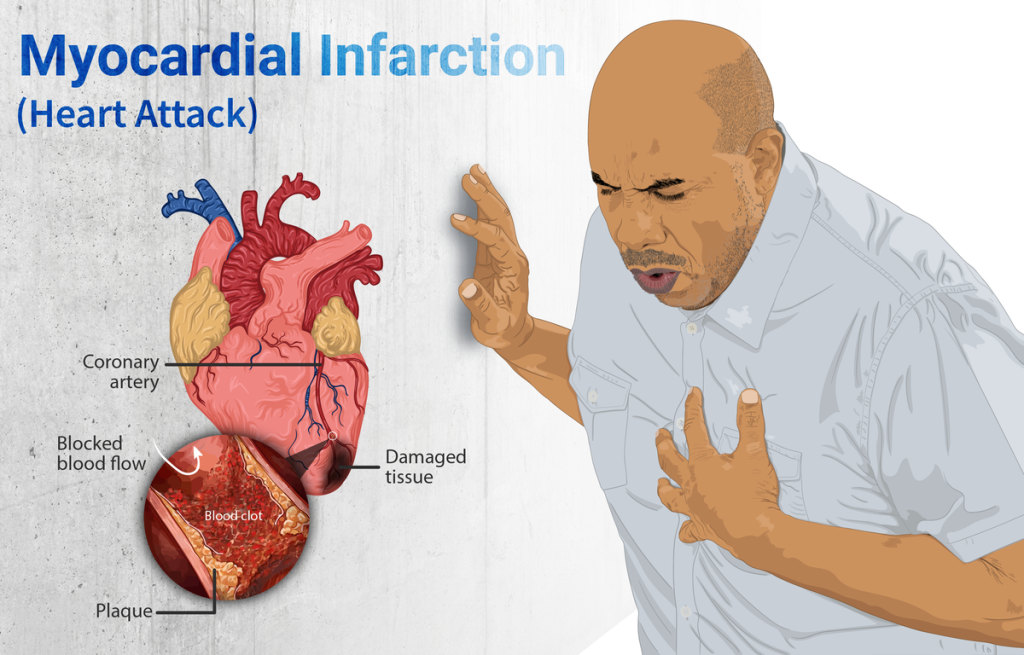
Myocardial Infarction
Myocardial infarction (MI) is the medical term for what is commonly known as a heart attack. An MI results from a lack of oxygenated blood flow (ischemia) to a region of the heart myocardium, resulting in death of the cardiac muscle cells. An MI often occurs when a coronary artery is blocked by the buildup of atherosclerotic plaque that consists of lipids, cholesterol and fatty acids, and white blood cells. An MI can also occur when a piece of an unstable atherosclerotic plaque travels through the coronary arterial system and lodges in one of the smaller vessels. The resulting blockage restricts the flow of blood and oxygen to the myocardium and causes death of the tissue.[38]
Modifiable risk factors for MI include high blood pressure; high cholesterol; smoking; obesity; physical inactivity; and diets high in saturated fats, trans fats, sodium, and refined sugars. Chronic stress and excessive alcohol consumption can also play a role in the development of coronary artery disease. There are also numerous nonmodifiable risk factors for coronary artery disease. The risk of coronary artery disease increases with age; men over the age of 45 and women over the age of 55 are at higher risk. Family history and genetics are also nonmodifiable risk factors, especially if a patient has a first-degree relative who has been diagnosed with coronary artery disease or had a myocardial infarction at a young age. Specific ethnic groups, such as African Americans are also at higher risk for the development of cardiovascular disease.[39],[40]
During an MI, the individual may experience sudden pain deep to the sternum (retrosternal pain) called angina pectoris, often radiating down the left arm or into the jaw. Additional symptoms of MI may include dyspnea (shortness of breath), palpitations (irregular heartbeat), diaphoresis (sweating), nausea and vomiting, anxiety, and fainting (syncope). However, females may not have these classic symptoms but simply experience vague symptoms of fatigue, indigestion, and anxiety. Until this anomaly between the sexes was discovered, many female patients suffering MIs were misdiagnosed with indigestion and sent home from the emergency room without treatment.[41] See Figure 11.59[42] for an illustration of the symptoms of an MI.
Immediate emergency treatment for MI is essential and includes aspirin to reduce clot formation, nitroglycerin to dilate the coronary arteries and improve blood flow to the heart tissue, and administration of supplementary oxygen as indicated. Intravenous heparin is typically administered to prevent the clot from enlarging. Emergent revascularization procedures, such as angioplasty, stenting, or coronary artery bypass graft (CABG) surgery, are typically performed if vessel occlusion is significant. If revascularization procedures cannot be performed within a few hours, thrombolytic agents may be administered to dissolve the clot.[43],[44] Read more about these procedures under the “Coronary Artery Disease” subsection.
Pericarditis
Pericarditis is swelling and irritation of the pericardium, the thin, saclike tissue surrounding the heart. Pericarditis often causes sharp, stabbing chest pain when the irritated layers of the pericardium rub against each other. The pain often worsens when breathing deeply or lying down but improves when sitting up or leaning forward. Pericarditis is typically caused by a viral infection but is also associated with autoimmune disorders such as rheumatoid arthritis or lupus. Pericarditis often resolves on its own with rest, but treatment may be required for severe cases to prevent complications such as pericardial effusion that can lead to cardiac tamponade.[45]
Peripheral Artery Disease[46]
Peripheral artery disease (PAD) is caused by atherosclerosis, with narrowed or blocked arteries, causing reduced oxygenated blood flow to the lower extremities. Risk factors for peripheral artery disease are similar to atherosclerosis and include smoking, hypertension, high cholesterol, and inflammation. Additional risk factors include age and a history of diabetes or previous injuries or trauma to arterial vessels.
See Figure 11.60[47] for an illustration of PAD.
Peripheral artery disease can cause non-healing wounds in the lower extremities, which can become infected and lead to foot or leg amputation. Peripheral artery disease also increases the risk for myocardial infarction and stroke.
The most common symptom of peripheral artery disease is painful muscle cramping in the hips, thighs, or calves when walking, climbing stairs, or exercising called intermittent claudication. This pain typically resolves when the activity is stopped, although it may take a few minutes. Other symptoms may include muscle wasting or atrophy, reduced or absent pulses, prolonged capillary refill time, changes in skin color, hair loss, and sensations of numbness or tingling.
Health care providers may use a combination of noninvasive and invasive tests to evaluate blood flow and identify blockages in the arteries of the limbs. Treatment of peripheral artery disease consists of lifestyle modifications, medication therapy, and surgical management.
Shock
Shock is a life-threatening condition where the body’s tissues and organs don’t receive enough blood and oxygen. This inadequate blood flow leads to cellular dysfunction and can result in organ damage and failure if not treated promptly. It should not be confused with emotional or psychological shock.[48]
Shock is generally classified into four categories called hypovolemic, cardiogenic, distributive, and obstructive[49]:
- Hypovolemic shock can be caused by hemorrhage or significant fluid losses, often related to severe vomiting or diarrhea or extensive burns. Typically, patients with hypovolemic shock have decreased blood pressure; a rapid heart rate; a weak pulse often described as “thready;” cool, clammy skin in the extremities due to restricted peripheral blood flow; rapid, shallow breathing; thirst; and dry mouth. Treatments involve treating the cause and providing intravenous fluids.[50]
- Cardiogenic shock results from the inability of the heart to adequately pump and maintain cardiac output. It is often caused by myocardial infarction (heart attack) but may also be caused by arrhythmias, valve disorders, cardiomyopathies, and heart failure. Treatment focuses on restoring the heart’s pumping ability and supporting blood flow until the underlying cause can be resolved. This often involves medications, mechanical circulatory support devices, and potentially surgery.[51]
- Distributive shock characterized by peripheral vasodilation and includes conditions such as septic shock, anaphylactic shock, neurogenic shock (caused by trauma to the cranium or spinal cord that damages the cardiovascular centers in the medulla oblongata or the nerve fibers originating from this region), and endocrine and metabolic shock (caused by adrenal failure, severe hypothyroidism called myxedema, diabetic ketoacidosis, other severe acid-base imbalances, and severe electrolyte imbalances). Treatment includes administration of intravenous fluids and medications to maintain adequate blood pressure to organs.
- Obstructive shock is caused by extracardiac conditions leading to a decrease in the left ventricular cardiac output and decreased delivery of oxygen to tissues. Causes include conditions such as pulmonary embolism (a blood clot lodged in pulmonary circuit), tension pneumothorax (a collapsed lung with excessive air present in the thoracic cavity), constrictive pericarditis, or cardiac tamponade. Treatments are based on the underlying cause and, in addition to administering fluids intravenously, may include administration of anticoagulant medications, removal of air from the thoracic cavity, removal of fluid from the pericardial cavity, or other types of surgery as required.
Varicose Veins
Varicose veins occur in the superficial veins of the legs when defective valves allow blood to accumulate, causing them to distend, twist, and become visible on the surface of the skin. Varicose veins can occur in anyone, but they are more common in females and often related to pregnancy. Without treatment, varicose veins tend to grow worse over time. Individuals often wear compression socks or support hose and elevate their legs whenever possible to minimize blood pooling. Laser surgery and interventional radiologic procedures can reduce the size and severity of varicose veins. Severe cases may require surgery to remove the damaged vessels. Due to the presence of anastomoses for smaller veins, removal does not typically impair the individual’s circulation.[52] See Figure 11.61[53] for an image of varicose veins.

- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- Mayo Clinic. (2025). Aneurysms. https://www.mayoclinic.org/diseases-conditions/aneurysms/symptoms-causes/syc-20354633 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Desai, D. S., & Hajouli, S. (2023). Arrhythmias. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK558923/ ↵
- “2024_Cardiac_Arrhythmias” by OpenStax College is licensed under CC By 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- “2113ab_Atherosclerosis.” by OpenStax College is licensed under CC BY 3.0 ↵
- Mayo Clinic. (n.d.). Arteriosclerosis/Atherosclerosis. https://www.mayoclinic.org/diseases-conditions/arteriosclerosis-atherosclerosis/symptoms-causes/syc-20350569 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Medstar Health. (2025). Patent foramen ovales and atrial septal defects. https://www.medstarhealth.org/services/patent-foramen-ovale-atrial-septal-defects-treatments ↵
- “2009_Congenital_Heart_Defects” by OpenStax College is licensed under CC BY 3.0 ↵
- Medstar Health. (2025). Patent foramen ovales and atrial septal defects. https://www.medstarhealth.org/services/patent-foramen-ovale-atrial-septal-defects-treatments ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Centers for Disease Control and Prevention. (n.d.). About congenital heart defects. https://www.cdc.gov/heart-defects/about/index.html ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Doyle, T., & Kavanaugh-McHugh, A. (2023). Tetralogy of fallot (TOF): Management and outcome. UpToDate. https://www.uptodate.com ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Centers for Disease Control and Prevention. (n.d.). About congenital heart defects. https://www.cdc.gov/heart-defects/about/index.html ↵
- Doyle, T., & Kavanaugh-McHugh, A. (2023). Tetralogy of fallot (TOF): Management and outcome. UpToDate. https://www.uptodate.com ↵
- Centers for Disease Control and Prevention. (n.d.). About congenital heart defects. https://www.cdc.gov/heart-defects/about/index.html ↵
- U.S. National Library of Medicine. (2023). Cyanotic heart disease. MedlinePlus. https://medlineplus.gov/ency/article/001104.htm ↵
- “2016_Occluded_Coronary_Arteries” by OpenStax College is licensed under CC BY 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing health alterations. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthalts/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- Basile, J., & Bloch, M. J. (2023). Overview of hypertension in adults. UpToDate. https://www.uptodate.com/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- Basile, J., & Bloch, M. J. (2023). Overview of hypertension in adults. UpToDate. https://www.uptodate.com/ ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- Ojha, N., & Dhamoon, A. S. (2023). Myocardial infarction. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537076/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- “Depiction_of_a_person_suffering_from_a_heart_attack_(Myocardial_Infarction).png” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
- Ojha, N., & Dhamoon, A. S. (2023). Myocardial Infarction. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537076/ ↵
- Mayo Clinic. (2024). Pericarditis. https://www.mayoclinic.org/diseases-conditions/pericarditis/symptoms-causes/syc-20352510 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing health alterations. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthalts/ ↵
- “Peripheral_Arterial_Disease.gif” by National Heart Lung and Blood Institute is in the Public Domain ↵
- Haseer Koya, H., & Paul, M. (2023). Shock. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK531492/ ↵
- Haseer Koya, H., & Paul, M. (2023). Shock. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK531492/ ↵
- Taghavi, S., Nassar, A. K., & Askari, R. (2023). Hypovolemic shock. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513297/ ↵
- UCSF Health. (n.d.). Cardiogenic shock. https://www.ucsfhealth.org/conditions/cardiogenic-shock ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2107_Varicose_Vein” by OpenStax College is licensed under CC BY 3.0 ↵
A weakened area in a blood vessel wall that bulges or balloons outward and can rupture, causing severe internal bleeding that may be life-threatening.
An abnormal heart rhythm due to disrupted electrical activity of the conduction system.
A common type of arrhythmia (irregular heartbeat) in which the atria (upper chambers of the heart) beat rapidly and irregularly, reducing the heart’s efficiency and increasing the risk of stroke.
Refers to a disruption in the normal conduction pathway of electrical signals through the atria and ventricles.
Refers to a very rapid heartbeat that originates in the ventricles.
A disorganized heart rhythm that causes the ventricles to quiver instead of contract.
The thickening and stiffening of arterial walls that is commonly associated with normal aging.
A condition where cholesterol, low-density lipoprotein (LDL) deposits, and wastes build up within the lining of the arteries.
Also known as Takotsubo cardiomyopathy, stress-induced cardiomyopathy, or apical ballooning syndrome, it is a temporary heart condition triggered by intense emotional or physical stress. It mimics a heart attack but usually resolves within days or weeks.
A medical emergency in which fluid builds up in the pericardial sac (the lining around the heart), putting pressure on the heart and preventing it from filling and pumping properly.
Structural abnormalities in the heart or blood vessels that are present at birth and affect how blood flows through the heart and out to the rest of the body.
A common congenital heart defect that occurs when the fossa ovalis in the interatrial septum that is present during fetal circulation does not fuse after birth.
A congenital abnormal narrowing of the aorta that is normally located at the insertion of the ligamentum arteriosum, the remnant of the fetal shunt called the ductus arteriosus.
A congenital condition in which the ductus arteriosus fails to close at birth.
A complex set of congenital heart defects that occurs in approximately 400 out of one million live births.
The leading cause of death worldwide. It occurs when the buildup of plaque obstructs blood flow within coronary arteries and decreases compliance of the vessels.
A fatty material including cholesterol, connective tissue, white blood cells, and smooth muscle cells.
A procedure in which the occlusion caused by plaque is mechanically widened with a balloon.
Swelling caused by excess fluid trapped in the body's tissues, often occurring in the hands, feet, ankles, or legs.
Occurs when the heart loses its effectiveness in pumping blood and is referred to as decreased cardiac output.
Refers to chronically elevated blood pressure greater than 120/80 mm Hg.
Meaning the individual was born with the defect.
The most common valve disorder, detected in approximately 2 percent of the population.
The medical term for what is commonly known as a heart attack.
Swelling and irritation of the pericardium, the thin, saclike tissue surrounding the heart.
Caused by atherosclerosis, with narrowed or blocked arteries, causing reduced oxygenated blood flow to the lower extremities.
A life-threatening condition where the body's tissues and organs don't receive enough blood and oxygen.
Caused by hemorrhage or significant fluid losses, often related to severe vomiting or diarrhea or extensive burns.
Results from the inability of the heart to adequately pump and maintain cardiac output.
Characterized by peripheral vasodilation and includes conditions such as septic shock, anaphylactic shock, neurogenic shock or others.
Caused by extracardiac conditions leading to a decrease in the left ventricular cardiac output and decreased delivery of oxygen to tissues.
Occur in the superficial veins of the legs when defective valves allow blood to accumulate, causing them to distend, twist, and become visible on the surface of the skin.

