11.5 Blood Vessels
Blood Vessels[1]
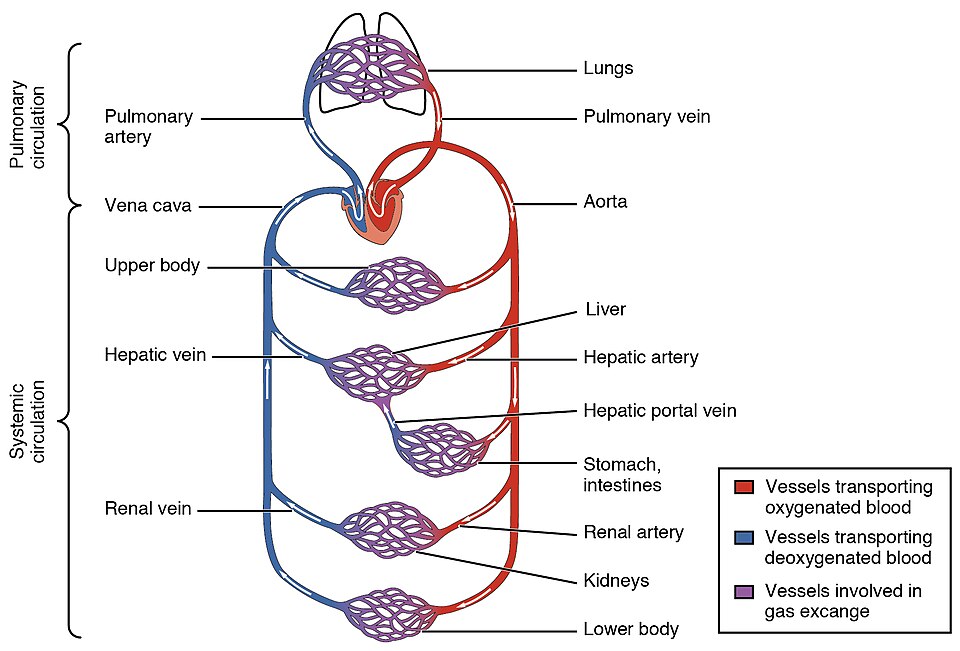
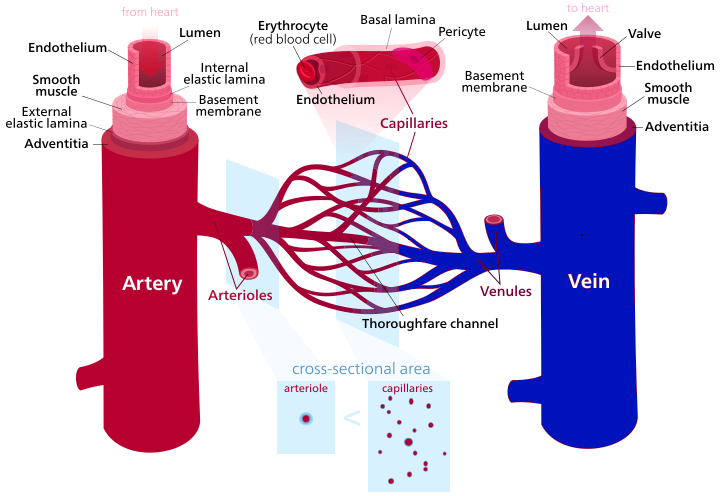
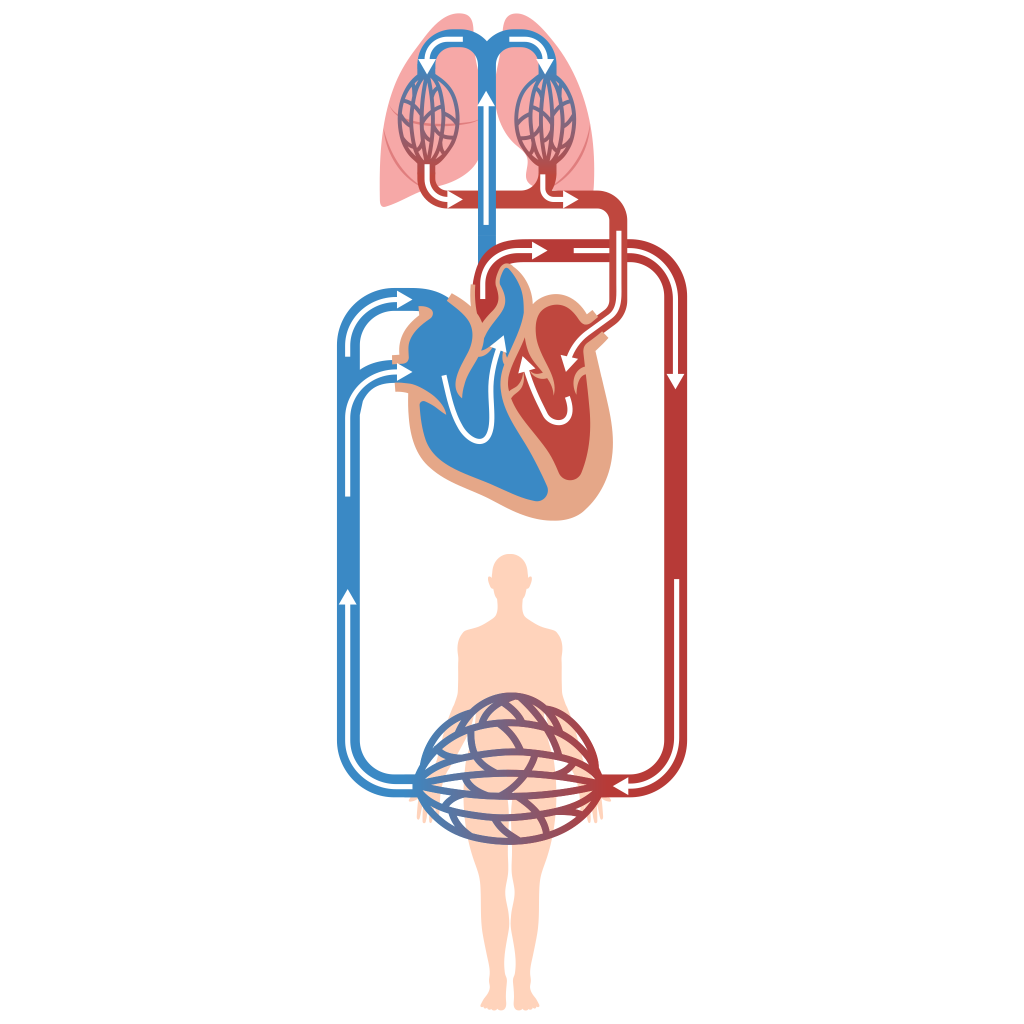
Blood is carried through the body by blood vessels. An artery is a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels. Eventually, the smallest arteries, called arterioles, branch into tiny capillaries, where gases, nutrients, and wastes are exchanged. Capillaries turn into venules, small veins, which carry blood to veins. Veins merge and eventually become the largest veins in the body called the superior and inferior venae cavae that return blood to the heart. As discussed previously in this chapter, arteries and veins transport blood in two distinct circuits: the systemic circuit and the pulmonary circuit. Systemic arteries provide blood rich in oxygen to the body’s tissues. The blood returned to the heart through systemic veins has less oxygen because oxygen carried by the arteries has been delivered to the cells. In contrast, in the pulmonary circuit, arteries carry blood low in oxygen to the lungs for gas exchange. Pulmonary veins then return freshly oxygenated blood from the lungs to the heart to be pumped back out into systemic circulation. See Figure 11.20[2] for an illustration of blood flow through the systemic and pulmonary circuits in vessels carrying oxygenated blood and deoxygenated blood.
Shared Features of Arteries and Veins
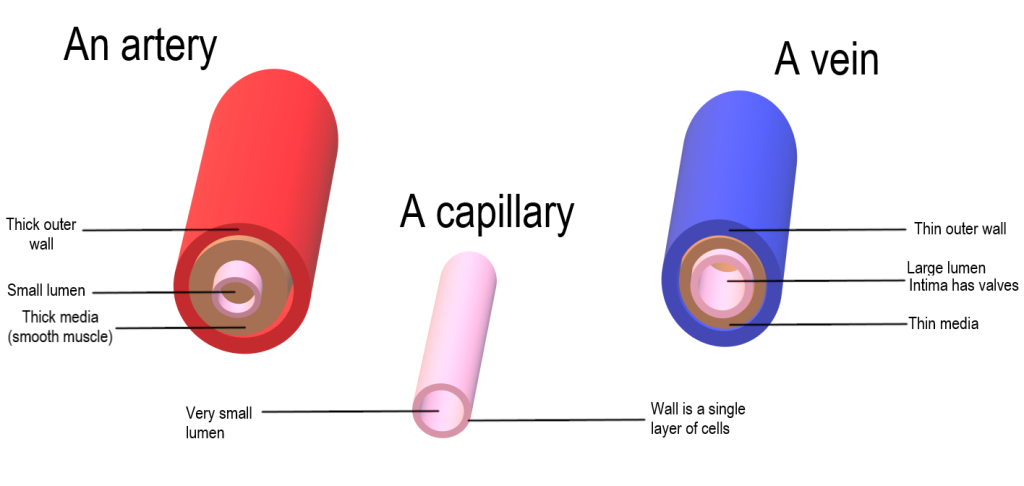
Although arteries and veins differ structurally and functionally, they share certain features. Arteries and arterioles have thicker walls than veins and venules because they are closer to the heart and receive blood that is surging at a far greater pressure.
Each type of vessel has a lumen—a hollow central passageway through which blood flows. Arteries have smaller lumens than veins, a characteristic that helps to maintain the pressure of blood moving through the system. Together, their thicker walls and smaller diameters give arterial lumens a more rounded appearance in cross section than the lumens of veins.
By the time blood has passed through capillaries and entered venules, the pressure initially generated by heart contraction has diminished. In comparison to arteries, venules and veins have a much lower pressure from the blood that flows through them. Their walls are considerably thinner, and their lumens are larger in diameter, allowing more blood to flow with less vessel resistance. In addition, many veins of the body, particularly those of the limbs, contain valves that assist the flow of blood toward the heart. This is critical because blood flow becomes sluggish in the extremities, as a result of the lower pressure and the effects of gravity.
Both arteries and veins have the same three distinct tissue layers, called tunics (from the Latin term tunica) for the garments first worn by ancient Romans. From the inner to outer layers, these tunics are the tunica interna (also known as tunica intima), the tunica media, and the tunica externa.
See Figure 11.21[3] for an illustration showing these three layers and comparing the differences in the walls of arteries and veins.

Tunica Interna
The tunica interna (also called the tunica intima) is composed of smooth epithelial and connective tissue layers. Lining the tunica interna is the specialized simple squamous epithelium called the endothelium, which is continuous throughout the entire vascular system, including the lining of the chambers of the heart. Damage to this endothelial lining and exposure of blood to the deep collagenous fibers are primary causes of clot formation.
Under the microscope, the lumen and the entire tunica interna of a vein will appear smooth, whereas those of an artery will normally appear wavy because of the partial constriction of the smooth muscle in the tunica media.
Tunica Media
The tunica media is the middle layer of the vessel wall. It is generally the thickest layer in arteries. Arteries also have a thicker tunica media compared to veins. The tunica media consists of layers of smooth muscle supported by connective tissue that is primarily made up of elastic fibers, most of which are arranged in circular sheets. Toward the outer portion of the tunic, there are also layers of longitudinal muscle. Contraction and relaxation of the circular muscles decrease and increase the diameter of the vessel lumen, respectively.
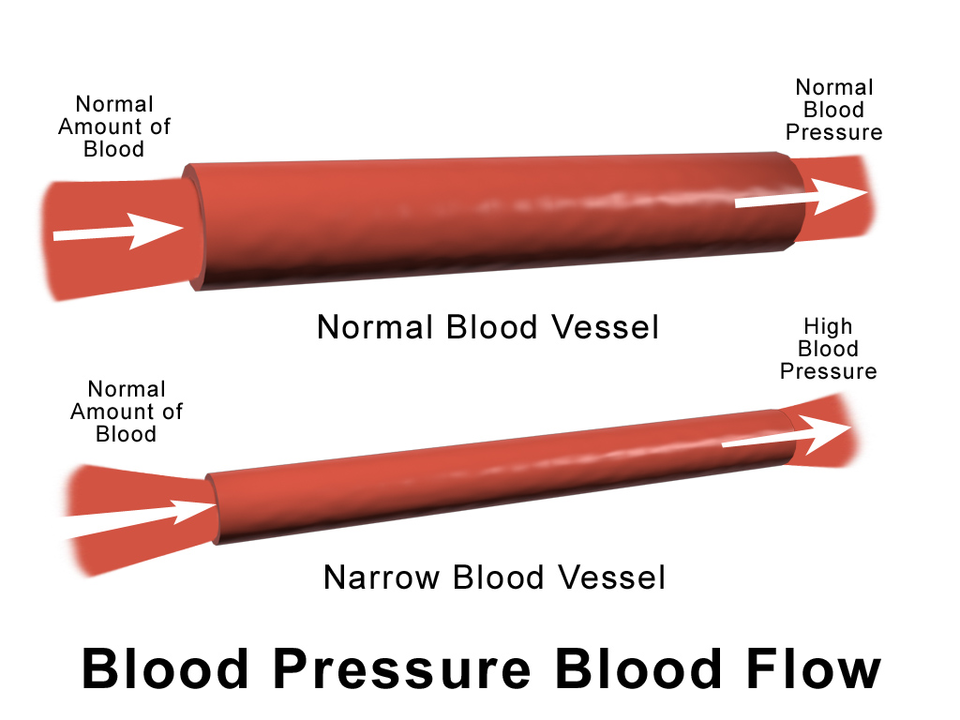
Specifically in arteries, vasoconstriction decreases blood flow as the smooth muscle in the walls of the tunica media contracts, making the lumen narrower and increasing blood pressure. Similarly, vasodilation increases blood flow as the smooth muscle relaxes, allowing the lumen to widen and blood pressure to drop.
Tunica Externa
The outer tunic, the tunica externa (also called the tunica adventitia), is a sheath of connective tissue composed primarily of collagenous fibers. Some bands of elastic fibers are found here as well. This is normally the thickest tunic in veins and may be thicker than the tunica media in some larger arteries. The outer layers of the tunica externa are not distinct but rather blend with the surrounding connective tissue outside the vessel, helping to hold the vessel in position. If you are able to palpate some of the superficial veins in your upper limbs and try to move them, you will find that the tunica externa prevents this. If the tunica externa did not hold the vessel in place, any movement would likely result in disruption of blood flow.
Table 11.5a compares and contrasts the tunics of the arteries and veins. Figure 10.22 compares the appearance of arteries, capillaries, and veins.
Table 11.5a. Comparison of Tunics in Arteries and Veins[4]
| Arteries | Veins | |
|---|---|---|
| General Appearance |
|
|
| Tunica Interna |
|
|
| Tunica Media |
|
|
| Tunica Externa |
|
|
Artery Types and Arterioles
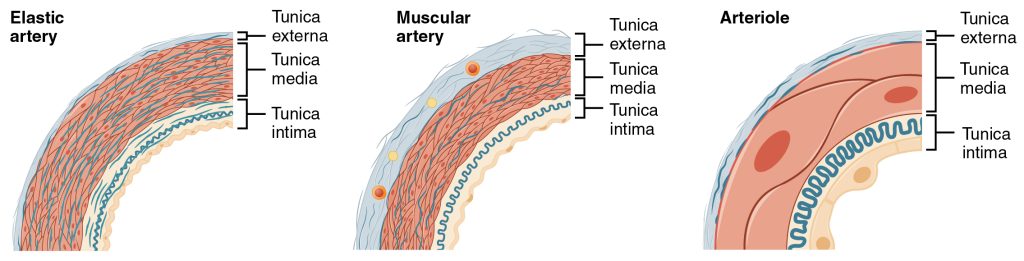
As previously discussed in this chapter, arteries have relatively thick walls that can withstand the high pressure of blood pumped from the heart. Arteries closest to the heart have the thickest walls, containing a high percentage of elastic fibers in all three of their tunics. This type of artery is known as an elastic artery.
Vessels larger than 10 mm in diameter are typically elastic. Their abundant elastic fibers allow them to expand, as blood pumped from the ventricles passes through them, and then to recoil after the surge has passed. If artery walls were rigid and unable to expand and recoil, their resistance to blood flow would greatly increase and blood pressure would be higher, which would require the heart to pump harder to maintain adequate pressure and flow. Artery walls would have to become even thicker in response to this increased pressure. An elastic artery is also known as a conducting artery because the large diameter of the lumen enables it to accept a large volume of blood from the heart and conduct it to smaller branches.
Farther from the heart, where the surge of blood has dampened, the percentage of elastic fibers in an artery’s tunica interna decreases, and the amount of smooth muscle in its tunica media increases. The artery at this point is described as a muscular artery. The diameter of muscular arteries typically ranges from 0.1 mm to 10 mm. Their thick tunica media allows muscular arteries to play a leading role in vasoconstriction. In contrast, their decreased quantity of elastic fibers limits their ability to expand. Fortunately, because the blood pressure has eased by the time it reaches these more distant vessels, elasticity is less important.
Notice that although the distinctions between elastic and muscular arteries are important, there is no clear boundary where an elastic artery suddenly becomes muscular. Rather, there is a gradual transition as the vascular tree repeatedly branches. In turn, muscular arteries branch to distribute blood to the vast network of arterioles. For this reason, a muscular artery is also known as a distributing artery.
An arteriole is a very small artery that leads to a capillary. Arterioles have the same three tunics as the larger vessels, but the thickness of each is greatly diminished. The critical endothelial lining of the tunica interna is intact. The tunica media is restricted to one or two smooth muscle cell layers in thickness. The tunica externa remains but is very thin. With a lumen averaging 30 micrometers or less in diameter, arterioles are critical in slowing down—or resisting—blood flow and causing a substantial drop in blood pressure. The importance of the arterioles is that they will be the primary site of both resistance and regulation of blood pressure.
See Figure 11.23[5] for an illustration comparing the walls of an elastic artery, muscular artery, and arteriole.
Capillaries
A capillary is a microscopic vessel that supplies blood to the tissues, a process called perfusion. Exchange of gases, nutrients, wastes, and other substances occurs between the blood in capillaries and the surrounding cells and their tissue fluid (interstitial fluid). The diameter of a capillary lumen ranges from 5–10 micrometers; the smallest capillaries are just barely wide enough for an erythrocyte to squeeze through. Flow through capillaries is often described as microcirculation.
The wall of a capillary consists of the endothelial layer surrounded by a basement membrane with occasional smooth muscle fibers. There is some variation in wall structure. In a large capillary, several endothelial cells bordering each other may line the lumen; in a small capillary, there may be only a single cell layer that wraps around to contact itself.
Veins and Venules
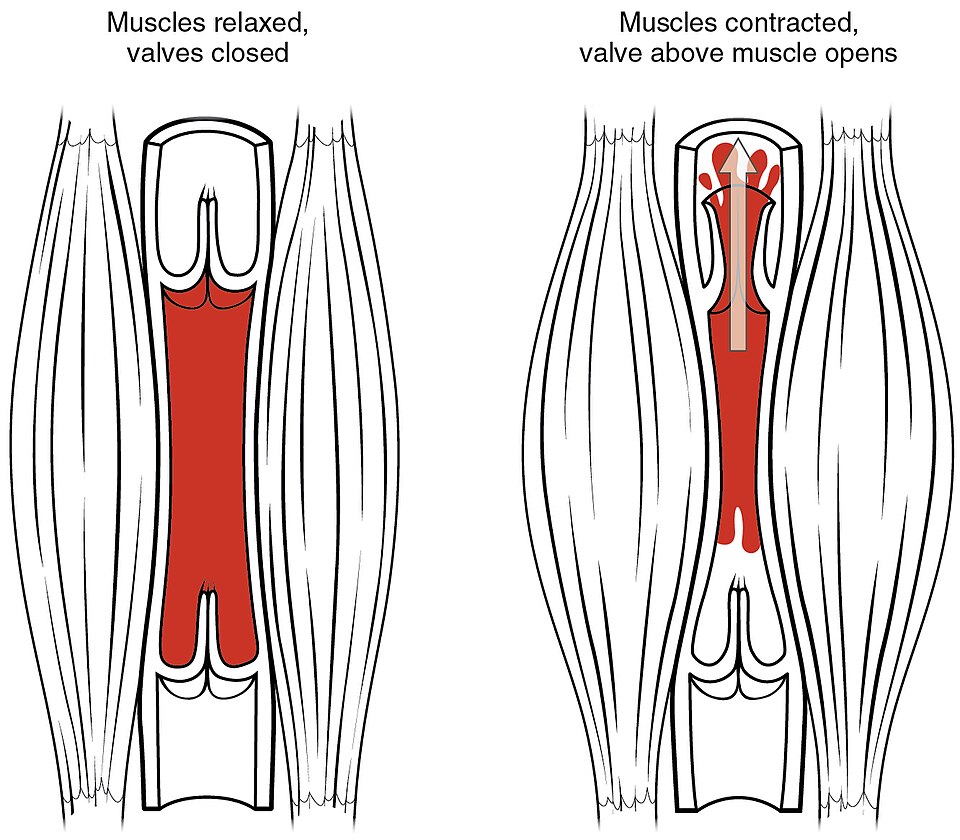
Compared to arteries, veins are thin-walled vessels with large and irregular lumens. Because of the low blood pressure in veins, as well as the pull of gravity, larger veins are commonly equipped with valves that promote the unidirectional flow of blood toward the heart and prevent backflow toward the capillaries.
A venule is an extremely small vein, generally 8–100 micrometers in diameter. Once gas exchange has occurred in the capillaries, blood is ready to start its return to the heart. Venules are the small veins exiting the capillaries. Multiple venules join to form veins. The walls of venules consist of endothelium, a thin tunica media – with a few muscle cells and elastic fibers, plus an outer layer of connective tissue fibers that constitute a very thin tunica externa.
See Figure 11.24[6] for an illustration comparing large veins, medium veins, and venules.
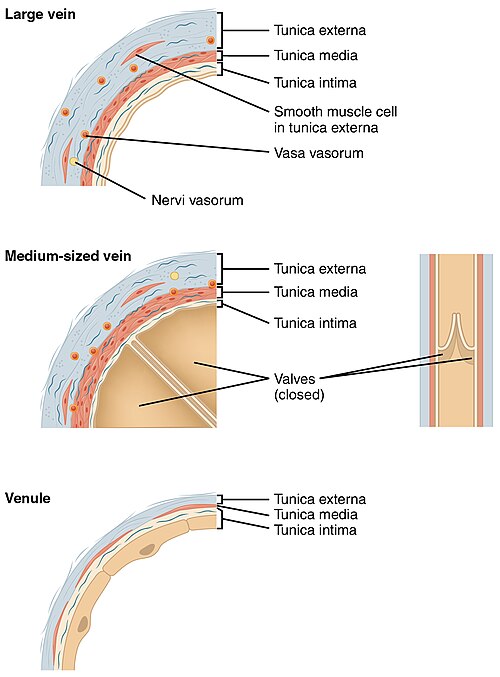
Table 11.5b compares the features of arteries and veins.
Table 11.5b. Comparison of Arteries and Veins[7]
| Arteries | Veins | |
|---|---|---|
| Direction of Blood Flow | Conducts blood away from the heart | Conducts blood toward the heart |
| General Appearance | Rounded | Irregular and often collapsed |
| Blood Pressure | High | Low |
| Wall Thickness | Thick | Thin |
| Relative Oxygen Concentration | Higher in systemic arteries
Lower in pulmonary arteries |
Lower in systemic veins
Higher in pulmonary veins |
| Valves | Not present | Present most commonly in limb veins and in veins inferior to the heart |
See Figure 10.25[8] for an illustration of arteries, arterioles, capillaries, venules, and veins.
Blood Pressure
Blood flow is initiated by the contraction of the ventricles of the heart and refers to the movement of blood through a vessel, tissue, or organ. Ventricular contraction ejects blood into the major arteries, resulting in flow from regions of higher pressure to regions of lower pressure, where blood encounters smaller arteries and arterioles, then capillaries, and then the venules and veins of the venous system.
Hydrostatic pressure is the force exerted by a fluid against the wall of the container in which it is located. One form of hydrostatic pressure is blood pressure, the force exerted by blood on the walls of the blood vessels or the chambers of the heart. Blood pressure typically refers to systemic arterial blood pressure—that is, the pressure of blood flowing in the arteries of the systemic circulation. In clinical practice, this pressure is measured in mmHg (millimeters of mercury) and is typically obtained by applying a sphygmomanometer (blood pressure cuff) on the brachial artery of a patient’s arm.
When systemic arterial blood pressure is measured, it is recorded as a ratio of two numbers expressed as systolic pressure over diastolic pressure. For example, 120/80 mmHg is a normal adult blood pressure. The systolic pressure reflects the arterial pressure resulting from the ejection of blood during ventricular contraction (called systole). The diastolic pressure represents the arterial pressure of blood during ventricular relaxation (called diastole).
Variables Affecting Blood Flow and Blood Pressure
Blood is pumped from the ventricles of the heart into the arteries at high pressure and then blood pressure decreases as blood flows through the arteries, capillaries, and veins. See Figure 11.26[9] for an illustration of the changes in pressures through the circulatory system from the aorta to the venae cavae back into the heart.
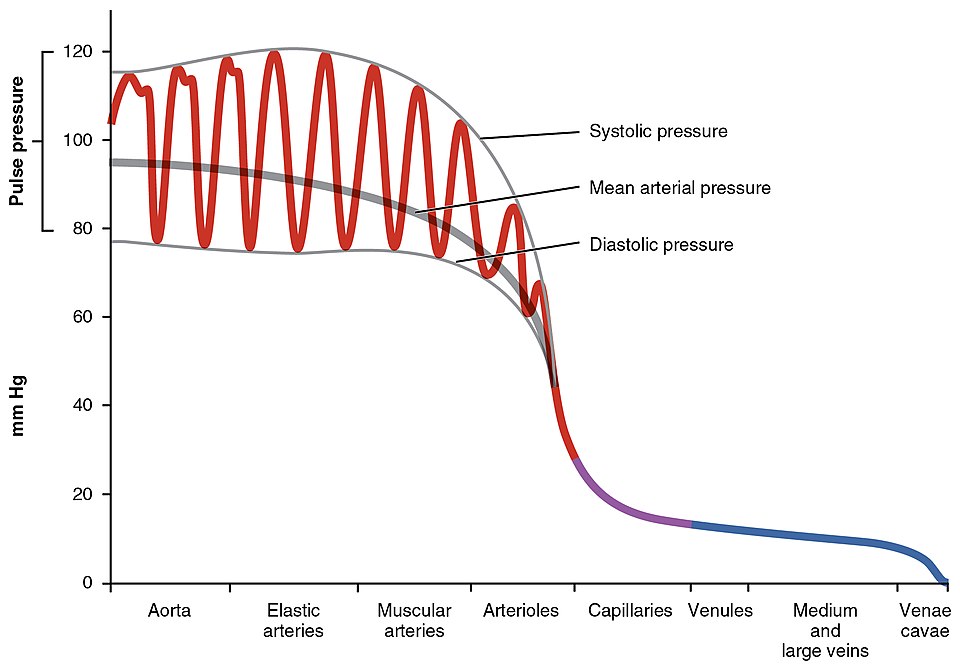
If the pressure inside the arteries increases and cardiac function does not compensate, blood flow decreases to tissues and organs. In the venous system, the opposite relationship is true. Increased pressure inside the veins (such as through the application of compression socks) increases blood flow back to the heart.
Five variables that influence blood flow and blood pressure are as follows:
- Cardiac output
- Compliance (the stretchiness/elasticity of the walls of the blood vessel)
- Blood volume
- Blood viscosity
- Blood vessel length and diameter
Cardiac Output
As previously discussed in this chapter, cardiac output is the measurement of blood flow from the heart through the ventricles and is usually measured in liters per minute. Any factor that causes cardiac output to increase, by elevating heart rate or stroke volume or both, will elevate blood pressure and promote blood flow. For example, sympathetic nervous system stimulation increases the heart rate and cardiac output. Conversely, factors that decrease cardiac output, by decreasing heart rate or stroke volume, will decrease arterial pressure and blood flow. For example, altered levels of potassium or calcium in the blood can cause decreased heart rate and cardiac output.
Compliance
Compliance is the ability to expand or stretch. The greater the compliance of an artery, the more effectively it can expand to accommodate surges in blood flow without increased resistance. (Resistance is anything that slows blood or counteracts blood flow). Veins are more compliant than arteries and can easily expand to hold more blood. However, when vascular disease causes stiffening of the arteries, compliance is reduced and resistance to blood flow is increased, resulting in higher pressure within the vessel and reduced blood flow.
Blood Volume
Under normal circumstances, there is little variation in an individual’s blood volume. However, if blood volume increases, blood pressure and blood flow increase. If blood volume decreases, blood pressure and blood flow decrease.
Low blood volume, called hypovolemia, can be caused by bleeding, dehydration, vomiting, severe burns, or side effects of certain medications. Regulatory mechanisms in the body are so effective at maintaining blood pressure that an individual may be asymptomatic until 10–20 percent of the blood volume has been lost. Treatment of hypovolemia includes treating the cause and typically includes intravenous fluid replacement.
Excessive blood volume, called hypervolemia, is caused by excessive retention of water and sodium that can be caused by heart failure, kidney disease, and side effects of steroid medications. Treatment of hypervolemia includes treating the cause and typically includes medications called diuretics that increase the amount of urine produced by the kidneys to excrete excess water and sodium from the body.
Blood Viscosity
Viscosity is a measure of a fluid’s thickness, which directly influences how easily it flows. Clean water, for example, is less viscous than mud. The viscosity of blood is directly proportional to resistance and inversely proportional to flow; therefore, any condition that causes viscosity to increase will also increase resistance and decrease blood flow. For example, imagine sipping milk and then a milkshake through the same sized straw. There is more resistance and, therefore, less flow due to the increased viscosity of the milkshake. Conversely, any condition that causes viscosity to decrease (such as when the milkshake melts) will decrease resistance and increase flow.
Normally, the viscosity of blood does not change over short periods of time. The two primary determinants of blood viscosity are the formed elements and plasma proteins. Any condition causing increased levels of formed elements, such as polycythemia, can increase viscosity. Conversely, because most plasma proteins are produced by the liver, any condition affecting liver function, such as hepatitis or excessive alcohol intake, can decrease the viscosity of the blood.
Vessel Length and Diameter
Blood vessel length is directly proportional to its resistance, meaning the longer the vessel, the greater the resistance and the lower the flow. The length of blood vessels increases throughout childhood, but under normal physiological circumstances does not change in adulthood. However, the distribution of vessels is not the same in all tissues. Adipose tissue does not have an extensive vascular supply. One pound of adipose tissue contains approximately 200 miles of vessels, whereas skeletal muscle contains more than twice that. An individual weighing 150 pounds has approximately 60,000 miles of vessels in the body. Gaining about 10 pounds adds from 2,000 to 4,000 miles of vessels, depending on the nature of the gained tissue. Blood pressure has to be higher to move blood through the extra miles of vessels. One of the great benefits of weight reduction is the reduced stress to the heart and blood pressure, which does not have to overcome the resistance of as many miles of vessels.
In contrast to length, the diameter of blood vessels varies by vessel type and affects resistance differently. The diameter of any vessel also changes frequently throughout the day in response to neural and chemical signals that trigger contraction and relaxation of smooth muscle, resulting in vasoconstriction or vasodilation of the vessel, respectively. Vessel diameter has an inverse effect on resistance. Vasodilation (widening of vessels) lowers resistance and increases blood flow, whereas vasoconstriction (narrowing of vessels) raises resistance and decreases flow.
See Figure 10.27[10] comparing blood flow in a normal artery versus a narrowed artery.
Pulse
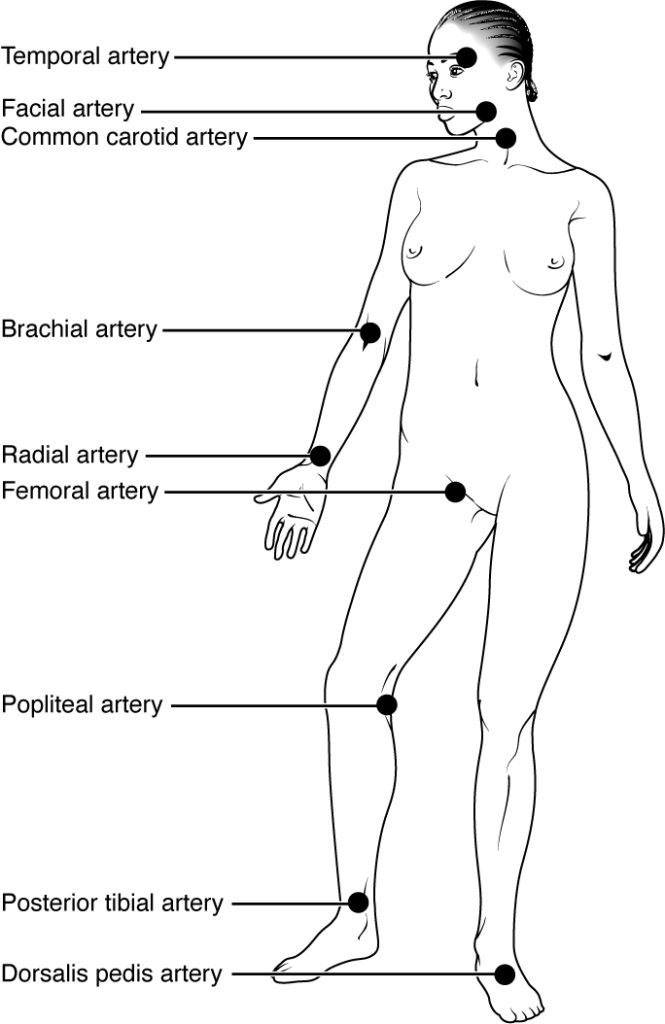
After blood is ejected from the heart, elastic fibers in the arteries help maintain a high-pressure gradient as they expand to accommodate the blood and then recoil. This expansion and recoiling effect, known as the pulse, can be palpated manually or measured electronically. Although the effect diminishes farther from the heart, elements of the systolic and diastolic components of the pulse are still evident down to the level of the arterioles.
Pulse is frequently measured clinically to assess a patient’s state of health and is recorded as beats per minute (bpm). The rate and the strength of the pulse are both important clinical indicators of health. For example, a fast or irregular pulse may indicate an underlying heart condition. The pulse strength represents the strength of ventricular contraction and cardiac output. If the pulse is strong, then systolic pressure is high, but if it is weak, medical intervention may be required to improve cardiac output.
Pulse can be palpated manually by placing the tips of the fingers across an artery that runs close to the body surface and pressing lightly. This procedure is typically performed using the radial artery in the wrist or the common carotid artery in the neck, but other common sites include brachial arteries in the upper arms, femoral arteries in the thighs, popliteal arteries behind the knees, posterior tibial arteries near the ankles, and dorsalis pedis arteries in the feet. See Figure 11.28 for an illustration of pulse sites.
Venous System Pressure
The pumping action of the heart propels the blood into the arteries from an area of higher pressure toward an area of lower pressure. For the blood to flow adequately from the veins back into the heart, the pressure in the veins must be greater than the pressure in the atria of the heart. Two factors help maintain this pressure gradient between the veins and the heart. First, the pressure in the atria during diastole is very low, often approaching zero when the atria are relaxed (atrial diastole). Second, two physiologic “pumps” increase pressure in the venous system, the skeletal muscle pump and the respiratory pump. These “pumps” help return blood to the heart.
Skeletal Muscle Pump
In many body regions, the pressure within the veins can be enhanced by the contraction of the surrounding skeletal muscle. This mechanism, known as the skeletal muscle pump, helps the lower-pressure veins counteract the force of gravity, increasing pressure to return blood to the heart. As leg muscles contract, for example during walking or running, they exert pressure on nearby veins with their numerous one-way valves. This increased pressure causes blood to flow against gravity, opening valves superior to the contracting muscles so blood flows through. Simultaneously, valves inferior to the contracting muscles close, so blood does not flow back down toward the feet. See Figure 11.29[11] for an illustration of the skeletal muscle pump.
Respiratory Pump
The respiratory pump aids blood flow through the veins of the chest and abdomen. During inhalation, the volume of the chest cavity increases, causing air pressure in the chest cavity to decrease and allowing us to inhale. As air pressure within the chest cavity drops, blood pressure in the thoracic veins also drops, falling below the pressure in the abdominal veins. This causes blood to flow into the thoracic region, where pressure is now lower and promotes the return of blood from the thoracic veins to the atria.
Relationships in the Circulatory System
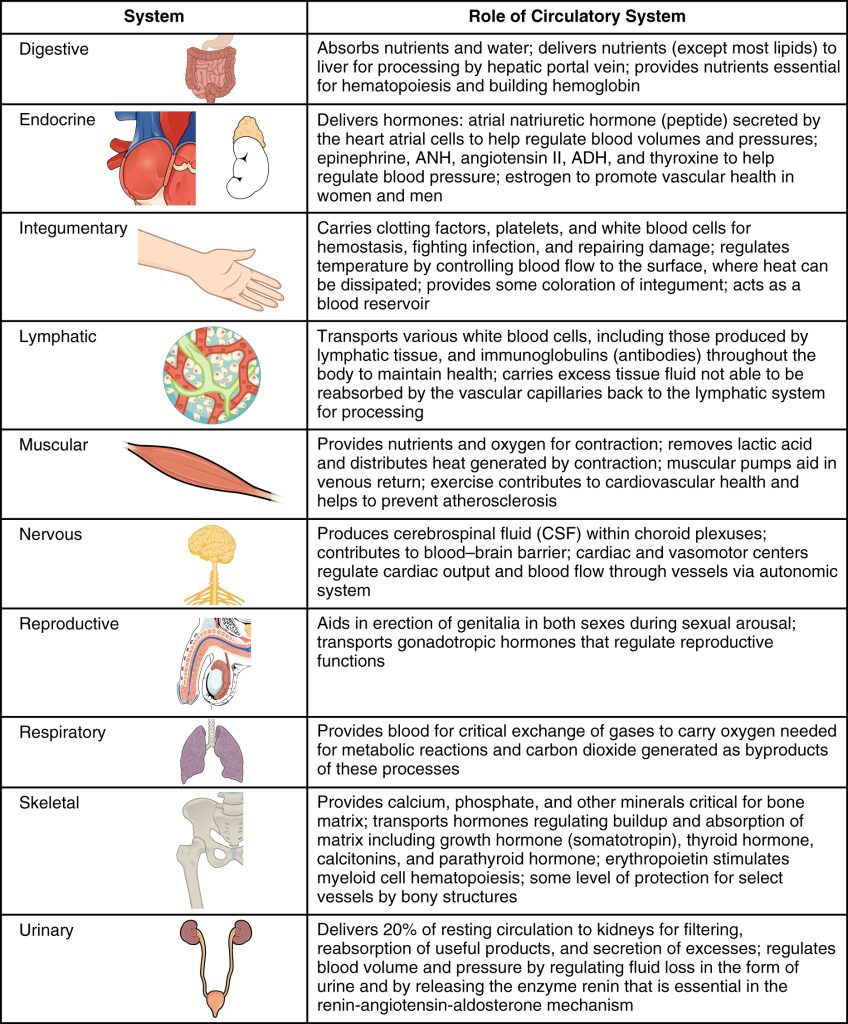
The circulatory system affects nearly every cell, tissue, organ, and system in the body. This includes the generalized and more specialized functions of transport of materials, capillary exchange, maintenance of health by transporting white blood cells and various immunoglobulins (antibodies), hemostasis, regulation of body temperature, and assistance in maintaining acid-base balance. In addition to these shared functions, many systems enjoy a unique relationship with the circulatory system. Figure 11.30[12] summarizes these relationships.
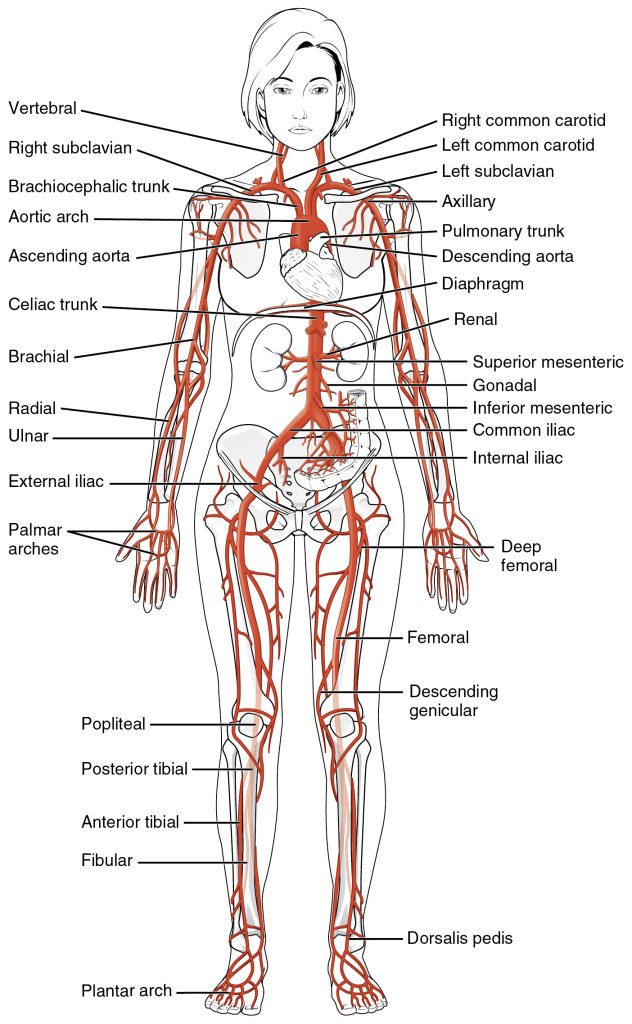
As you learn more about specific vessels of the body, notice that many arteries and veins share the same names, parallel one another throughout the body, and are very similar on the right and left sides of the body. For example, there are a pair of femoral arteries and a pair of femoral veins, with one vessel on each side of the body. In contrast, some vessels closer to the midline of the body, such as the aorta, are unique. Some superficial veins, such as the great saphenous vein in the femoral region, have no arterial counterpart.
Names of vessels can change with location. An artery or vein can change names as it passes an anatomical landmark. For example, the left subclavian artery becomes the axillary artery as it passes through the body wall and into the axillary region and then becomes the brachial artery as it moves from the axillary region into the upper arm (or brachium).
As you read about circulatory pathways, notice that a large artery is referred to as a trunk, indicating that the vessel gives rise to several smaller arteries. For example, the celiac trunk gives rise to the left gastric, common hepatic, and splenic arteries.
As previously discussed in the “Anatomy of the Heart” section, the heart acts as a double pump, simultaneously pumping blood to and from the lungs (pulmonary circulation) and to and from the remainder of the body tissues (systemic circulation). See Figure 10.31[13] for an illustration of the pulmonary and systemic circulation circuits. The vessels in these two circulation circuits will be further discussed in the following two subsections.
Pulmonary Circulation
Blood returning from the systemic circuit enters the right atrium through the superior and inferior venae cavae, as well as the coronary sinus that receives blood from the heart muscle. These vessels will be described more fully later in this section.
This blood is relatively low in oxygen and relatively high in carbon dioxide because much of the oxygen has been dropped off for use by the tissues, and carbon dioxide was picked up to be transported to the lungs for exhalation.
From the right atrium, blood moves into the right ventricle, which pumps it to the lungs for gas exchange. This system of vessels is referred to as the pulmonary circuit.
The single vessel exiting the right ventricle is the pulmonary trunk. At the base of the pulmonary trunk is the pulmonary valve, which prevents backflow of blood into the right ventricle during ventricular diastole. As the pulmonary trunk reaches the superior surface of the heart, it bifurcates (divides) into two branches, a left and a right pulmonary artery. The right pulmonary artery carries deoxygenated blood to the right lung, and the left pulmonary artery carries deoxygenated blood to the left lung.
The right and left pulmonary arteries, in turn, branch many times within each lung, forming a series of smaller arteries and arterioles that eventually lead to the pulmonary capillaries. The pulmonary capillaries surround structures known as alveoli, which are the sites of oxygen and carbon dioxide exchange.
Once gas exchange is completed, oxygenated blood flows from the pulmonary capillaries into a series of pulmonary venules that eventually lead to a series of larger pulmonary veins. Four pulmonary veins, two on the left and two on the right, return blood to the left atrium. At this point, the pulmonary circuit is complete. See Figure 11.32[14] for an illustration of the pulmonary circuit.
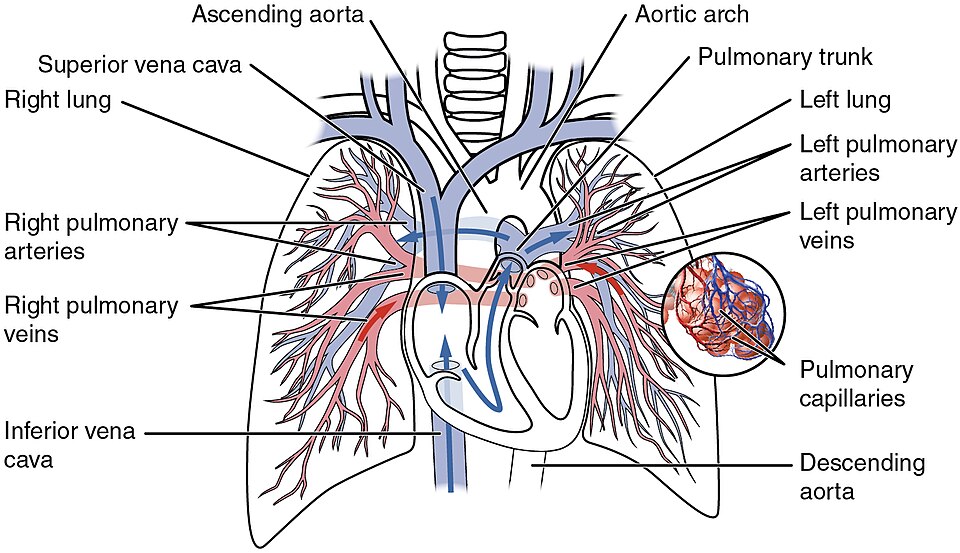
Table 11.5c defines the major arteries and veins of the pulmonary circuit.
Table 11.5c. Pulmonary Trunk, Arteries, and Veins[15]
| Vessel | Description |
|---|---|
| Pulmonary Trunk | Single large vessel exiting the right ventricle that divides into the right and left pulmonary arteries |
| Pulmonary Arteries | Left and right arteries that take deoxygenated blood to each lung; lead to smaller arterioles and eventually to the pulmonary capillaries |
| Pulmonary Veins | Two sets of paired veins—one pair on each side—that take newly oxygenated blood from the lungs to the left atrium of the heart |
Systemic Circulation
From the left atrium, blood moves into the left ventricle, which pumps blood into the aorta. The aorta and its branches—the systemic arteries—send blood to virtually every organ of the body. After the systemic capillaries exchange gases, nutrients, and wastes, the systemic veins and superior vena cava and inferior vena cava return the blood back to the right atrium.
Systemic Arteries
A great approach to learning the vessels is to create simple line drawings, labeling each of the major vessels. It is beyond the scope of this text to name every vessel in the body, but this text will cover the major arteries and veins in the body.
See Figure 11.33[16] for an illustration of the major systemic arteries of the body.
Aorta
The aorta is the largest artery in the body. It arises from the left ventricle and eventually descends to the abdominal region, where it bifurcates (divides) at the level of the fourth lumbar vertebra into the two common iliac arteries.
The aorta consists of the ascending aorta (or aortic root), the aortic arch, and the descending aorta, which passes through the diaphragm, a large dome-shaped muscle that divides the thorax from the abdomen. The descending aorta in the chest is called the thoracic aorta. Once the aorta enters the abdominal region, it is called the abdominal aorta. Arteries originating from the aorta ultimately distribute blood to virtually all tissues of the body.
At the base of the aorta is the aortic valve, which prevents backflow of blood into the left ventricle while the heart is relaxing. After exiting the left ventricle, the ascending aorta moves in an upward direction. Following this ascent, it forms a graceful arc to the left, called the aortic arch. The aortic arch descends toward the abdomen and ends at the level of the intervertebral disk between the fourth and fifth thoracic vertebrae. Now called the descending aorta, it passes through an opening in the diaphragm known as the aortic hiatus. Superior to the diaphragm, the aorta is called the thoracic aorta, and inferior to the diaphragm, it is called the abdominal aorta. See Figure 11.34[17] for an illustration of the ascending aorta, the aortic arch, and the initial segment of the descending aorta plus major branches.
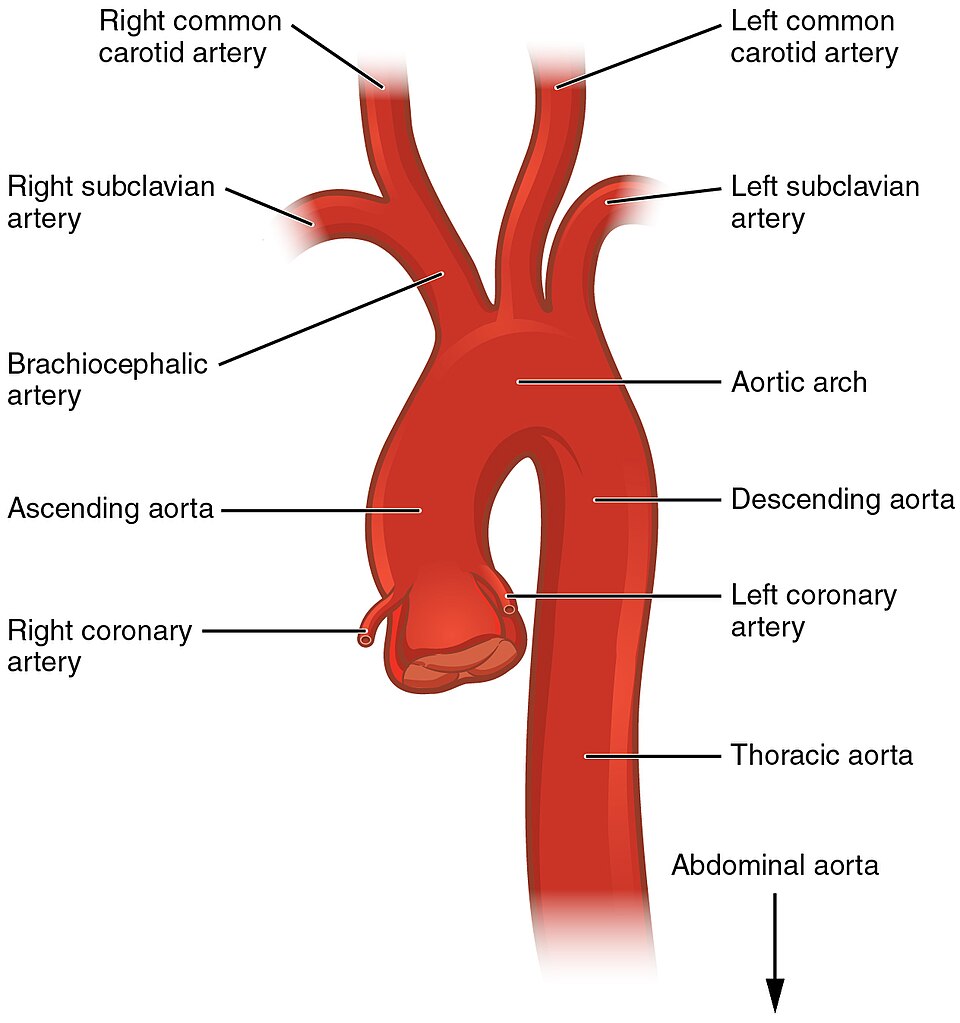
Table 11.5d summarizes the structures of the aorta.
Table 11.5d. Structures of the Aorta[18]
| Vessel | Description |
|---|---|
| Aorta | Largest artery in the body, originating from the left ventricle and descending to the abdominal region, where it divides into the common iliac arteries at the level of the fourth lumbar vertebra; arteries originating from the aorta distribute blood to virtually all tissues of the body |
| Ascending Aorta | Initial portion of the aorta, rising superiorly from the left ventricle for a distance of approximately 5 cm |
| Aortic Arch | Graceful arc to the left that connects the ascending aorta to the descending aorta; ends at the intervertebral disk between the fourth and fifth thoracic vertebrae |
| Descending Aorta | Portion of the aorta that continues inferiorly past the end of the aortic arch; subdivided into the thoracic aorta and the abdominal aorta |
| Thoracic Aorta | Portion of the descending aorta superior to the diaphragm |
| Abdominal Aorta | Portion of the descending aorta inferior to the diaphragm and superior to the common iliac arteries |
Coronary Arteries
The first vessels that branch off of the ascending aorta are the paired coronary arteries. Refer back to Figure 11.34 to view the coronary arteries emerging from the aorta. The coronary arteries encircle the heart, forming a ring-like structure that divides into the next level of branches that supply blood to the myocardium of the heart.
Aortic Arch Branches
There are three major branches from the aortic arch: the brachiocephalic artery, the left common carotid artery, and the left subclavian (literally “under the clavicle”) artery:
- The brachiocephalic artery is located only on the right side of the body; there is no corresponding artery on the left. The brachiocephalic artery branches into the right subclavian artery and the right common carotid artery.
- The left common carotid artery branches directly from the aortic arch.
- The left subclavian artery branches directly from the aortic arch.
Refer back to Figure 11.34 to view these three major aortic arch branches emerging from the aortic arch.
The right and left subclavian arteries supply blood to the arms, chest, shoulders, back, and central nervous system. The right and left common carotid arteries divide into internal and external carotid arteries.
The external carotid artery supplies blood to numerous structures within the face, lower jaw, neck, esophagus, and larynx. These branches include the lingual, facial, occipital, maxillary, and superficial temporal arteries. The internal carotid arteries, along with the vertebral arteries, are the two primary suppliers of blood to the human brain. Given the central role and vital importance of the brain to life, it is critical that blood supply to this organ remains uninterrupted. Both the carotid and vertebral arteries branch once they enter the cranial cavity, and some of these branches form a structure known as the arterial circle (or circle of Willis), an anastomosis that is remarkably like a traffic circle that sends off branches (in this case, arterial branches to the brain). As a rule, branches to the anterior portion of the cerebrum are normally fed by the internal carotid arteries; the remainder of the brain receives blood flow from branches associated with the vertebral arteries. See Figure 11.35[19] for an illustration of arteries supplying the head and neck and Figure 11.36[20] for an illustration of arteries supplying the brain.
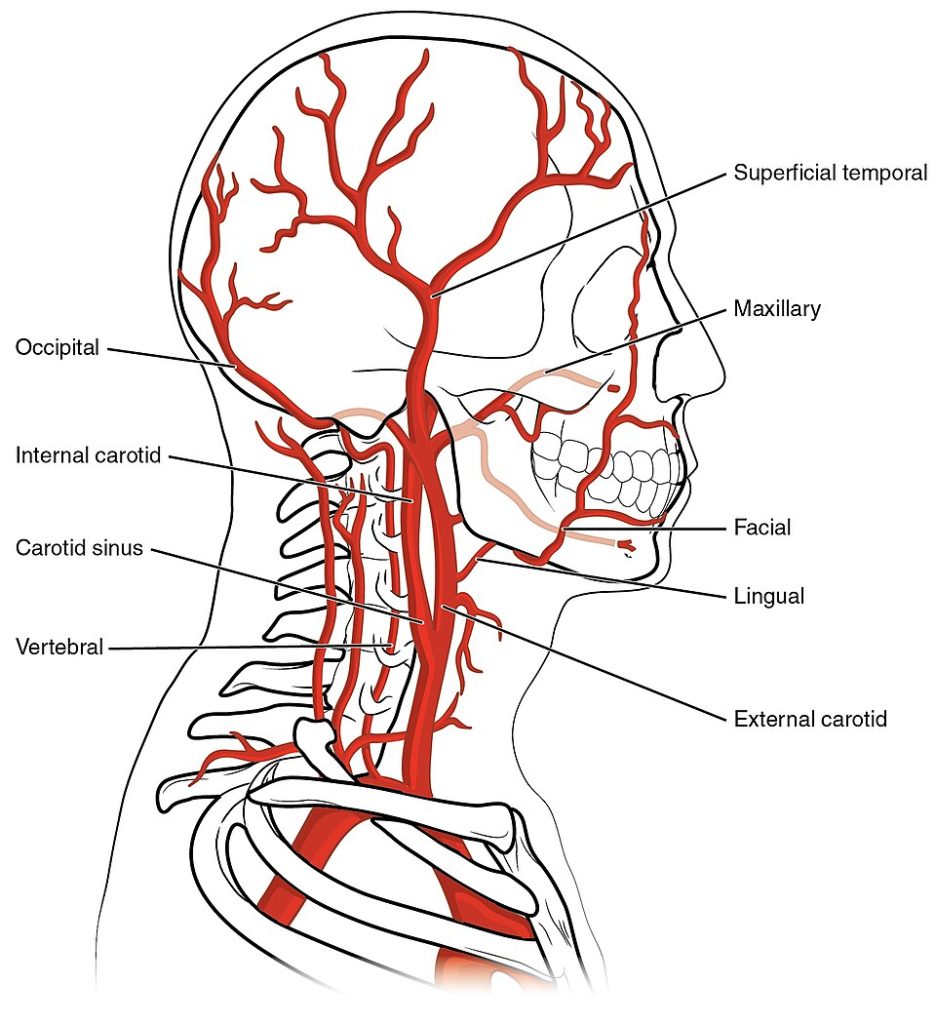
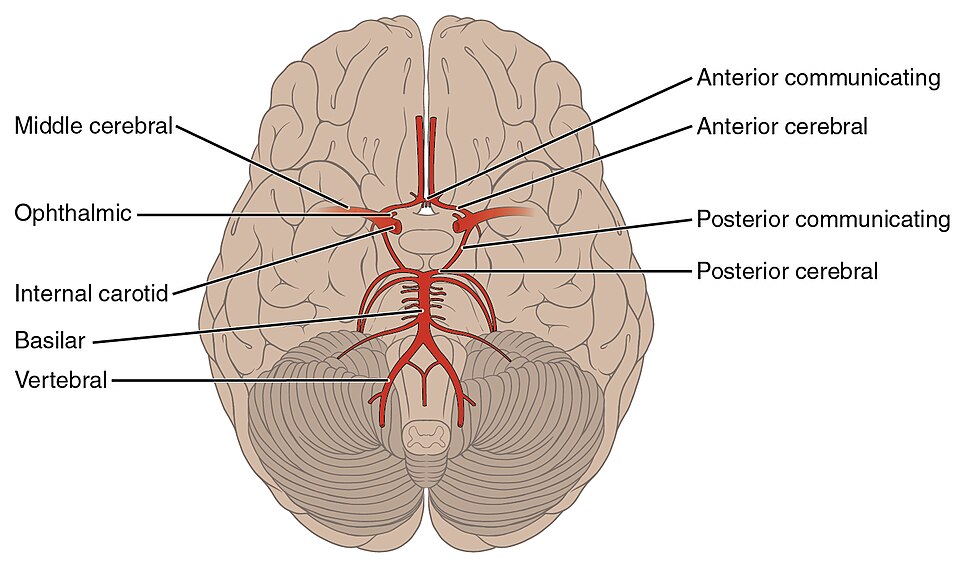
Table 11.5e summarizes the aortic arch branches, including the major branches supplying the brain.
Table 11.5e. Major Aortic Arch Branches and Arteries Supplying the Brain[21]
| Vessel | Description |
|---|---|
| Brachiocephalic Artery | Single vessel located on the right side of the body; the first vessel branching from the aortic arch; gives rise to the right subclavian artery and the right common carotid artery; supplies blood to the head, neck, upper limb, and wall of the thoracic region |
| Subclavian Arteries | The right subclavian artery arises from the brachiocephalic artery while the left subclavian artery arises from the aortic arch; gives rise to the internal thoracic, vertebral, and thyrocervical arteries; supplies blood to the arms, chest, shoulders, back, and central nervous system |
| Vertebral Arteries | Arises from the subclavian artery and passes through the transverse foramina of the cervical vertebrae and then through the foramen magnum to the brain; joins with the internal carotid artery to form the arterial circle; supplies blood to the brain and spinal cord |
| Common Carotid Arteries | The right common carotid artery arises from the brachiocephalic artery, and the left common carotid artery arises from the aortic arch; each gives rise to the external and internal carotid arteries; supplies the respective sides of the head and neck |
| External Carotid Arteries | Arises from the common carotid artery; supplies blood to numerous structures within the face, lower jaw, neck, esophagus, and larynx |
| Internal Carotid Arteries | Arises from the common carotid artery and begins with the carotid sinus; goes through the carotid canal of the temporal bone to the base of the brain; combines with the branches of the vertebral artery, forming the arterial circle; supplies blood to the brain |
| Arterial Circle or Circle of Willis | An anastomosis located at the base of the brain that ensures continual blood supply; formed from the branches of the internal carotid and vertebral arteries; supplies blood to the brain |
Major Branches of the Thoracic Aorta
The thoracic aorta begins at the level of vertebra T5 and continues to the diaphragm. As it passes through the thoracic region, the thoracic aorta gives rise to several branches, which are collectively referred to as visceral branches and parietal branches. These branches supply various organs and muscles in the thoracic region. See Figure 11.37[22] for an illustration of major branches of the thoracic aorta.
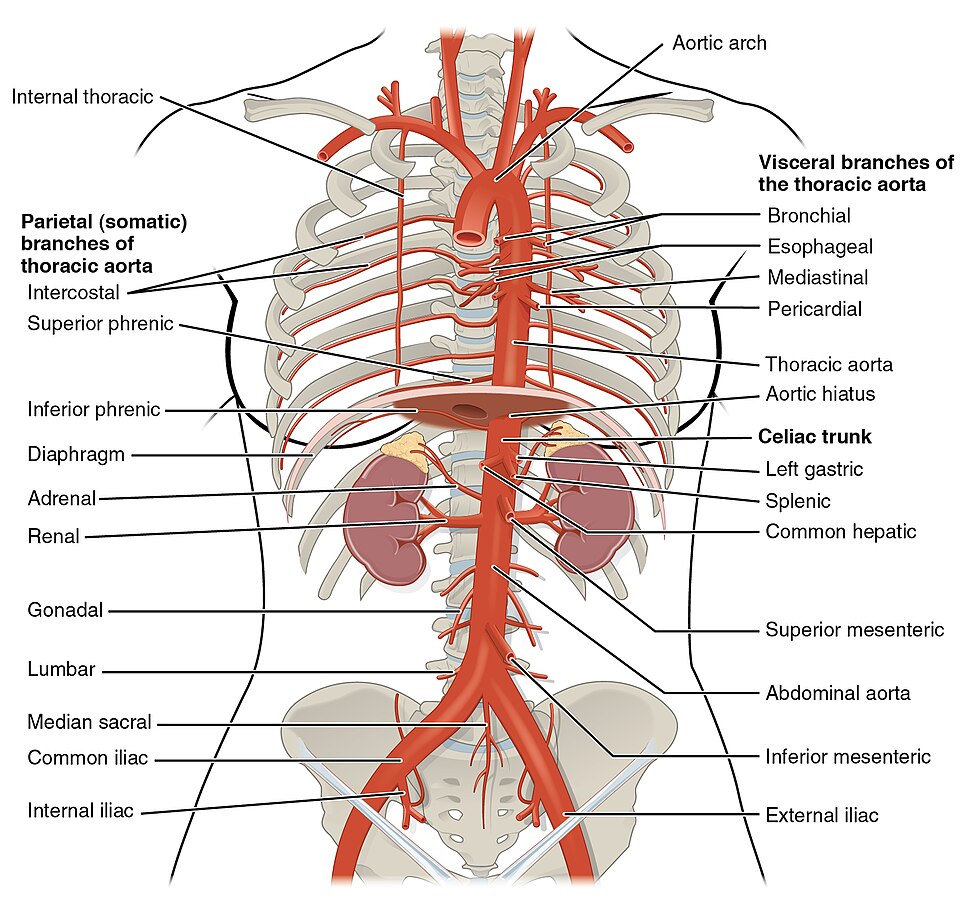
Abdominal Aorta and Major Branches
After passing through the diaphragm, the thoracic aorta is called the abdominal aorta. It formally ends at approximately the level of vertebra L4, where it divides to form the common iliac arteries. The abdominal aorta gives rise to several important branches.
A single celiac trunk emerges and divides into the left gastric artery to supply blood to the stomach and esophagus, the splenic artery supplies blood to the spleen, and the common hepatic artery, which, in turn, gives rise to the hepatic artery proper to supply blood to the liver.
Two additional single vessels arise from the abdominal aorta. These are the superior and inferior mesenteric arteries. The superior mesenteric artery arises approximately 2.5 cm inferior to the celiac trunk and branches into several major vessels that supply blood to the small intestine (duodenum, jejunum, and ileum), the pancreas, and a majority of the large intestine. The inferior mesenteric artery supplies blood to the distal segment of the large intestine, including the rectum. It arises approximately 5 cm superior to the common iliac arteries.
In addition to these single branches, the abdominal aorta gives rise to several significant paired arteries along the way. These include the inferior phrenic arteries, the adrenal arteries, the renal arteries, the gonadal arteries, and the lumbar arteries.
Each inferior phrenic artery is a counterpart of a superior phrenic artery and supplies blood to the inferior surface of the diaphragm. The adrenal artery supplies blood to the adrenal glands and arises near the superior mesenteric artery. Each renal artery branches approximately 2.5 cm inferior to the superior mesenteric arteries and supplies a kidney. The right renal artery is longer than the left because the aorta lies to the left of the vertebral column and the vessel must travel a greater distance to reach its target. Renal arteries branch repeatedly to supply blood to the kidneys.
Each gonadal artery supplies blood to the gonads, or reproductive organs, and is also described as either an ovarian artery or a testicular artery, depending upon the sex of the individual. An ovarian artery supplies blood to an ovary, Fallopian tube, and the uterus and is located within the suspensory ligament of the uterus. It is considerably shorter than a testicular artery, which ultimately travels outside the body cavity to the testes, forming one component of the spermatic cord. The gonadal arteries arise inferior to the renal arteries and are generally retroperitoneal. The ovarian artery continues to the uterus where it forms an anastomosis with the uterine artery that supplies blood to the uterus. Both the uterine arteries and vaginal arteries, which distribute blood to the vagina, are branches of the internal iliac artery.
The aorta divides at approximately the level of vertebra L4 into a left and a right common iliac artery but continues as a small vessel, the median sacral artery, into the sacrum.
The common iliac arteries provide blood to the pelvic region and, ultimately, to the lower limbs. They split into external and internal iliac arteries approximately at the level of the lumbar-sacral articulation. Each internal iliac artery sends branches to the urinary bladder, the walls of the pelvis, the external genitalia, and the medial portion of the femoral region. In females, they also provide blood to the uterus and vagina. The much larger external iliac artery supplies blood to each of the lower limbs. Figure 11.38[23] shows the distribution of the major branches of the aorta into the thoracic and abdominal regions.
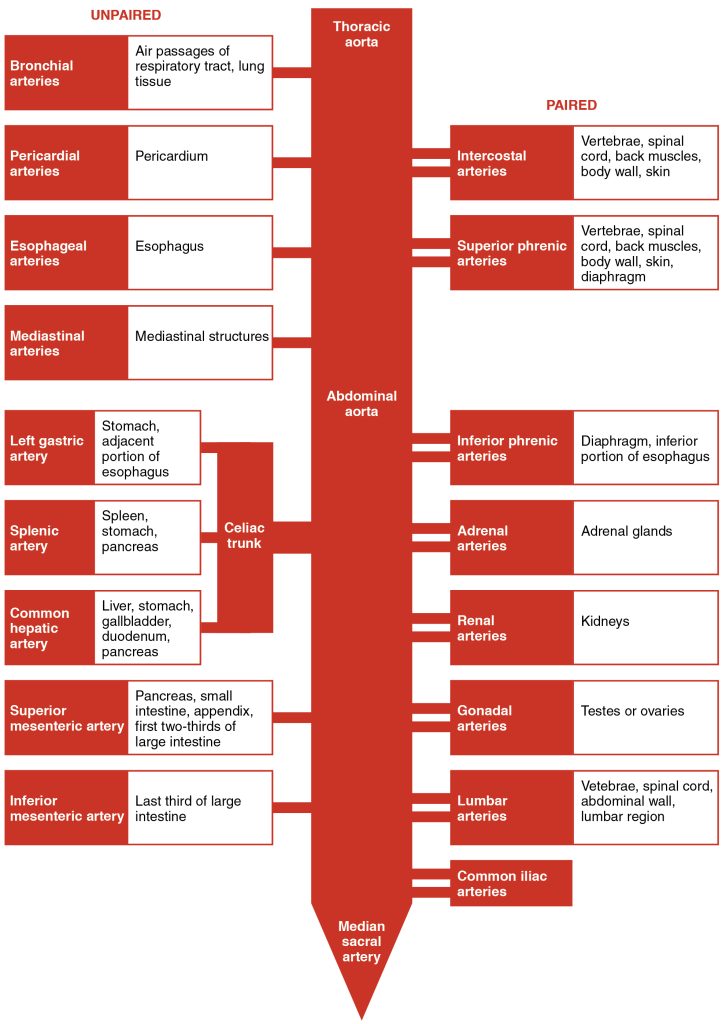
Figure 11.39[24] shows the distribution of the major branches of the common iliac arteries.
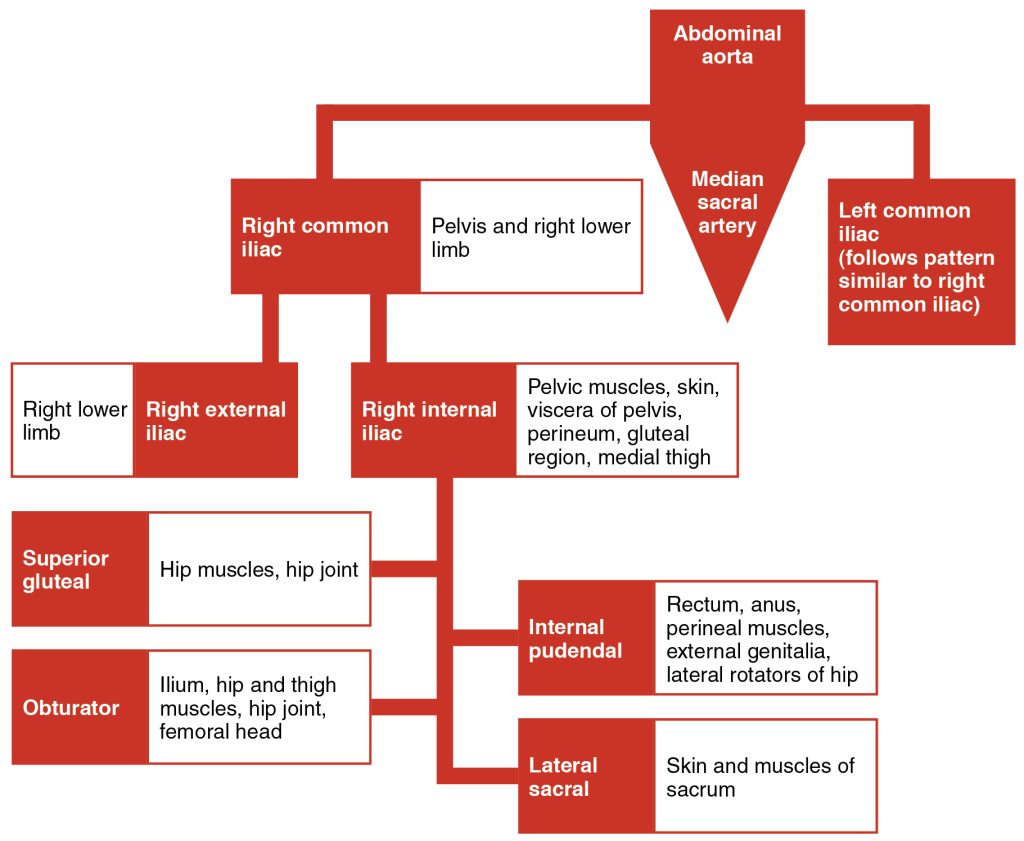
Table 11.5f summarizes the major branches of the abdominal aorta.
Table 11.5f. Vessels of the Abdominal Aorta[25]
| Vessel | Description |
|---|---|
| Celiac Trunk | Also called the celiac artery; a major branch of the abdominal aorta; gives rise to the left gastric artery, the splenic artery, and the common hepatic artery |
| Left Gastric Artery | Branch of the celiac trunk; supplies blood to the stomach |
| Splenic Artery | Branch of the celiac trunk; supplies blood to the spleen |
| Common Hepatic Artery | Branch of the celiac trunk that forms the proper hepatic artery, the right gastric artery, and the gastroduodenal artery |
| Proper Hepatic Artery | Branch of the common hepatic artery; supplies systemic blood to the liver and gallbladder |
| Right Gastric Artery | Branch of the common hepatic artery; supplies blood to the stomach |
| Gastroduodenal Artery | Branch of the common hepatic artery; supplies blood to the stomach and duodenum |
| Superior Mesenteric Artery | Branch of the abdominal aorta; supplies blood to the small intestine (duodenum, jejunum, and ileum), the pancreas, and a majority of the large intestine |
| Inferior Mesenteric Artery | Branch of the abdominal aorta; supplies blood to the distal segment of the large intestine and rectum |
| Inferior Phrenic Arteries | Branches of the abdominal aorta; supply blood to the inferior surface of the diaphragm |
| Adrenal Arteries | Branch of the abdominal aorta; supplies blood to the adrenal (suprarenal) glands |
| Renal Arteries | Branch of the abdominal aorta; supplies blood to each kidney |
| Gonadal Arteries | Branch of the abdominal aorta; supplies blood to the gonads or reproductive organs; also described as ovarian arteries or testicular arteries, depending upon the sex of the individual |
| Ovarian Arteries | Branch of the abdominal aorta; supplies blood to ovary, uterine (Fallopian) tube, and uterus |
| Testicular Arteries | Branch of the abdominal aorta; ultimately travels outside the body cavity to the testes and forms one component of the spermatic cord |
| Common Iliac Arteries | Branch of the aorta that leads to the internal and external iliac arteries |
| Median Sacral Artery | Continuation of the aorta into the sacrum |
| Internal Iliac Arteries | Branch from the common iliac arteries; supplies blood to the urinary bladder, walls of the pelvis, external genitalia, and the medial portion of the femoral region; in females, also provides blood to the uterus and vagina |
| External Iliac Arteries | Branch of the common iliac artery that leaves the body cavity and becomes a femoral artery; supplies blood to the lower limbs |
Arteries Serving the Upper Limbs
As the subclavian artery exits the thorax into the axillary region, it is renamed the axillary artery. Although it does branch and supply blood to the region near the head of the humerus, the majority of the vessel continues into the upper arm, or brachium, and becomes the brachial artery.
The brachial artery supplies blood to much of the brachial region and divides at the elbow into several smaller branches, including the deep brachial arteries, which provide blood to the posterior surface of the arm, and the ulnar collateral arteries, which supply blood to the region of the elbow. As the brachial artery approaches the coronoid fossa, it bifurcates (divides) into the radial and ulnar arteries, which continue into the forearm, or antebrachium.
The radial artery and ulnar artery parallel their namesake bones, giving off smaller branches until they reach the wrist, or carpal region. At this level, they fuse to form the superficial and deep palmar arches that supply blood to the hand, as well as the digital arteries that supply blood to the digits.
See Figure 11.40[26] for an illustration of the major arteries of the upper limbs.
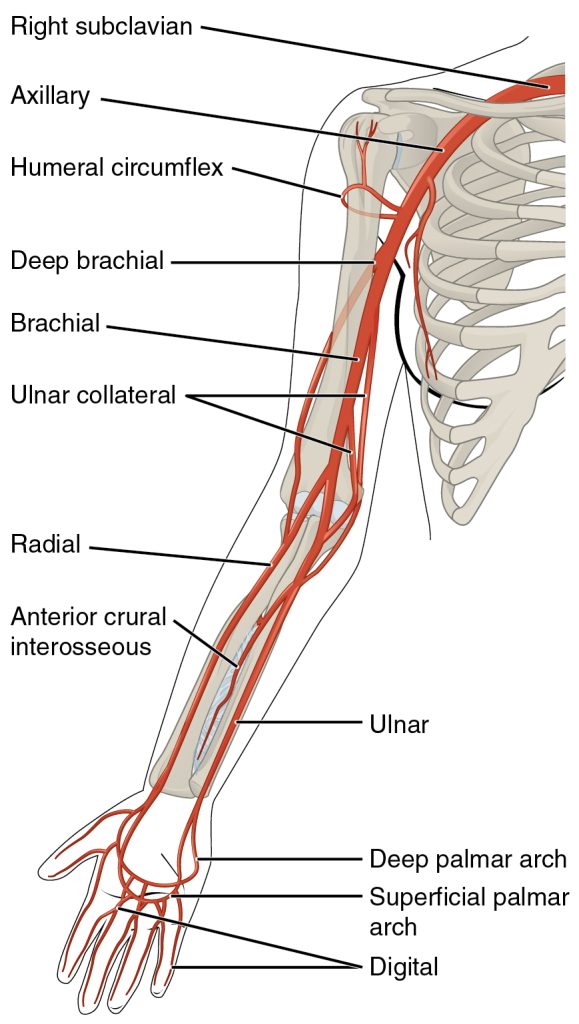
Figure 11.41[27] shows the distribution of systemic arteries from the heart into the upper limb.
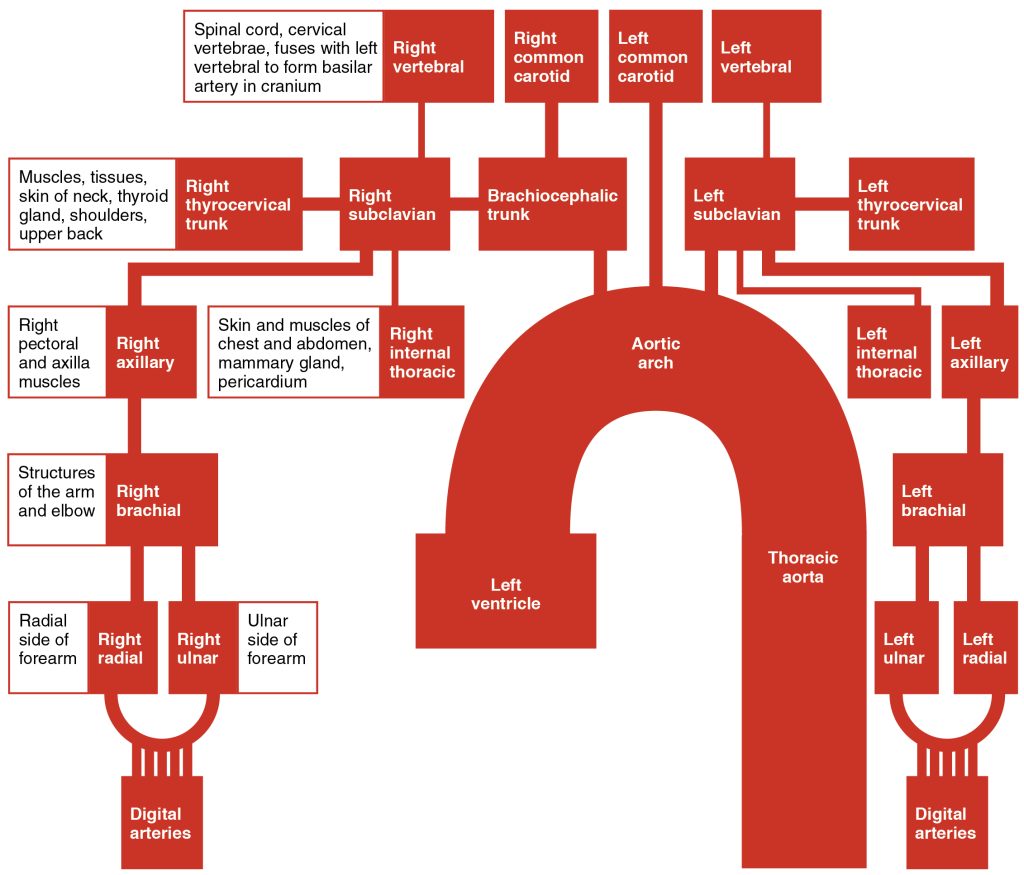
Table 11.5g summarizes the arteries serving the upper limbs.
Table 11.5g. Arteries Serving the Upper Limbs[28]
| Vessel | Description |
|---|---|
| Axillary Arteries | Continuation of the subclavian artery as it penetrates the body wall and enters the axillary region; supplies blood to the region near the head of the humerus (humeral circumflex arteries); the majority of the vessel continues into the brachium and becomes the brachial artery |
| Brachial Arteries | Continuation of the axillary artery in the brachium; supplies blood to much of the brachial region; gives off several smaller branches that provide blood to the posterior surface of the arm in the region of the elbow; bifurcates into the radial and ulnar arteries at the coronoid fossa |
| Radial Arteries | Formed at the bifurcation of the brachial artery; parallels the radius; gives off smaller branches until it reaches the carpal region where it fuses with the ulnar artery to form the superficial and deep palmar arches; supplies blood to the lower arm and carpal region |
| Ulnar Arteries | Formed at the bifurcation of the brachial artery; parallels the ulna; gives off smaller branches until it reaches the carpal region where it fuses with the radial artery to form the superficial and deep palmar arches; supplies blood to the lower arm and carpal region |
| Palmar Arches (Superficial and Deep) | Formed from anastomosis of the radial and ulnar arteries; supply blood to the hand and digital arteries |
| Digital Arteries | Formed from the superficial and deep palmar arches; supply blood to the digits |
Arteries Serving the Lower Limbs
The external iliac artery exits the body cavity and enters the femoral region of the lower leg. When it enters the thigh, it is renamed the femoral artery. It gives off several smaller branches, as well as the lateral deep femoral artery that, in turn, gives rise to a lateral circumflex artery. These arteries supply blood to the deep muscles of the thigh, as well as ventral and lateral regions of the integument. The femoral artery also gives rise to the genicular artery, which provides blood to the region of the knee. As the femoral artery passes posterior to the knee near the popliteal fossa, it is called the popliteal artery. The popliteal artery branches into the anterior and posterior tibial arteries.
The anterior tibial artery is located between the tibia and fibula and supplies blood to the muscles and skin of the anterior tibial region. Upon reaching the tarsal region, it becomes the dorsalis pedis artery, which branches repeatedly and provides blood to the tarsal and dorsal regions of the foot.
The posterior tibial artery provides blood to the muscles and skin on the posterior surface of the tibial region. The fibular or peroneal artery branches from the posterior tibial artery. It bifurcates (divides) and becomes the medial plantar artery and lateral plantar artery, providing blood to the plantar surfaces.
There is an anastomosis with the dorsalis pedis artery and the medial and lateral plantar arteries that form two arches called the dorsal arch (also called the arcuate arch) and the plantar arch, which provide blood to the remainder of the foot and toes.
See Figure 11.42[29] for an illustration of the major arteries in the leg.
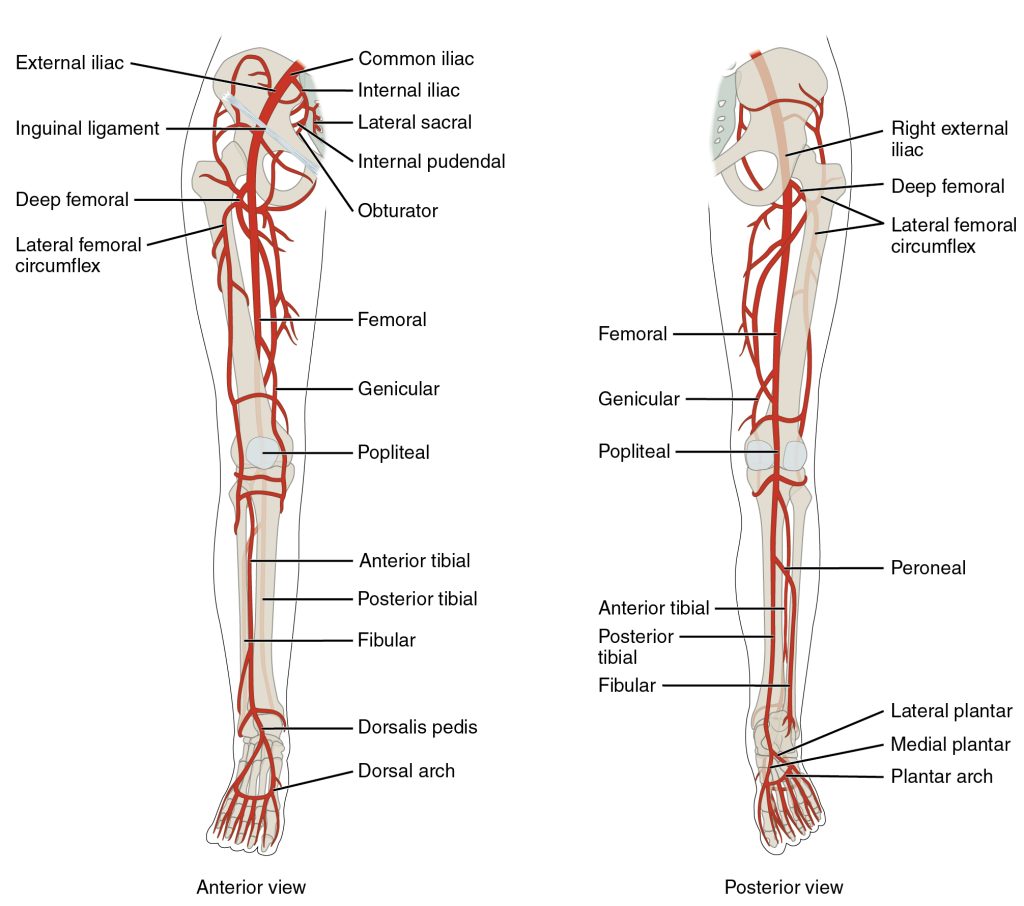
Figure 11.43[30] shows the distribution of the major systemic arteries in the lower limb.
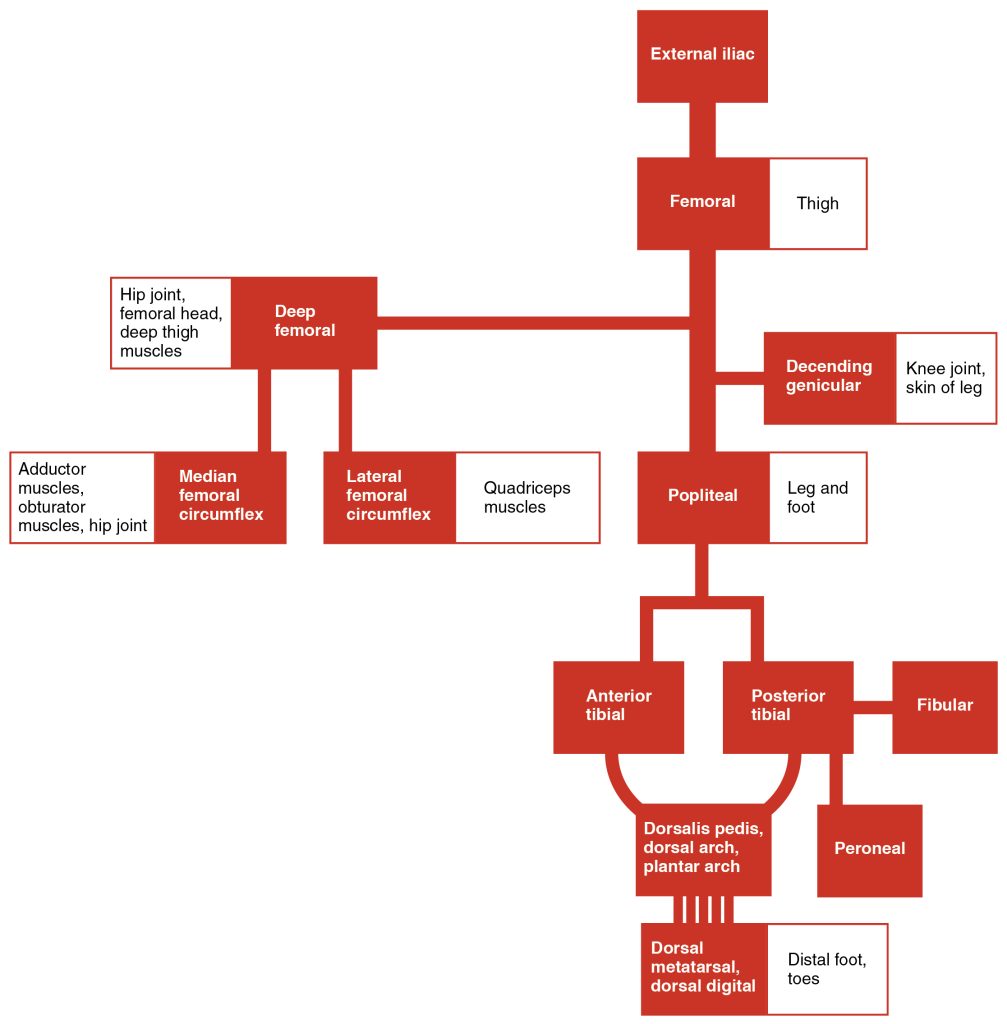
Table 11.5h summarizes the major arteries serving the lower limbs.
Table 11.5h. Arteries Serving the Lower Limbs[31]
| Vessel | Description |
|---|---|
| Femoral Arteries | Continuation of the external iliac artery after it enters the thigh; divides into several smaller branches, the lateral deep femoral artery and the genicular artery; becomes the popliteal artery as it passes posterior to the knee |
| Deep Femoral Arteries | Branch of the femoral artery; gives rise to the lateral circumflex arteries |
| Popliteal Arteries | Continuation of the femoral artery posterior to the knee; branches into the anterior and posterior tibial arteries |
| Anterior Tibial Arteries | Branches from the popliteal artery; supplies blood to the anterior tibial region; becomes the dorsalis pedis artery |
| Dorsalis Pedis Arteries | Forms from the anterior tibial artery; branches repeatedly to supply blood to the tarsal and dorsal regions of the foot |
| Posterior Tibial Arteries | Branches from the popliteal artery and gives rise to the fibular or peroneal artery; supplies blood to the posterior tibial region |
| Medial Plantar Arteries | Arises from the bifurcation of the posterior tibial arteries; supplies blood to the medial plantar surfaces of the foot |
| Lateral Plantar Arteries | Arises from the bifurcation of the posterior tibial arteries; supplies blood to the lateral plantar surfaces of the foot |
| Dorsal or Arcuate Arches | Formed from the anastomosis of the dorsalis pedis artery and the medial and plantar arteries; branches supply the distal portions of the foot and digits |
| Plantar Arches | Formed from the anastomosis of the dorsalis pedis artery and the medial and plantar arteries; branches supply the distal portions of the foot and digits |
Systemic Veins
Systemic veins return blood to the right atrium. Because the blood has already passed through the systemic capillaries, it will be relatively low in oxygen concentration. In many cases, there will be veins draining organs and regions of the body with the same name as the arteries that supplied these regions, and the two often parallel one another. This is often described as a “complementary” pattern. However, there is a great deal more variability in the venous circulation than normally occurs in the arteries.
In both the neck and limb regions, there are often both superficial and deeper veins. The deeper veins generally correspond to their complementary arteries. The superficial veins do not normally have direct arterial counterparts, but in addition to returning blood, they also contribute to maintaining body temperature. When the ambient temperature is warm, more blood is diverted to the superficial veins where heat can be more easily dissipated to the environment. In colder weather, there is more constriction of the superficial veins, and blood is diverted deeper where the body can retain more of the heat.
See Figure 11.44[32] for an illustration of the major systemic veins from an anterior view.
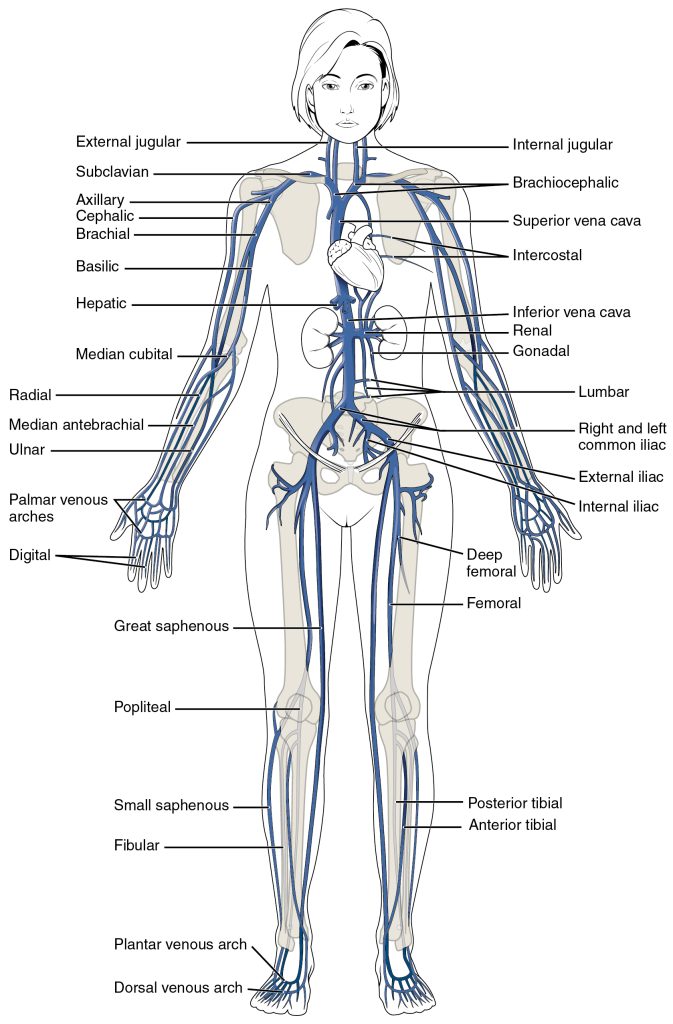
The right atrium receives all the systemic venous return. Most of the blood flows into either the superior vena cava or inferior vena cava. The superior vena cava receives blood from the head, neck, chest, shoulders, and upper limbs. The exception to this is that most venous blood flow from the coronary veins flows directly into the coronary sinus and from there directly into the right atrium. Inferior to the diaphragm, systemic venous blood from the abdominal and pelvic regions and the lower limbs enters the inferior vena cava to be returned to the right atrium.
Major Veins That Flow Into the Superior Vena Cava
The superior vena cava drains most of the body superior to the diaphragm. On both the left and right sides, the subclavian vein forms when the axillary vein passes through the body wall from the axillary region. It fuses with the external and internal jugular veins from the head and neck to form the brachiocephalic vein. The superior vena cava then receives blood from the brachiocephalic veins. See Figure 11.45[33] for an illustration of the veins that flow into the superior vena cava.
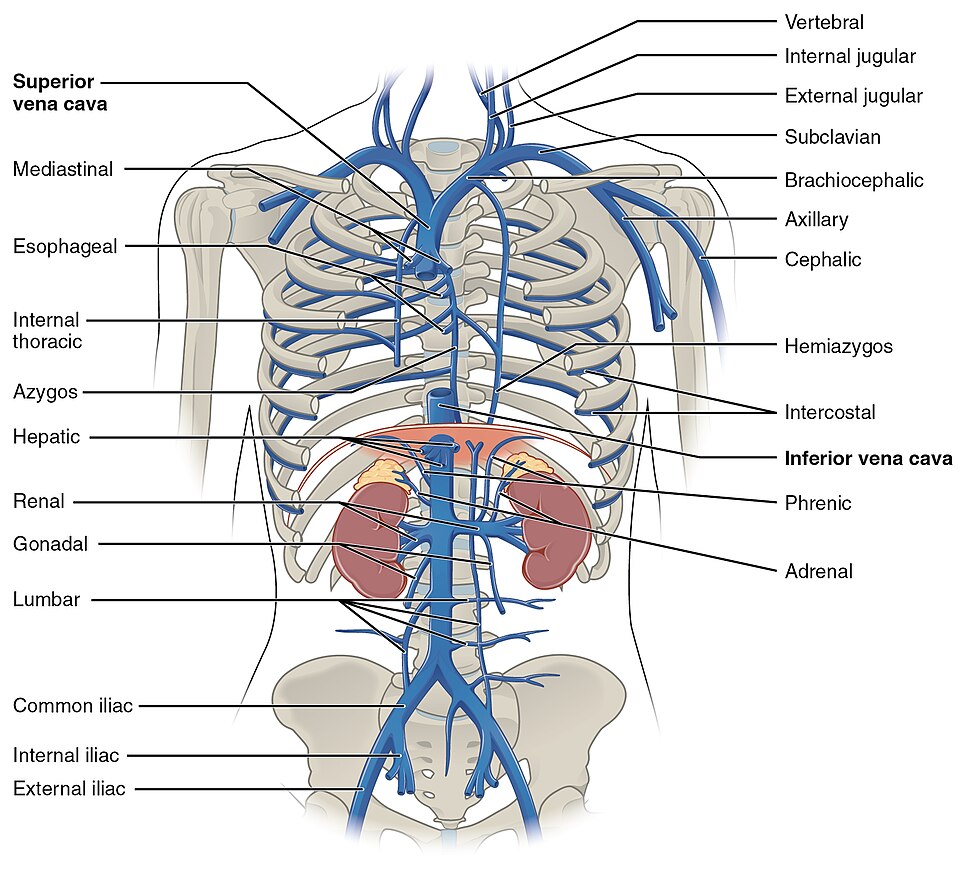
Table 11.5i summarizes the veins of the thoracic region that flow into the superior vena cava.
Table 11.5i. Major Veins of the Thoracic Region[34]
| Vessel | Description |
|---|---|
| Superior Vena Cava | Large systemic vein; drains blood from most areas superior to the diaphragm; empties into the right atrium |
| Subclavian Veins | Located deep in the thoracic cavity; formed by the axillary vein as it enters the thoracic cavity from the axillary region; drains the axillary and smaller local veins near the scapular region and leads to the brachiocephalic vein |
| Brachiocephalic Veins | Pair of veins that form from a fusion of the external and internal jugular veins and the subclavian vein; subclavian, external and internal jugulars, vertebral, and internal thoracic veins flow into it; drain the upper thoracic region and lead to the superior vena cava |
Major Veins of the Head and Neck
Blood from the brain and the superficial facial vein flow into each internal jugular vein. Blood from the more superficial portions of the head, scalp, and cranial regions, including the temporal vein and maxillary vein, flow into each external jugular vein. Although the external and internal jugular veins are separate vessels, there are anastomoses between them close to the thoracic region. Blood from the external jugular vein empties into the subclavian vein. See Figure 11.46[35] for an illustration of the internal and external jugular veins.
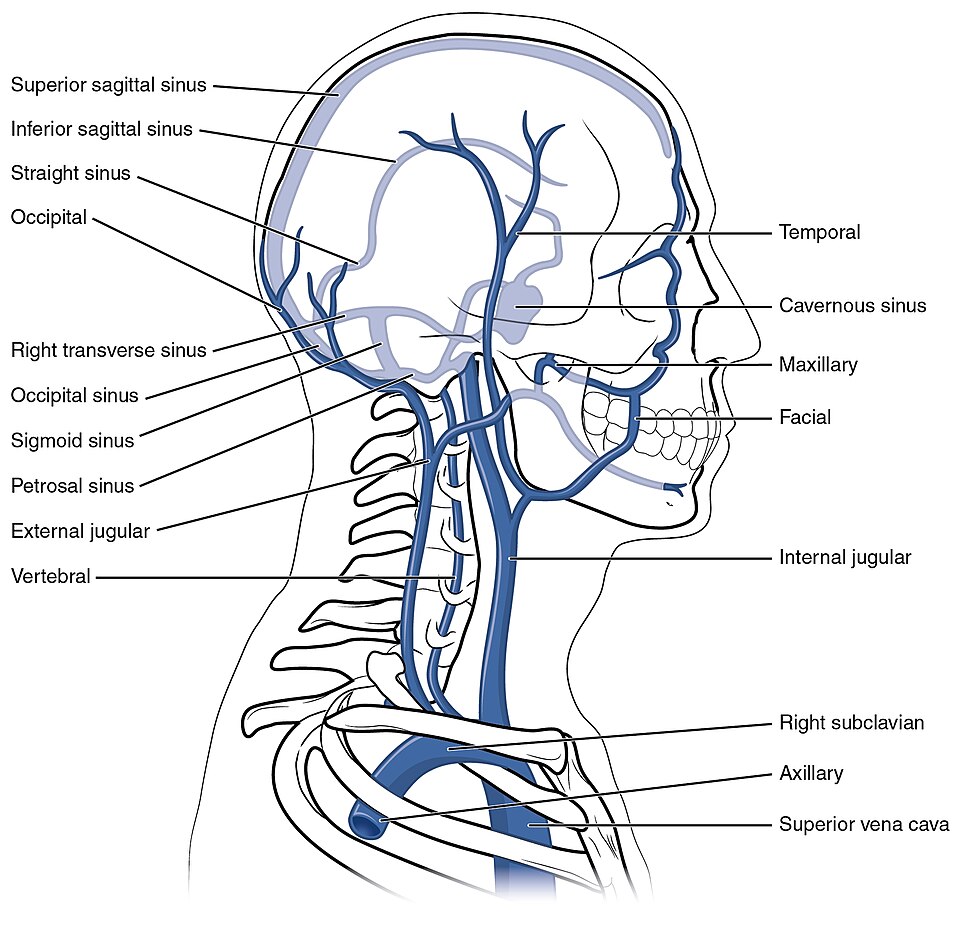
Table 11.5j. Major Veins of the Head and Neck[36]
| Vessel | Description |
|---|---|
| Internal Jugular Veins | Parallel to the common carotid artery, which is more or less its counterpart, and passes through the jugular foramen and canal; primarily drains blood from the brain, receives the superficial facial vein, and leads to the brachiocephalic vein |
| External Jugular Veins | Drains blood from the more superficial portions of the head, scalp, and cranial regions, and empties into the subclavian vein |
Major Veins Draining the Upper Limbs
The digital veins in the fingers come together in the hand to form the palmar venous arches. From here, the veins come together to form the radial vein, the ulnar vein, and the median antebrachial vein. The radial vein and the ulnar vein parallel the bones of the forearm and join together at the antebrachium to form the brachial vein, a deep vein that flows into the axillary vein in the brachium.
The median antebrachial vein parallels the ulnar vein, is more medial in location, and joins the basilic vein in the forearm. As the basilic vein reaches the antecubital region, it gives off a branch called the median cubital vein that crosses at an angle to join the cephalic vein. The median cubital vein is the most common site for drawing venous blood in humans. The basilic vein continues through the arm medially and superficially to the axillary vein.
The cephalic vein begins in the antebrachium (between the elbow and wrist) and drains blood from the superficial surface of the arm into the axillary vein. It is extremely superficial and easily seen along the surface of the biceps brachii muscle in individuals with good muscle tone and in those without excessive adipose tissue in the arms.
The subscapular vein drains blood from the subscapular region and joins the cephalic vein to form the axillary vein. As it passes through the body wall and enters the thorax, the axillary vein becomes the subclavian vein.
See Figure 11.47[37] for an illustration of the veins in the upper limb.
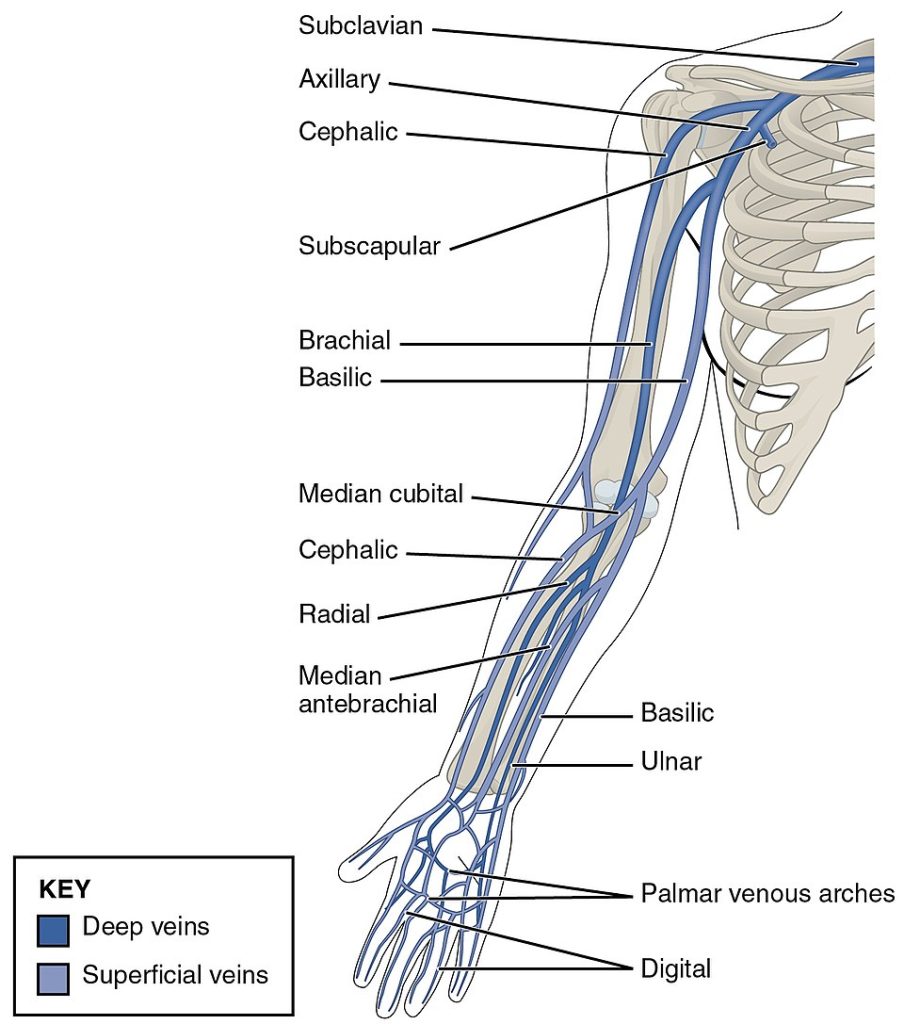
Many of the larger veins of the thoracic and abdominal region and upper limb are further represented in the flow chart in Figure 11.48.[38]
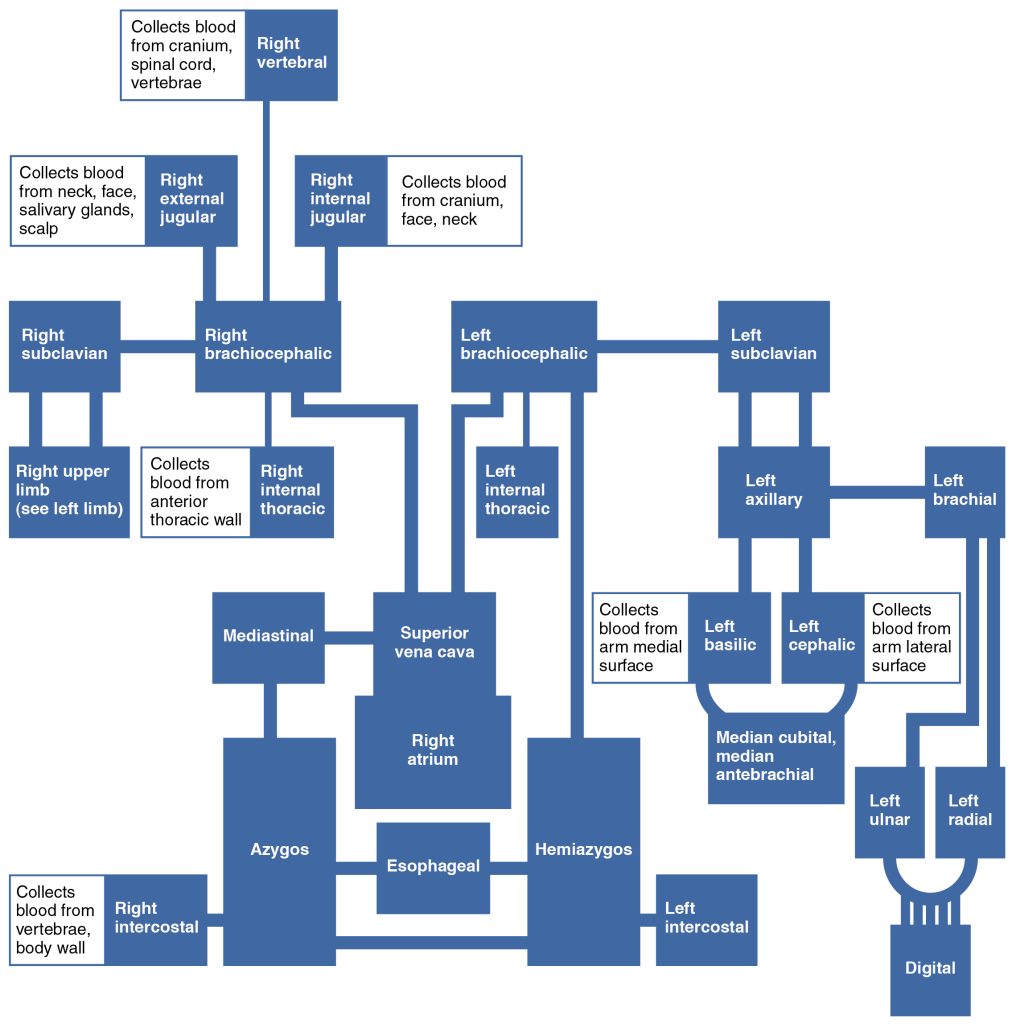
Table 11.5k summarizes the veins of the upper limbs.
Table 11.5k. Major Veins of the Upper Limbs[39]
| Vessel | Description |
|---|---|
| Digital Veins | Drain the digits and lead to the palmar arches of the hand and dorsal venous arch of the foot |
| Palmar Venous Arches | Drain the hand and digits and lead to the radial vein, ulnar veins, and median antebrachial vein |
| Radial Veins | Vein that parallels the radius and radial artery; arises from the palmar venous arches and leads to the brachial vein |
| Ulnar Veins | Vein that parallels the ulna and ulnar artery; arises from the palmar venous arches and leads to the brachial vein |
| Brachial Veins | Deeper vein of the arm that forms from the radial and ulnar veins in the lower arm; leads to the axillary vein |
| Median Antebrachial Veins | Vein that parallels the ulnar vein but is more medial in location; intertwines with the palmar venous arches; leads to the basilic vein |
| Basilic Veins | Superficial, medial vein of the arm that arises from the median antebrachial vein, intersects with the median cubital vein, parallels the ulnar vein, and continues into the upper arm; along with the brachial vein, it leads to the axillary vein |
| Median Cubital Veins | Superficial vessel located in the antecubital region that links the cephalic vein to the basilic vein in the form of a “V”; a frequent site from which to draw blood |
| Cephalic Veins | Superficial, lateral vessel in the upper arm; leads to the axillary vein |
| Subscapular Veins | Drains blood from the subscapular region and leads to the axillary vein |
| Axillary Veins | Major vein in the axillary region; drains the upper limb and becomes the subclavian vein |
Major Veins That Flow Into the Inferior Vena Cava
Most of the blood inferior to the diaphragm drains into the inferior vena cava before it is returned to the heart. The inferior vena cava parallels the abdominal aorta, where it can receive blood from abdominal veins.
Blood supply from the kidneys flows into each renal vein, the largest veins entering the inferior vena cava. A number of other smaller veins empty into the left renal vein. Each adrenal vein drains the adrenal or suprarenal glands located immediately superior to the kidneys. The right adrenal vein enters the inferior vena cava directly, whereas the left adrenal vein enters the left renal vein.
From the male reproductive organs, each testicular vein flows from the scrotum, forming a portion of the spermatic cord. Each ovarian vein drains an ovary in females. Each of these veins is generically called a gonadal vein. The right gonadal vein empties directly into the inferior vena cava, and the left gonadal vein empties into the left renal vein.
Blood supply from the liver drains into each hepatic vein and directly into the inferior vena cava. Because the inferior vena cava lies primarily to the right of the vertebral column and aorta, the left renal vein is longer, as are the left adrenal and gonadal veins. The longer length of the left renal vein makes the left kidney the primary target of surgeons removing this organ for donation.
See Figure 11.49[40] for an illustration of the veins that flow into the inferior vena cava.
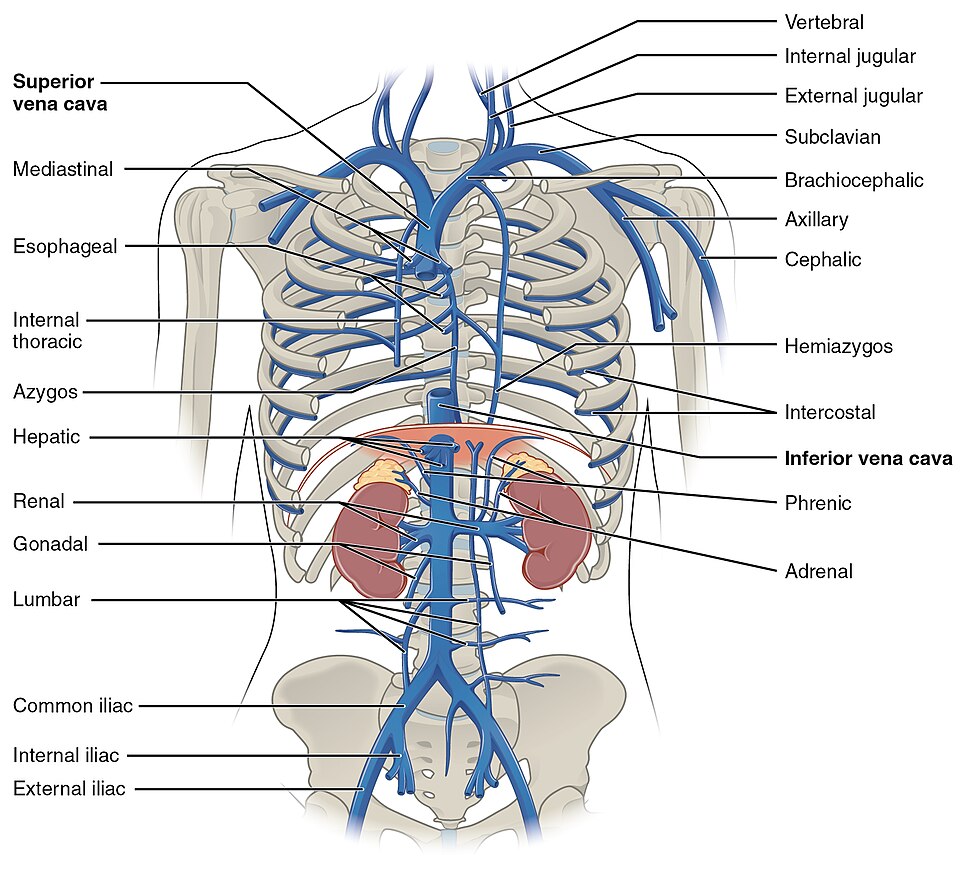
Figure 11.50[41] provides a flow chart of the veins flowing into the inferior vena cava.
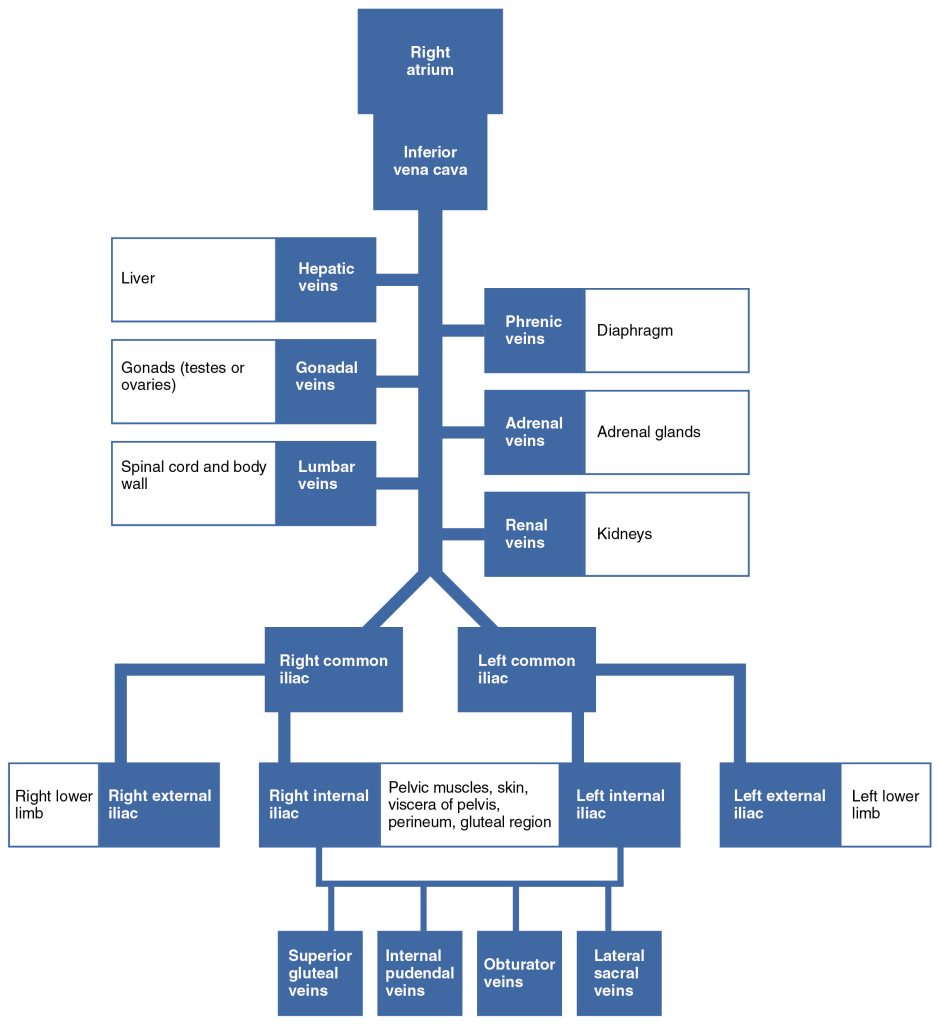
Table 11.5l summarizes the major veins of the abdominal region.
Table 11.5l. Major Veins of the Abdominal Region[42]
| Vessel | Description |
|---|---|
| Inferior Vena Cava | Large systemic vein that drains blood from areas largely inferior to the diaphragm; empties into the right atrium |
| Renal Veins | Largest vein entering the inferior vena cava; drains the kidneys and flows into the inferior vena cava |
| Adrenal Veins | Drains the adrenal or suprarenal glands; the right adrenal vein enters the inferior vena cava directly, and the left adrenal vein enters the left renal vein |
| Testicular Veins | Drains the testes and forms part of the spermatic cord; the right testicular vein empties directly into the inferior vena cava, and the left testicular vein empties into the left renal vein |
| Ovarian Veins | Drains the ovary; the right ovarian vein empties directly into the inferior vena cava, and the left ovarian vein empties into the left renal vein |
| Gonadal Veins | Generic term for a vein draining a reproductive organ; may be either an ovarian vein or a testicular vein, depending on the sex of the individual |
| Phrenic Veins | Drains the diaphragm; the right phrenic vein flows into the inferior vena cava, and the left phrenic vein empties into the left renal vein |
| Hepatic Veins | Drains systemic blood from the liver and flows into the inferior vena cava |
Major Veins Draining the Lower Limbs
The superior surface of the foot drains into the digital veins, and the inferior surface drains into the plantar veins, which flow into a complex series of anastomoses in the feet and ankles, including the dorsal venous arch and the plantar venous arch.
From the dorsal venous arch, blood supply drains into the anterior and posterior tibial veins. The anterior tibial vein drains the area near the tibialis anterior muscle and combines with the posterior tibial vein and the fibular vein to form the popliteal vein. The posterior tibial vein drains the posterior surface of the tibia and joins the popliteal vein. The fibular vein drains the muscles and skin in proximity to the fibula and also joins the popliteal vein. The small saphenous vein located on the lateral surface of the leg drains blood from the superficial regions of the lower leg and foot and flows into the popliteal vein. As the popliteal vein passes behind the knee in the popliteal region, it becomes the femoral vein. It is palpable in patients without excessive adipose tissue.
The great saphenous vein, the deep femoral vein, and the femoral circumflex vein drain into the femoral vein. The great saphenous vein is a prominent surface vessel located on the medial surface of the leg and thigh and collects blood from the superficial portions of these areas. It runs from the ankle to the groin and is the longest vein in the body. The deep femoral vein, as the name suggests, drains blood from the deeper portions of the thigh. The femoral circumflex vein forms a loop around the femur just inferior to the trochanters and drains blood from the areas in proximity to the head and neck of the femur.
As the femoral vein penetrates the body wall from the femoral portion of the leg, it becomes the external iliac vein, a large vein that drains blood from the leg to the common iliac vein. The pelvic organs and skin drain into the internal iliac vein, which forms from several smaller veins in the region. The external and internal iliac veins combine near the inferior portion of the sacroiliac joint to form the common iliac vein. In addition to blood supply from the external and internal iliac veins, the middle sacral vein drains the sacral region into the common iliac vein. Similar to the common iliac arteries, the common iliac veins come together at the level of L5 to form the inferior vena cava.
See Figure 11.51[43] for an illustration of the major veins flowing in the lower limbs.
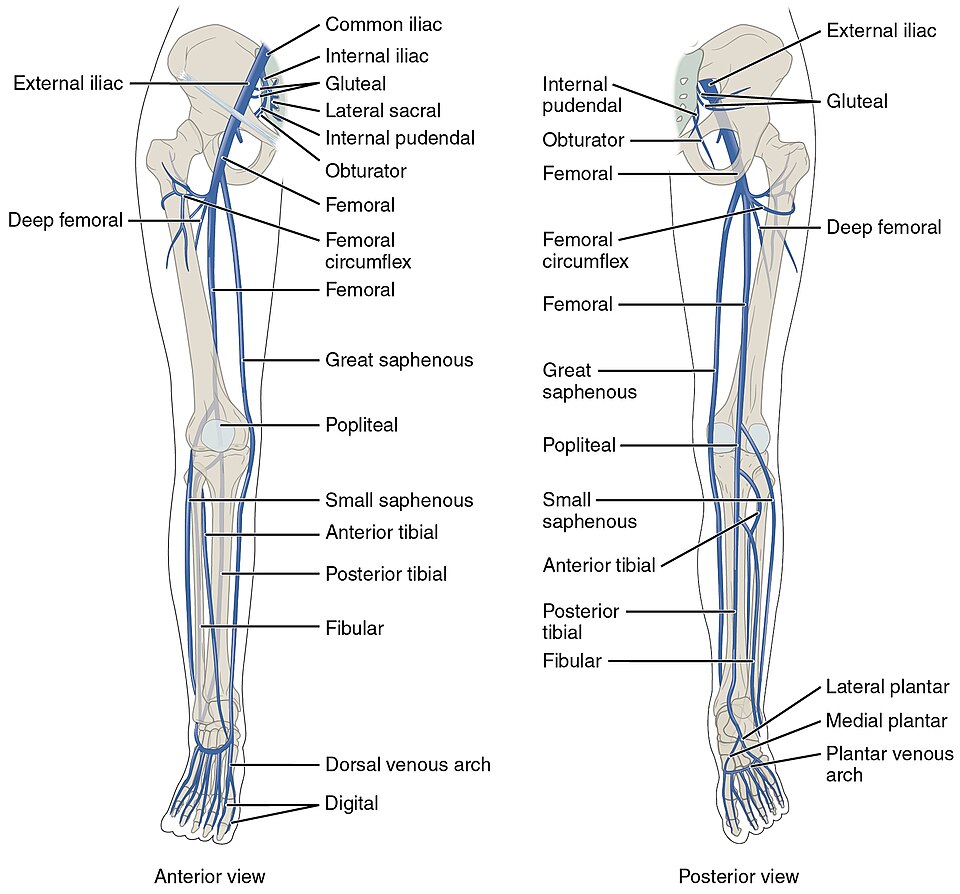
See Figure 11.52[44] for a flow chart of veins flowing into the lower limb.
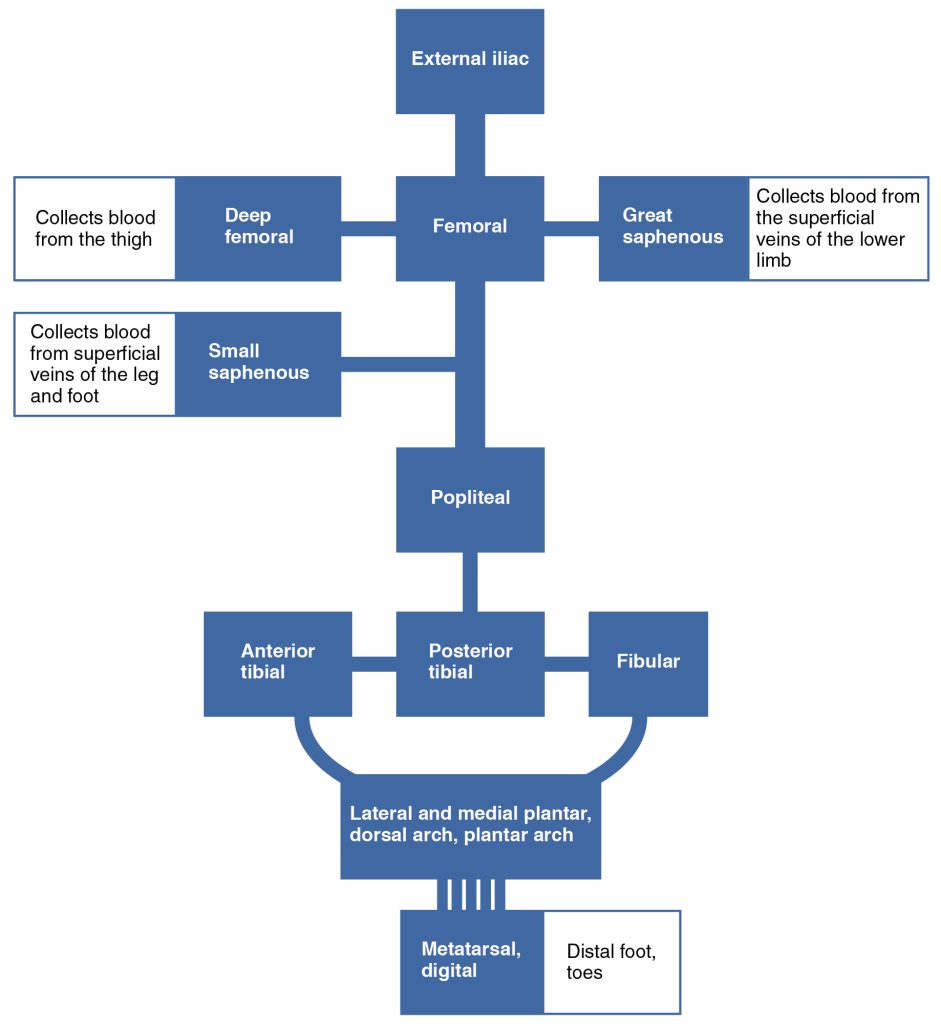
Table 11.5m summarizes the major veins of the lower limbs.
Table 11.5m. Major Veins of the Lower Limbs[45]
| Vessel | Description |
|---|---|
| Plantar Veins | Drain the foot and flow into the plantar venous arch |
| Dorsal Venous Arches | Drains blood from digital veins and vessels on the superior surface of the foot |
| Plantar Venous Arches | Formed from the plantar veins; flows into the anterior and posterior tibial veins through anastomoses |
| Anterior Tibial Veins | Formed from the dorsal venous arch; drains the area near the tibialis anterior muscle and flows into the popliteal vein |
| Posterior Tibial Veins | Formed from the dorsal venous arch; drains the area near the posterior surface of the tibia and flows into the popliteal vein |
| Fibular Veins | Drains the muscles and integument near the fibula and flows into the popliteal vein |
| Popliteal Veins | Drains the region behind the knee and forms from the fusion of the fibular, anterior, and posterior tibial veins; flows into the femoral vein |
| Great Saphenous Veins | Prominent surface vessel located on the medial surface of the leg and thigh; drains the superficial portions of these areas and flows into the femoral vein |
| Femoral Veins | Drains the upper leg; receives blood from the great saphenous vein, the deep femoral vein, and the femoral circumflex vein; becomes the external iliac vein when it enters the body wall |
| External Iliac Veins | Formed when the femoral vein passes into the body cavity; drains the legs and flows into the common iliac vein |
| Internal Iliac Veins | Drains the pelvic organs and integument; formed from several smaller veins in the region; flows into the common iliac vein |
| Middle Sacral Vein | Drains the sacral region and flows into the left common iliac vein |
| Common Iliac Veins | Flows into the inferior vena cava at the level of L5; drains the sacral region; formed from the union of the external and internal iliac veins near the inferior portion of the sacroiliac joint |
Hepatic Portal System
The liver is a complex biochemical processing plant. It processes nutrients absorbed by the digestive system; produces plasma proteins, clotting factors, and bile; and disposes of worn-out cell components and waste products. Instead of entering the circulation directly, absorbed nutrients and certain wastes (for example, materials produced by the spleen) travel to the liver for processing via the hepatic portal system. See Figure 11.53[46] for an illustration of the hepatic portal system.
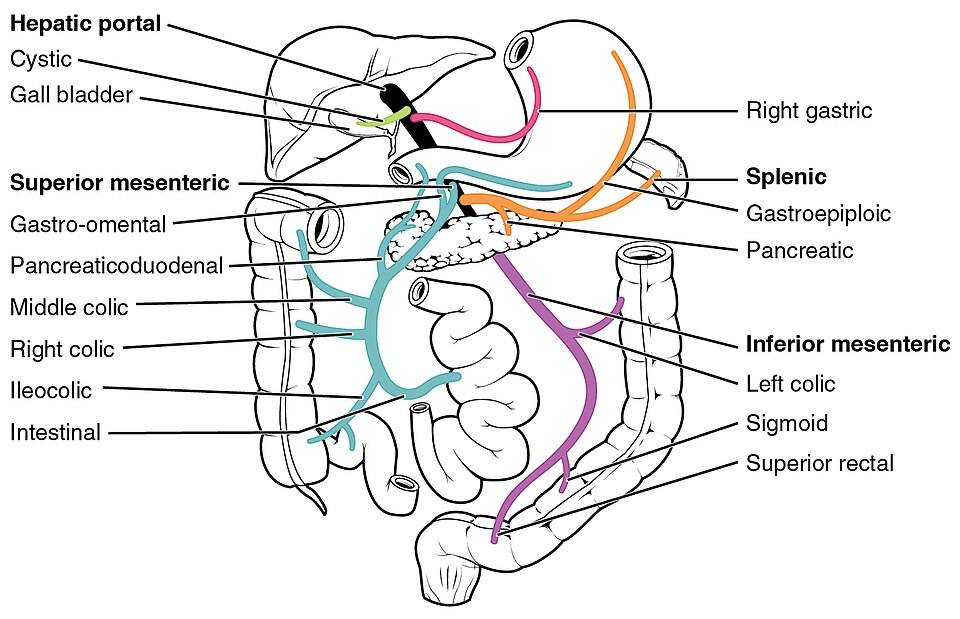
Portal systems begin and end in capillaries. In this case, the initial capillaries from the stomach, small intestine, large intestine, and spleen lead to the hepatic portal vein and end in specialized capillaries within the liver, the hepatic sinusoids. The hepatic portal vein delivers materials from these digestive and circulatory organs directly to the liver for processing.
Because of the hepatic portal system, the liver receives its blood supply from two different sources: from normal systemic circulation via the hepatic artery and from the hepatic portal vein. The liver processes the blood from the portal system to remove certain wastes and excess nutrients, which are stored for later use. This processed blood, as well as the systemic blood that came from the hepatic artery, exits the liver via the right, left, and middle hepatic veins, and flows into the inferior vena cava.
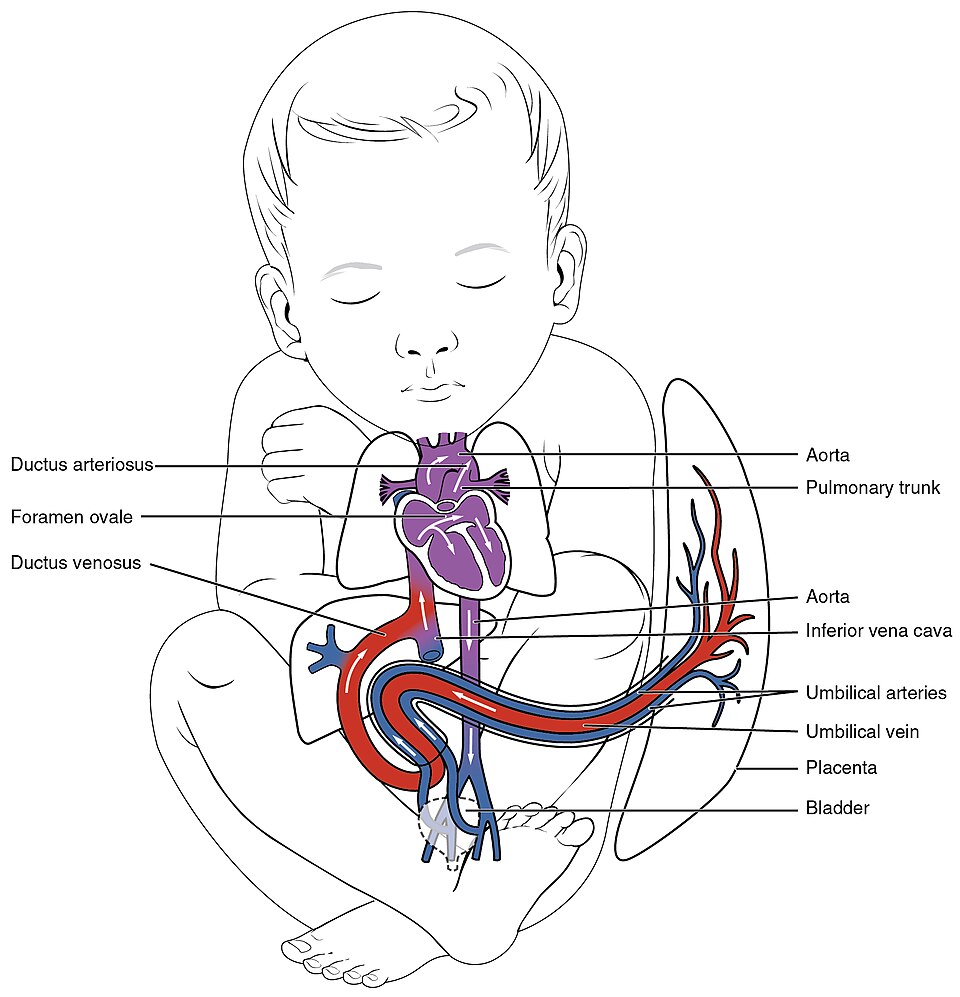
Fetal Circulation
In a developing embryo, the heart develops enough by post-fertilization Day 21 to begin beating. Circulation patterns are clearly established by the fourth week of embryonic life. It is critical to the survival of the developing human that the circulatory system forms early to supply the growing tissue with nutrients and gases and to remove waste products. As the embryo grows within the mother’s uterus, its requirements for nutrients and gas exchange also grow. The placenta (a circulatory organ unique to pregnancy) develops jointly from the embryo and uterine wall structures to fill this need. Emerging from the placenta is the umbilical vein that carries oxygen-rich blood from the mother to the fetus.
There are three major shunts (alternate paths for blood flow) found in the fetal circulatory system. The first two shunts are critical during fetal life when gas exchange is provided by the placenta, not the fetal lungs that are compressed and filled with amniotic fluid. These shunts close shortly after birth when the newborn takes its first breaths. The third shunt persists a bit longer but becomes nonfunctional once the umbilical cord is severed. The three shunts are as follows:
- The ductus venosus is a temporary blood vessel that branches from the umbilical vein, allowing much of the freshly oxygenated blood from the mother and the placenta to bypass the immature fetal liver to flow directly to the fetal inferior vena cava and into the heart, where it is pumped into fetal circulation. The ductus venosus closes slowly during the first weeks of infancy and degenerates to become the ligamentum venosum.
- The foramen ovale is an opening in the interatrial septum that allows blood to flow from the right atrium to the left atrium and bypass the lungs because they are not required for oxygenation. A valve associated with this opening prevents backflow of blood during the fetal period. After childbirth when the newborn begins to breathe, blood pressure in the atria increases, and this shunt closes. The fossa ovalis remains in the interatrial septum after birth, marking the location of the former foramen ovale.
- The ductus arteriosus is a short, muscular vessel that connects the pulmonary trunk to the aorta, diverting most of the blood pumped from the right ventricle into the aorta. A small amount of blood reaches the fetal lungs to supply the developing lung tissue. When a newborn takes their first breath, the lungs expand and the pressure within the lungs drops dramatically, causing the pulmonary vessels to expand. As the amount of oxygen increases, the smooth muscles in the wall of the ductus arteriosus constrict, sealing off the passage. Eventually, the muscular and endothelial components of the ductus arteriosus degenerate, leaving only the connective tissue component of the ligamentum arteriosum.
Two umbilical arteries carry oxygen-depleted fetal blood, including wastes and carbon dioxide, to the placenta. Remnants of the umbilical arteries remain in the adult.
See Figure 11.54[47] for an illustration of fetal circulation with oxygen-rich blood received from the placenta.
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2101_Blood_Flow_Through_the_Heart” by OpenStax College is licensed under CC BY 3.0 ↵
- “2102_Comparison_of_Artery_and_Vein” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2103_Muscular_and_Elastic_Artery_Arteriole” by OpenStax College is licensed under CC BY 3.0 ↵
- “2106_Large_Medium_Vein_Venule” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- This image is derived from "Blood_vessels-en" by Kelvinsong and is licensed under CC BY-SA 3.0. ↵
- “2109_Systemic_Blood_Pressure” by OpenStax College is licensed under CC BY 3.0 ↵
- “Blausen_0092_BloodPressureFlow” by Blausen.com staff (2014). “Medical gallery of Blausen Medical 201” is licensed under CC BY 3.0 ↵
- “2114_Skeletal_Muscle_Vein_Pump” by OpenStax College is licensed under CC BY 3.0 ↵
- “2141_CircSyst_vs_OtherSystemsN” by OpenStax College is licensed under CC BY 3.0 ↵
- “2119_Pulmonary_Circuit” by OpenStax College is licensed under CC BY 3.0 ↵
- “2119_Pulmonary_Circuit” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2120_Major_Systemic_Artery” by OpenStax College is licensed under CC BY 3.0 ↵
- “2121_Aorta” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2122_Common_Carotid_Artery” by OpenStax College is licensed under CC BY 3.0 ↵
- “2123_Arteries_of_the_Brain” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2124_Thoracic_Abdominal_Arteries” by OpenStax College is licensed under CC BY 3.0 ↵
- “2125_Thoracic_Abdominal_Arteries_Chart” by OpenStax College is licensed under CC BY 3.0 ↵
- “2126_Iliac_Artery_Branches_Chart” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2127_Thoracic_Upper_Limb_Arteries” by OpenStax College is licensed under CC BY 3.0 ↵
- “2128_Thoracic_Upper_Limb_Arteries_Chart” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2129ab_Lower_Limb_Arteries_Anterior_Posterior” by OpenStax College is licensed under CC BY 3.0 ↵
- “2130_Lower_Limb_Arteries_Chart” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2131_Major_Systematic_Veins” by OpenStax College is licensed under CC BY 3.0 ↵
- “2132_Thoracic_Abdominal_Veins” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2133_Head_and_Neck_Veins” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2134_Thoracic_Upper_Limb_Veins” by OpenStax College is licensed under CC BY 3.0 ↵
- “2135_Veins_Draining_into_Superior_Vena_Cava_Chart” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2132_Thoracic_Abdominal_Veins” by OpenStax College is licensed under CC BY 3.0 ↵
- “2140_FlowChart_Veins_into_VenaCava” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2136ab_Lower_Limb_Veins_Anterior_Posterior” by OpenStax College is licensed under CC BY 3.0 ↵
- “2137_Lower_Limb_Veins_Chart” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2138_Hepatic_Portal_Vein_System” by OpenStax College is licensed under CC BY 3.0 ↵
- “2139_Fetal_Circulation” by OpenStax College is licensed under CC BY 3.0 ↵
A blood vessel that carries blood away from the heart.
The smallest arteries.
The smallest blood vessels in the body, where the exchange of oxygen, nutrients, waste products, and other substances occurs between the blood and surrounding tissues.
Small blood vessels that receive blood from capillaries and transport it into larger veins, beginning the return flow of blood back to the heart.
Vessels that bring blood back to the heart.
A hollow central passageway through which blood flows.
The three distinct layers that make up the walls of blood vessels.
Composed of smooth epithelial and connective tissue layers.
The middle layer of the vessel wall.
Decreases blood flow as the smooth muscle in the walls of the tunica media contracts, making the lumen narrower and increasing blood pressure.
Increases blood flow as the smooth muscle relaxes, allowing the lumen to widen and blood pressure to drop.
A sheath of connective tissue composed primarily of collagenous fibers.
Arteries closest to the heart have the thickest walls, containing a high percentage of elastic fibers in all three of their tunics.
A medium-sized artery that contains a thick layer of smooth muscle, allowing it to regulate blood flow by constricting or dilating.
A very small artery that leads to a capillary.
A microscopic vessel that supplies blood to the tissues.
The process of delivering blood to the body’s tissues and organs to supply oxygen and nutrients.
The flow of blood through the smallest blood vessels—arterioles, capillaries, and venules—where exchange of gases, nutrients, and waste products occurs between blood and tissues.
An extremely small vein, generally 8–100 micrometers in diameter.
Initiated by the contraction of the ventricles of the heart and refers to the movement of blood through a vessel, tissue, or organ.
The force exerted by blood on the walls of the blood vessels or the chambers of the heart.
The higher number in a blood pressure reading; it measures the pressure in the arteries when the heart contracts and pumps blood.
The lower number in a blood pressure reading; it measures the pressure in the arteries when the heart is resting between beats.
The ability to expand or stretch.
Anything that slows blood or counteracts blood flow.
Low blood volume.
Excessive blood volume.
A measure of a fluid’s thickness or resistance to flow.
The expansion and recoiling of an artery as blood is pumped through it with each heartbeat; it can be felt manually or measured electronically.
Helps the lower-pressure veins counteract the force of gravity, increasing pressure to return blood to the heart.
A mechanism where pressure changes in the thoracic cavity during breathing help move blood toward the heart through the veins.
A large artery.
A large artery that carries blood out away from the right ventricle.
The blood vessel that carries deoxygenated blood from the right ventricle of the heart to the lungs for oxygenation.
Tiny blood vessels surrounding the alveoli in the lungs where the exchange of oxygen and carbon dioxide takes place between the blood and the air in the lungs.
Blood vessels that carry oxygen-rich blood from the lungs back to the left atrium of the heart.
The largest artery in the body.
Moves in an upward direction.
The curved portion of the aorta, the largest artery in the body, which gives rise to major arteries that supply blood to the head, neck, and upper limbs.
The part of the aorta that extends downward from the aortic arch, carrying oxygenated blood to the chest, abdomen, and lower parts of the body.
Opening in the diaphragm that allows the aorta, the body's main artery, to pass from the thoracic cavity into the abdominal cavity.
The portion of the descending aorta located in the chest (thoracic) cavity that supplies blood to the chest wall and organs within the thorax.
The part of the descending aorta that passes through the abdominal cavity, supplying oxygenated blood to the abdominal organs, pelvis, and lower limbs.
The first major branch of the aortic arch that supplies blood to the right arm, head, and neck.
A major artery branching from the brachiocephalic artery that supplies blood to the right arm and parts of the chest and shoulder.
A major artery branching from the brachiocephalic artery that supplies oxygenated blood to the right side of the head and neck.
Branches directly from the aortic arch.
Branches directly from the aortic arch.
Supply blood to the arms, chest, shoulders, back, and central nervous system.
Divide into internal and external carotid arteries.
Supplies blood to numerous structures within the face, lower jaw, neck, esophagus, and larynx.
Major arteries that arise from the common carotid arteries and supply oxygenated blood to the brain, eyes, and other internal structures of the head.
Arteries travel through the cervical vertebrae to supply blood to the brain.
A circular network of arteries located at the base of the brain that provides collateral blood flow between the anterior and posterior cerebral circulations, helping ensure consistent blood supply to the brain.
A branch of the abdominal aorta that quickly divides into the left gastric, splenic, and common hepatic arteries to supply blood to the stomach, spleen, liver, and other abdominal organs.
A branch of the celiac trunk that supplies blood to the lower esophagus and the upper part of the stomach along its lesser curvature.
A major branch of the celiac trunk that supplies oxygenated blood to the spleen.
A branch of the celiac trunk that supplies oxygenated blood to the liver, stomach, duodenum, and pancreas.
A branch of the common hepatic artery that travels toward the liver and supplies it with oxygenated blood.
A major artery that branches from the abdominal aorta and supplies oxygenated blood to most of the small intestine and part of the large intestine.
A branch of the abdominal aorta that supplies oxygenated blood to the distal part of the large intestine, including the descending colon, sigmoid colon, and rectum.
A counterpart of a superior phrenic artery and supplies blood to the inferior surface of the diaphragm.
Supplies blood to the adrenal glands and arises near the superior mesenteric artery.
A blood vessel that branches off from the abdominal aorta and supplies oxygen-rich blood to the kidneys.
Supplies blood to the gonads, or reproductive organs, and is also described as either an ovarian artery or a testicular artery, depending upon the sex of the individual.
Supplies blood to an ovary, Fallopian tube, and the uterus and is located within the suspensory ligament of the uterus.
A paired artery that arises from the abdominal aorta and supplies oxygenated blood to the testes in males.
One of the two large arteries that branch off from the abdominal aorta, supplying blood to the pelvis and lower limbs.
A small artery that arises from the posterior surface of the abdominal aorta just before it splits into the common iliac arteries; it supplies blood to the sacrum and coccyx.
A branch of the common iliac artery that supplies blood to the pelvic organs, gluteal region, and medial thigh.
A continuation of the common iliac artery that supplies blood to the lower limbs; it becomes the femoral artery as it passes under the inguinal ligament.
A major artery that carries blood from the subclavian artery through the armpit (axilla) region to the upper limb.
Supplies blood to much of the brachial region and divides at the elbow into several smaller branches, including the deep brachial arteries, which provide blood to the posterior surface of the arm, and the ulnar collateral arteries, which supply blood to the region of the elbow.
A major artery of the forearm that runs along the thumb side, commonly used to measure the pulse at the wrist.
A major artery of the forearm that runs along the little finger side, supplying blood to the medial aspect of the forearm and hand.
Supply blood to the hand.
Supply blood to the digits.
A large artery in the thigh that supplies oxygenated blood to the lower limb.
A major branch of the femoral artery that supplies blood to the deeper muscles of the thigh.
A branch of the deep femoral artery that supplies blood to the muscles on the front and side of the thigh and the hip joint.
An artery that supplies blood to the knee joint and surrounding structures.
The main artery located behind the knee that supplies blood to the knee joint and lower leg.
Located between the tibia and fibula and supplies blood to the muscles and skin of the anterior tibial region.
An artery on the top of the foot that supplies blood to the foot and toes.
Provides blood to the muscles and skin on the posterior surface of the tibial region.
An artery that branches from the posterior tibial artery and supplies blood to the inner (medial) side of the sole of the foot.
An artery branching from the posterior tibial artery that supplies blood to the outer (lateral) side of the sole of the foot.
An arterial network on the back (dorsal) side of the foot formed mainly by the dorsalis pedis artery, which supplies blood to the foot and toes.
An arterial arch located on the sole (plantar surface) of the foot, formed mainly by the lateral plantar artery, providing blood supply to the foot’s plantar tissues.
A large vein that carries deoxygenated blood from the head, neck, upper limbs, and chest back to the right atrium of the heart.
A large vein that drains deoxygenated blood from the arms and shoulders and transports it to the superior vena cava.
A large vein formed by the union of the subclavian and internal jugular veins; it drains blood from the head, neck, and upper limbs into the superior vena cava.
A major vein that collects blood from the brain, face, and neck, and drains into the brachiocephalic vein.
A vein that drains blood from the scalp and parts of the face, eventually contributing to the formation of the external jugular vein.
A vein that drains blood from the deep parts of the face, including the maxillary region, and joins with other veins to form the retromandibular vein.
A vein that drains blood from the superficial areas of the head and neck and empties into the subclavian vein.
Veins that drain blood from the fingers and toes, returning it toward the heart.
Networks of interconnected veins located in the palm of the hand that collect blood from the fingers and hand, helping return it to the larger veins of the arm.
A vein that runs along the lateral (thumb) side of the forearm, draining blood from the hand and forearm back toward the heart.
A vein that runs along the medial (pinky) side of the forearm, returning blood from the hand and forearm to the heart.
A deep vein of the upper arm that drains blood from the arm and joins with the basilic vein to form the axillary vein.
Parallels the ulnar vein, is more medial in location, and joins the basilic vein in the forearm.
A large superficial vein on the inner side of the arm that helps drain blood from the hand and forearm and eventually joins the brachial vein to form the axillary vein.
A superficial vein located in the front of the elbow (cubital fossa) that connects the basilic and cephalic veins. It is commonly used for drawing blood (venipuncture).
A superficial vein that begins in the forearm and drains blood from the surface of the arm into the axillary vein, easily visible along the biceps muscle.
Drains blood from the subscapular region and joins the cephalic vein to form the axillary vein.
A large vein that drains blood from the upper limb and shoulder, running through the armpit (axilla) and continuing as the subclavian vein.
A large vein that carries deoxygenated blood from the lower limbs and abdominopelvic region back to the right atrium of the heart.
The vein that carries deoxygenated blood filtered by the kidneys back to the inferior vena cava.
The vein that drains blood from the adrenal (suprarenal) glands and empties into the inferior vena cava or the renal vein.
Flows from the scrotum, forming a portion of the spermatic cord.
The vein that drains blood from the ovaries and returns it to the inferior vena cava (right ovarian vein) or the left renal vein (left ovarian vein).
The vein that drains blood from the gonads (ovaries in females, testes in males) and returns it to the inferior vena cava or the left renal vein.
The vein that carries deoxygenated blood from the liver to the inferior vena cava.
Veins located in the sole (bottom) of the foot that drain blood from the foot’s tissues and return it toward the heart.
A network of veins on the top surface of the foot that drains into the anterior and posterior tibial veins.
A network of veins on the bottom surface of the foot that connects with other foot and ankle veins.
A vein that drains blood from the front (anterior) part of the lower leg (shin area) and carries it upward toward the heart, eventually joining larger veins in the leg.
A vein that drains blood from the back (posterior) part of the lower leg and foot, carrying it upward toward the heart.
A vein that drains blood from the lateral (outer) side of the lower leg and foot, returning it toward the heart.
A large superficial vein in the leg that drains blood from the foot and leg and empties into the deep venous system.
A deep vein located behind the knee that collects blood from the lower leg and drains into the femoral vein.
The longest vein in the body, running along the inner leg from the foot to the groin, where it drains into the femoral vein; it is a superficial vein used often in vein grafts for surgeries.
Drains blood from the deeper portions of the thigh.
Forms a loop around the femur just inferior to the trochanters and drains blood from the areas in proximity to the head and neck of the femur.
A large deep vein in the thigh that collects blood from the popliteal vein and the great saphenous vein, transporting it upward toward the external iliac vein and eventually back to the heart.
A large vein that drains blood from the leg to the common iliac vein.
A deep vein that drains blood from the pelvic organs and walls, joining with the external iliac vein to form the common iliac vein.
A vein that drains blood from the sacrum and coccyx, typically emptying into the left or right common iliac vein.
A large vein formed by the union of the internal and external iliac veins, which drains blood from the pelvis and lower limbs into the inferior vena cava.
A network of veins that carries nutrient-rich blood from the digestive organs and spleen to the liver for processing before it enters the general circulation.
Carries oxygen-rich blood from the mother to the fetus.
Alternative paths for blood flow.
A fetal blood vessel that shunts oxygen-rich blood from the umbilical vein directly to the inferior vena cava, bypassing the liver.
A fibrous remnant of the fetal ductus venosus found in the liver after birth.
An opening in the fetal heart that allowed blood to flow directly from the right atrium to the left atrium, bypassing the lungs before birth.
A small oval-shaped depression on the interatrial septum, marking the spot of a fetal opening called the foramen ovale.
A fetal blood vessel that connects the pulmonary artery to the aorta, allowing blood to bypass the lungs before birth. It normally closes soon after birth.
A small ligament that is the remnant of the ductus arteriosus after it closes following birth. It connects the aortic arch to the pulmonary artery.
Carry oxygen-depleted fetal blood, including wastes and carbon dioxide, to the placenta.

