11.4 Cardiac Cycle
Cardiac Cycle[1]
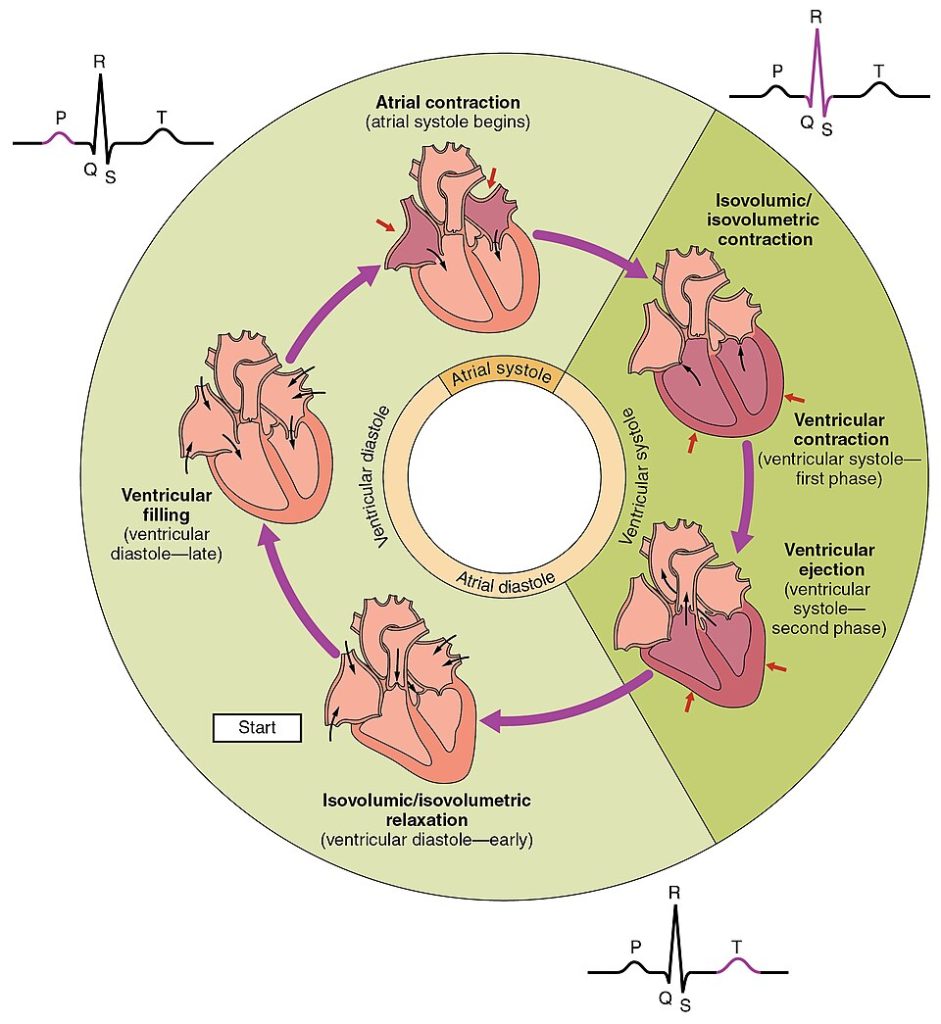
The period of time that begins with contraction of the atria and ends with ventricular relaxation is known as the cardiac cycle. One cardiac cycle consists of contraction and relaxation of the atria and contraction and relaxation of the ventricles.
Contraction of the heart is called systole. Systole pumps the blood out of the chambers. The period of relaxation that occurs as the chambers fill with blood is called diastole. Both the atria and ventricles undergo systole and diastole, and it is essential that these components be carefully regulated and coordinated to ensure blood is pumped efficiently to the body. The phases of the cardiac cycle are further described in the following subsections.
Phases of the Cardiac Cycle
At the beginning of the cardiac cycle, both the atria and ventricles are relaxed (or in diastole). Blood flows into the right atrium from the superior vena cava, the inferior vena cava, and the coronary sinus. At the same time, blood flows into the left atrium from the four pulmonary veins. During the first half of diastole, the AV valves are closed and only the atria fill. As blood volume and pressure increase in the atria, the AV valves are forced open to start ventricular filling during the second part of diastole.
Atrial Systole and Diastole
At the start of atrial systole, the ventricles are normally filled with approximately 70–80 percent of blood due to inflow during diastole. Atrial contraction, also referred to as the “atrial kick,” contributes the remaining 20–30 percent of filling for the ventricles. Contraction of the atria follows depolarization. As the atrial muscles contract from the superior portion of the atria, pressure rises within them, and blood is pumped into the ventricles through the open atrioventricular valves. Atrial systole lasts approximately 100 milliseconds (ms) and ends prior to ventricular systole, as the atrial muscle returns to diastole and blood flow into the atria resumes.
Ventricular Systole
Ventricular systole follows the depolarization of the ventricles. It may be conveniently divided into two phases, lasting a total of 270 milliseconds (ms). At the end of atrial systole and just prior to ventricular contraction, the ventricles contain approximately 130 milliliters (mL) of blood in a resting adult in a standing position. This volume is known as the end diastolic volume (EDV) or preload.
Initially, as the muscles in the ventricle contract, the pressure of the blood within the chamber rises, but it is not yet high enough to open the semilunar (pulmonary and aortic) valves and be ejected from the heart. However, blood pressure quickly rises above that of the atria that are now relaxed and in diastole. This increase in pressure causes blood to flow back toward the atria, closing the tricuspid and mitral valves. Because blood is not being ejected from the ventricles at this early stage, the volume of blood within the ventricles remains constant. Consequently, this initial phase of ventricular systole is known as isovolumetric contraction.
In the second phase of ventricular systole, the ventricular ejection phase, the contraction of the ventricular muscle raises the pressure within the ventricle to the point that it is greater than the pressures in the pulmonary trunk and the aorta. Blood is pumped from the heart as it pushes open the pulmonary and aortic semilunar valves. Pressure generated by the left ventricle will be appreciably greater than the pressure generated by the right ventricle because the existing pressure in the aorta will be so much higher. Nevertheless, both ventricles pump the same volume of blood. This quantity is referred to as stroke volume. Stroke volume will normally be in the range of 70–80 mL. Because ventricular systole begins with an end diastolic volume (EDV) of approximately 130 mL of blood, this means that there is still 50–60 mL of blood remaining in the ventricle following contraction, known as the end systolic volume (ESV).
Ventricular Diastole
Ventricular relaxation, or diastole, follows repolarization of the ventricles. It is divided into two distinct phases and lasts approximately 430 milliseconds (ms).
During the early phase of ventricular diastole, as the ventricular muscle relaxes, blood pressure within the ventricle begins to fall. When pressure within the ventricles drops below pressure in both the pulmonary trunk and aorta, blood flows back toward the heart, producing the dicrotic notch (small dip) seen in blood pressure tracings. The semilunar valves close to prevent backflow into the heart. Because the atrioventricular valves remain closed at this point, there is no change in the volume of blood in the ventricles, so the early phase of ventricular diastole is called the isovolumetric ventricular relaxation phase.
In the second phase of ventricular diastole, called late ventricular diastole, as the ventricular muscle relaxes, pressure on the blood within the ventricles drops even further. Eventually, it drops below the pressure in the atria. When this occurs, blood flows from the atria into the ventricles as it pushes open the tricuspid and mitral valves. All four chambers are in diastole, the atrioventricular valves are open, and the semilunar valves remain closed. The cardiac cycle is complete.
See Figure 11.17[2] for an illustration of the cardiac cycle.
Heart Sounds
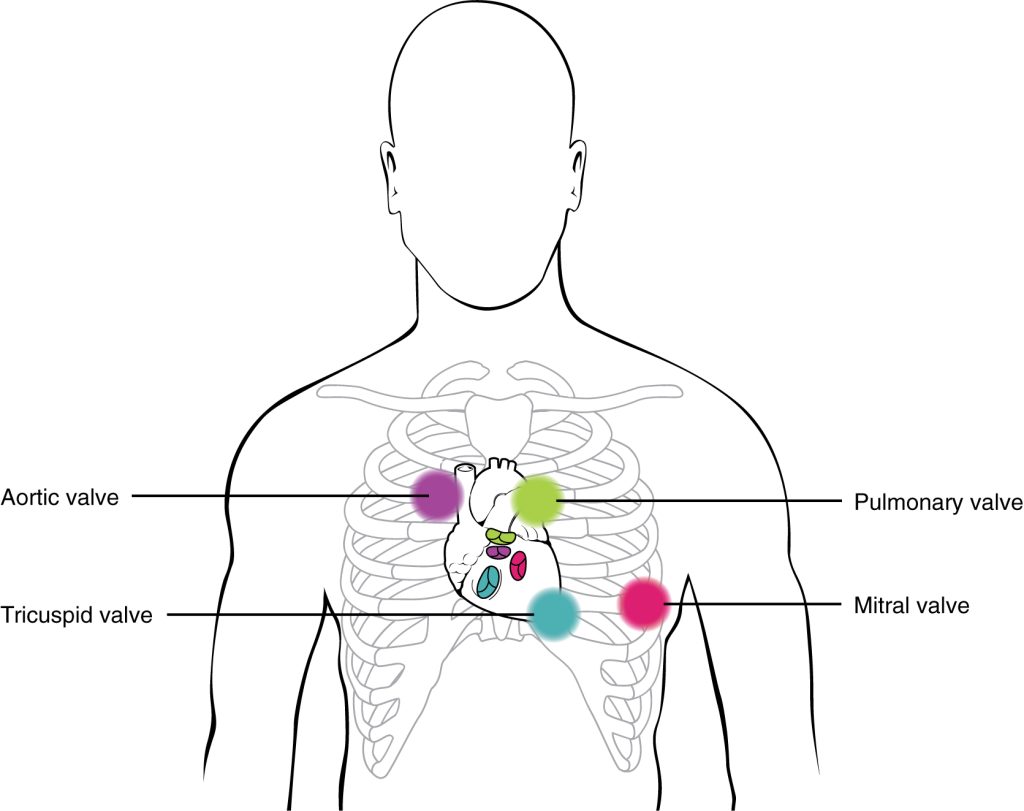
Health professionals commonly assess the status of a patient’s heart by auscultating (listening) to heart sounds using a stethoscope. In a normal, healthy heart, there are only two audible heart sounds: S1 and S2. S1 is the sound created by the closing of the atrioventricular valves during ventricular systole and is normally described as a “lub,” or first heart sound. The second heart sound, S2, is the sound of the closing of the semilunar valves during ventricular diastole and is described as a “dub.” See Figure 11.18[3] for stethoscope placement for auscultation of heart sounds over locations where valve sounds can best be heard.
The term murmur is used to describe an unusual sound coming from a heart valve that is caused by the turbulent flow of blood. Murmurs are graded on a scale of 1 to 6, with 1 being common, difficult to detect, and not serious, and 6 being the most severe.
Cardiac Output
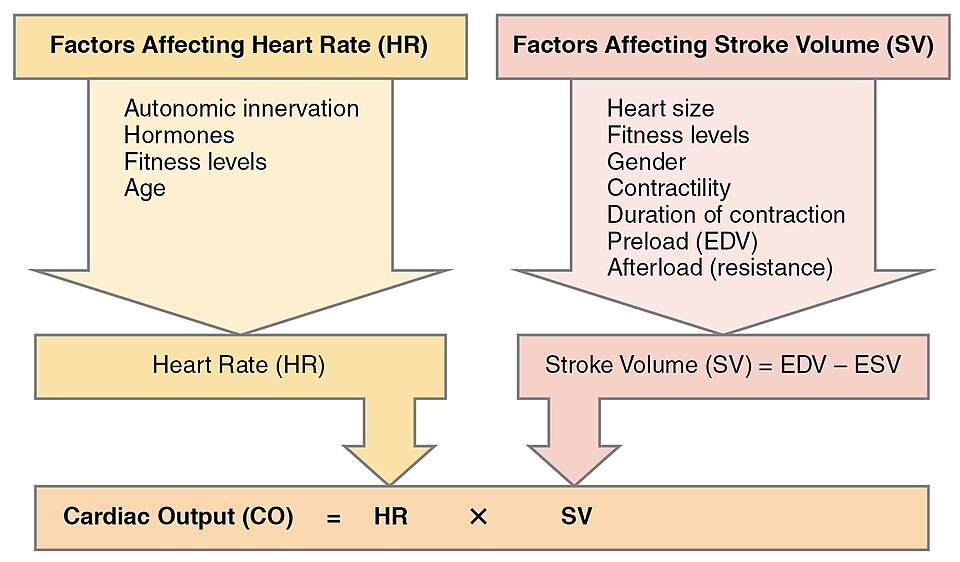
Cardiac output (CO) is the amount of blood pumped by each ventricle in one minute. To calculate this value, multiply stroke volume (SV), the amount of blood pumped by each ventricle, by heart rate (HR) per minute (or beats per minute, bpm). It can be represented mathematically by the following equation:
CO = HR × SV
The normal range for SV is 55–100 mL. The average resting HR is 75 beats per minute (bpm) with a normal range from 60–100 bpm. Using these numbers, average CO is 5.25 L/min, with a normal range of 4.0–8.0 L/min from each ventricle. Major factors influencing CO are summarized in Figure 11.19.[4]
Heart Rate
Heart rate across individuals varies considerably due to factors such as age and fitness levels. For example, a normal resting heart rate for an adult is 60-100 bpm, but a normal heart rate for a healthy newborn is 100-160 bpm. Heart rate gradually decreases until young adulthood.[5]
Abnormal Heart Rates
Bradycardia is a condition in which the resting heart rate for an adult drops below 60 bpm. If the patient is not exhibiting other symptoms, such as weakness, fatigue, dizziness, fainting, chest discomfort, palpitations, or respiratory distress, bradycardia is not considered clinically significant. In fact, trained athletes typically have heart rates below 60 bpm. However, if symptoms are present, they may indicate that the heart is not providing sufficient oxygenated blood to the tissues. Bradycardia can be caused by many factors, including side effects of medications, age, electrolyte imbalances, and a variety of medical conditions.[6]
Tachycardia is a condition in which the resting heart rate for an adult is greater than 100 bpm. Symptoms of tachycardia may include dizziness, shortness of breath, lightheadedness, heart palpitations, chest pain, or fainting (syncope). Tachycardia can be caused by a variety of factors, ranging from exercise, fever, anxiety, caffeine intake, electrolyte imbalances, side effects of medications, or underlying medical conditions.[7]
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2027_Phases_of_the_Cardiac_Cycle” by OpenStax College is licensed under CC BY 3.0 ↵
- “1914_Table_19_3_1” by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology-2e/pages/19-3-cardiac-cycle ↵
- “2031_Factors_in_Cardiac_Output” by OpenStax College is licensed under CC BY 3.0 ↵
- Charbek, E. (2024). Normal vital signs. Medscape. https://emedicine.medscape.com/article/2172054-author?form=fpf ↵
- Begum, J., & King, L. (2024). Bradycardia: Causes, symptoms, treatment. WebMD. https://www.webmd.com/heart-disease/atrial-fibrillation/bradycardia ↵
- Yale Medicine. (n.d.). Tachycardia. https://www.yalemedicine.org/conditions/tachycardia ↵
The period of time that begins with contraction of the atria and ends with ventricular relaxation.
Contraction of the heart.
The period of relaxation that occurs as the chambers fill with blood.
The electrical activation of atrial muscle cells that triggers their contraction, increasing atrial pressure and pumping blood into the ventricles through open atrioventricular valves.
The volume of blood in the ventricles at the end of ventricular filling (diastole), just before the heart contracts.
The volume of blood in the ventricles at the end of ventricular filling (diastole), just before the heart contracts.
The phase in the cardiac cycle when the ventricles contract with no change in volume because all heart valves are closed, causing a rapid increase in ventricular pressure.
The second phase of ventricular systole when the ventricles contract fully, forcing blood out through the open semilunar valves into the pulmonary trunk and aorta.
The amount of blood remaining in each ventricle after ventricular systole (contraction) and ejection of blood.
The process by which cardiac muscle cells restore their resting electrical state after depolarization, allowing the heart muscle to relax.
The early phase of ventricular diastole when the ventricles begin to relax, pressure falls, and all heart valves are closed, so no blood enters or leaves the ventricles.
Noises generated by the beating heart and the flow of blood, typically described as "lub-dub."
Used to describe an unusual sound coming from a heart valve that is caused by the turbulent flow of blood.
The amount of blood pumped by each ventricle in one minute.
The amount of blood pumped by each ventricle.
The number of heartbeats per minute, typically measured in beats per minute (bpm).
A condition in which the resting heart rate for an adult drops below 60 bpm.
A condition in which the resting heart rate for an adult is greater than 100 bpm.

