11.2 Anatomy of the Heart
Anatomy of the Heart[1]
The heart is located in the center of the thoracic cavity deep to the sternum and medially between the lungs in the space known as the mediastinum. Roughly two thirds of the heart is found left of the midline. Figure 11.1[2] shows the position of the heart within the thoracic cavity.
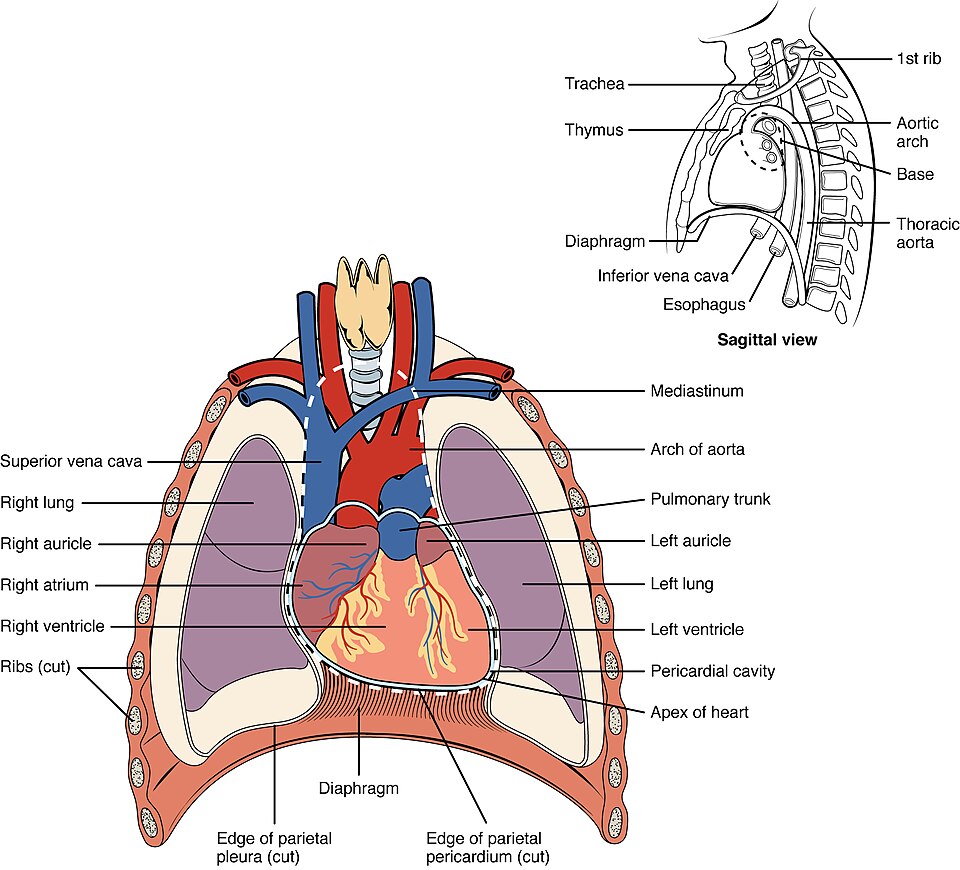
The superior surface of the heart at the widest point is called the base. The inferior tip of the heart, the apex, lies just left of the sternum. The right side of the heart is tilted anteriorly, and the left side is tilted posteriorly. The position and orientation of the heart are important to remember when placing a stethoscope on a patient’s chest and listening for heart sounds.
The heart is divided into four chambers. The two superior chambers are the right and left atria, and the two inferior chambers are the right and left ventricles.
A typical heart is approximately the size of your fist: 12 cm (5 in) in length, 8 cm (3.5 in) wide, and 6 cm (2.5 in) in thickness. The weight of a female heart is approximately 250–300 grams (9 to 11 ounces), and the weight of a male heart is approximately 300–350 grams (11 to 12 ounces).
Pericardium
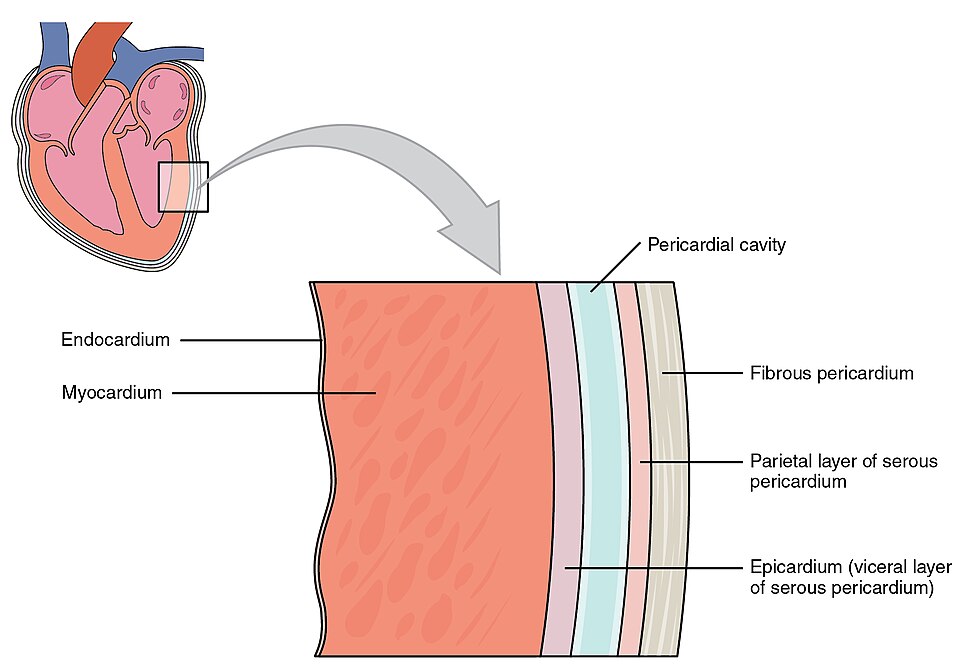
Within the mediastinum, the heart is located inside a tough double membrane sac known as the pericardium, or pericardial sac. The pericardial cavity is filled with a lubricating serous (watery) fluid that reduces friction between the heart and the pericardium during contraction.
The word pericardium literally translates to “around the heart.” It consists of two distinct layers: the sturdy outer fibrous pericardium and the inner serous pericardium. The fibrous pericardium is made of tough, dense connective tissue that protects the heart and maintains its position in the chest cavity. The more delicate serous pericardium consists of two layers: the parietal pericardium, which is fused to the fibrous pericardium, and an inner visceral pericardium, or epicardium, which is fused to the heart and is part of the heart wall. See Figure 11.2[3] for an illustration of the pericardial membranes.
Layers of the Heart Wall
The wall of the heart is composed of three layers of unequal thickness. From superficial to deep, they are the epicardium, the myocardium, and the endocardium. Refer back to Figure 11.2 for an illustration of these three layers.
Epicardium
The epicardium is the outermost layer of the heart wall. It is also the innermost layer of the serous pericardium, called the visceral pericardium.
Myocardium
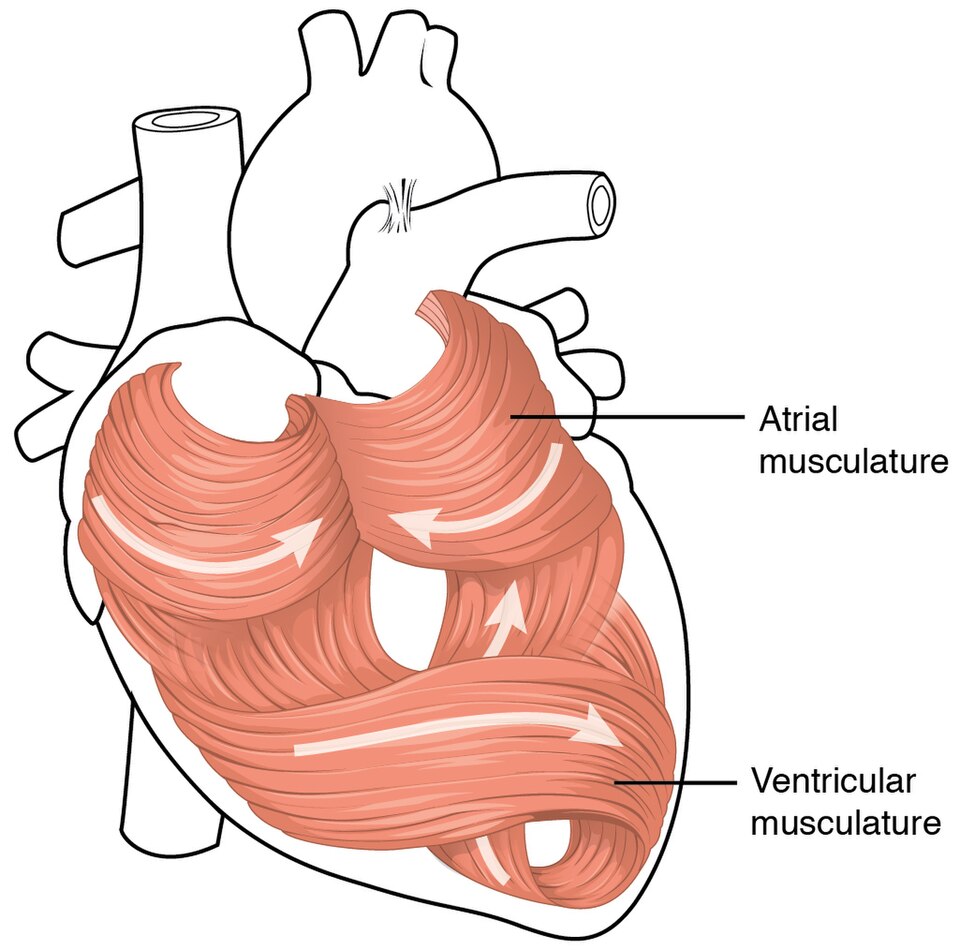
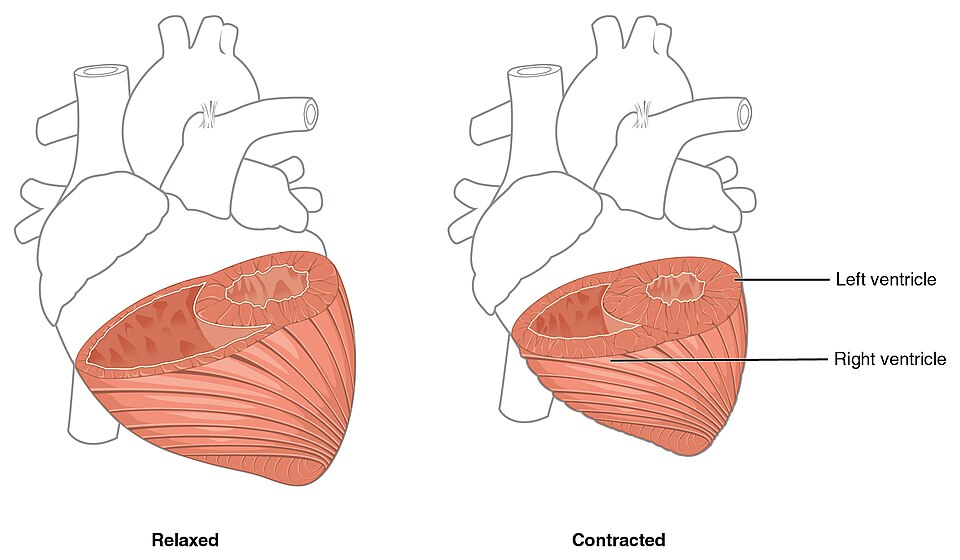
The middle and thickest layer of the heart is the myocardium, made up largely of cardiac muscle cells. It is the contraction of the myocardium that pumps blood through the heart and into the major arteries. The muscle pattern is elegant and complex, as the muscle cells swirl and spiral around the chambers of the heart. This complex swirling pattern allows the heart to pump blood more effectively than a simple linear pattern would. The muscle is reinforced with dense connective tissue called the fibrous skeleton of the heart. It includes four rings that surround the openings between the atria and ventricles and the openings to the pulmonary trunk and aorta. These rings serve as attachment points for the heart valves. The fibrous cardiac skeleton also provides an important boundary in the heart’s electrical conduction system so that the ventricles don’t contract at the same time as the atria. Heart valves are further discussed in the “Heart Valve Structure and Function” subsection. See Figure 11.3[4] for an illustration of the arrangement of the cardiac muscle.
Endocardium
The endocardium is the innermost layer of the heart wall that is joined to the myocardium with a thin layer of connective tissue. The endocardium lines the chambers where the blood circulates and covers the heart valves. It is made of simple squamous epithelium called endothelium, which is continuous with the endothelial lining of the blood vessels.
Surface Features of the Heart
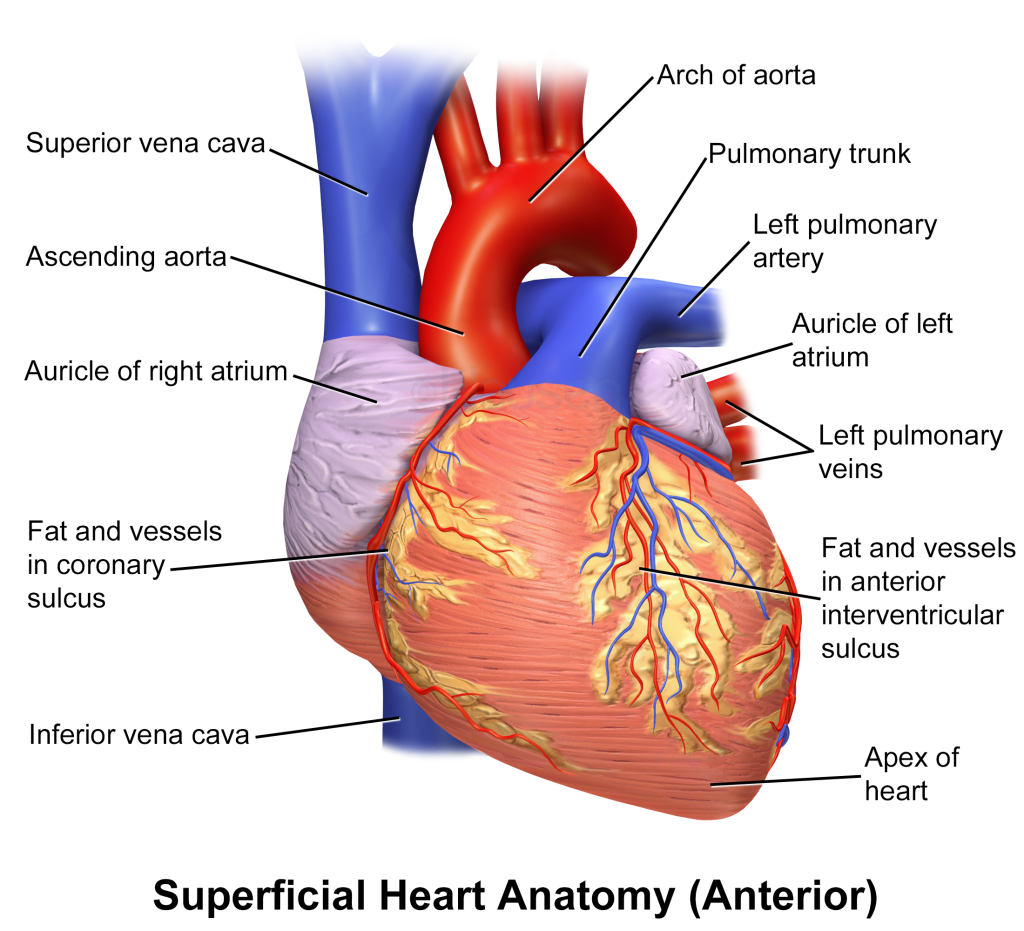
Inside the pericardium, the surface features of the heart are visible. On both the right and left sides of the heart, there is an extension of the atria visible on the superior surface called an auricle. Auricles are flaplike, thin-walled structures that can slightly expand to increase the volume of the atria, the upper chambers of the heart. It is named auricle, which means “ear-like,” because its shape resembles the external ear of a human. See Figure 11.4 for an illustration of the right and left auricles.
Also prominent is a series of fat-filled grooves, each of which is known as a sulcus (plural = sulci), along the superior surfaces of the heart. Major coronary blood vessels are located in these sulci. The deep coronary sulcus is located between the atria and ventricles. Located between the left and right ventricles are two additional sulci that are not as deep as the coronary sulcus. The anterior interventricular sulcus is visible on the anterior surface of the heart, whereas the posterior interventricular sulcus is visible on the posterior surface of the heart. See Figure 11.4[5] for an illustration of the surface features of the heart.
Chambers of the Heart
The heart consists of four chambers: two upper chambers called atria (single = atrium) and two lower chambers called ventricles (single = ventricle). The right atrium and the left atrium act as receiving chambers for blood which then contract and push blood into the lower chambers, the right ventricle and the left ventricle. The ventricles serve as the primary pumping and ejecting chambers of the heart, propelling blood to the lungs (pulmonary circulation) or to the rest of the body (systemic circulation).
The atria and ventricles are divided by septa. A septum (plural = septa) refers to a wall or partition that divides. The septa are physical extensions of the myocardium lined with endocardium. The interatrial septum (or atrial septum) is located between the right and left atria.
The interventricular septum (or ventricular septum) is located between the right and left ventricles. The interventricular septum is substantially thicker than the interatrial septum because the ventricles generate much more pressure when they contract. The septum between the atria and ventricles is known as the atrioventricular septum.
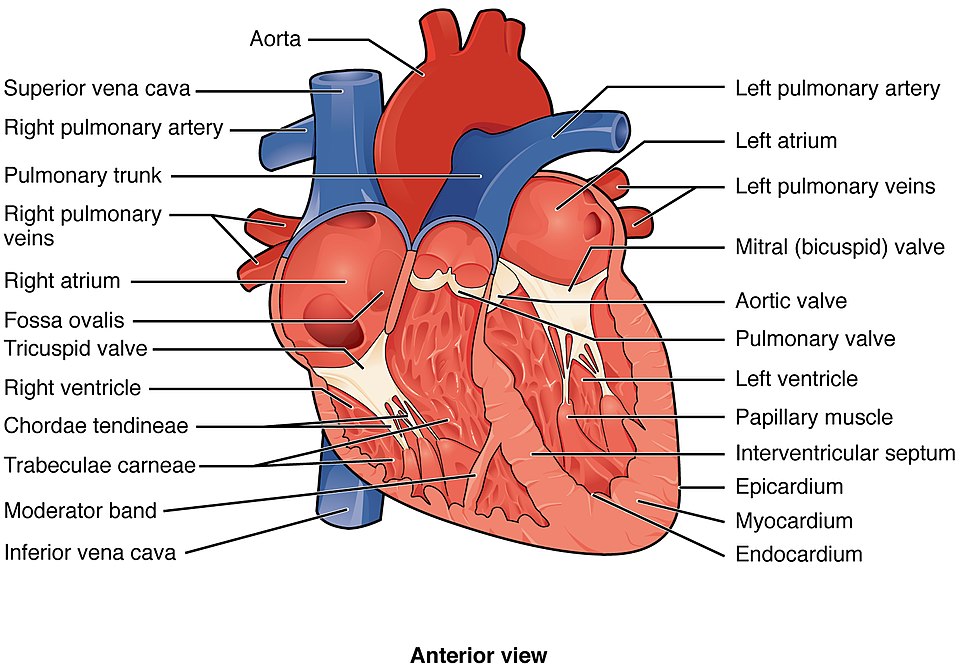
See Figure 11.5[6] for an illustration of the internal structures of the heart. Note that the interatrial septum is not visible as it is covered by the aorta and pulmonary trunk.
The atrioventricular septum has four openings that allow blood to move from the atria into the ventricles and from the ventricles into the pulmonary trunk and aorta. Located in each of these openings between the atria and ventricles is a valve, a specialized structure that ensures one-way flow of blood. Because these openings and valves structurally weaken the atrioventricular septum, the remaining tissue is reinforced with dense connective tissue called the cardiac fibrous skeleton of the heart. It includes four rings that surround the openings between the atria and ventricles and the openings to the pulmonary trunk and aorta and serve as the point of attachment for the heart valves. The cardiac skeleton also provides an important boundary in the heart’s electrical conduction system. Heart valves are further discussed in the “Heart Valve Structure and Function” subsection.
Right Atrium
The right atrium serves as the receiving chamber for deoxygenated blood returning to the heart from the body (systemic circulation). The two major systemic veins (the superior vena cava and the inferior vena cava) and the coronary sinus (a large coronary vein whose walls can’t change diameter) transport deoxygenated blood to the right atrium.
The superior vena cava receives deoxygenated blood from the head, neck, upper limbs, and the chest region. It empties into the superior portion of the right atrium. The inferior vena cava receives deoxygenated blood from the lower limbs and abdominopelvic region of the body. It empties into the right atrium below the opening of the superior vena cava. Refer back to Figure 11.4 on the “Surface Features of the Heart” for an illustration of the superior and inferior vena cavae entering the right atrium.
On the posterior surface of the right atrium is the opening of the coronary sinus. This thin-walled vessel receives deoxygenated blood from most of the coronary veins, the systemic veins that receive deoxygenated blood from the heart muscle itself.
Special Features of the Right Atrium
While most of the inner surface of the right atrium is smooth, there are a few areas that are not. A small oval-shaped depression on the interatrial septum is the fossa ovalis, which marks the former location of the foramen ovale, the opening in the fetal heart that allowed blood to flow directly from the right atrium to the left atrium and bypass pulmonary circulation. Read more about the foramen ovale in the “Fetal Circulation” subsection.
The other special features of the right atrium are prominent or rough ridges of muscle called pectinate muscles on the inner surface of the anterior right atrium. The right auricle also has pectinate muscles.
Right Ventricle
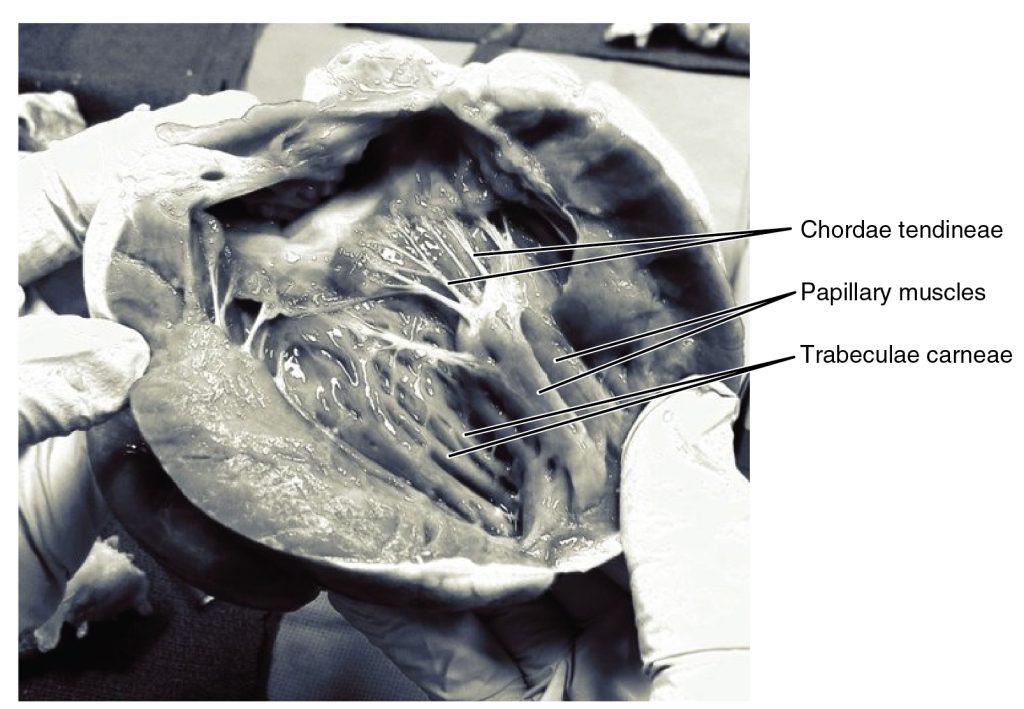
The right ventricle receives blood from the right atrium through the tricuspid valve. Each flap of the valve is attached to strong cords of connective tissue called the chordae tendineae, literally translated as “tendinous cords,” or sometimes more poetically referred to as the “heart strings.” The chordae tendineae connect each of the flaps to a papillary muscle that extends from the inferior ventricle wall.
When the myocardium of the ventricle contracts, pressure within the ventricle rises. Blood, like any fluid, flows from higher pressure to lower pressure, so in this case it moves upward toward the pulmonary trunk and the atrium. To prevent any potential backflow into the right atrium, the papillary muscles also contract, pulling on the chordae tendineae. This prevents the flaps of the valves and blood from being forced back up into the atria during ventricular contraction. See Figure 11.6[7] for a photo of the papillary muscles and chordae tendineae attached to the tricuspid valve.
When the right ventricle contracts, it ejects blood through the pulmonary valve and into the pulmonary trunk, a large artery that carries blood out away from the right ventricle. The pulmonary trunk divides into the left and right pulmonary arteries, which carry the deoxygenated blood to the lungs.
Special Features of the Right Ventricle
The walls of the right ventricle are lined with trabeculae carneae, ridges of cardiac muscle covered by endocardium. In addition to these muscular ridges, there is a band of cardiac muscle known as the moderator band, which reinforces the thin walls of the right ventricle and plays a crucial role in cardiac conduction. The moderator band crosses from the lower interventricular septum to the inferior papillary muscle. Refer back to Figure 11.5 for an illustration of the trabeculae carneae and the moderator band in the right ventricle.
Left Atrium
After oxygen is picked up and carbon dioxide is dropped off in the pulmonary capillaries of the lungs, freshly oxygenated blood returns to the left atrium of the heart through the four pulmonary veins. Most blood flows passively into the heart while both the atria and ventricles are relaxed, but toward the end of the ventricular relaxation period, the left atrium will contract, pumping blood into the ventricle. This atrial contraction accounts for approximately 20 percent of ventricular filling.
While the left atrium does not contain pectinate muscles, it does have an auricle that includes these pectinate ridges.
Left Ventricle
Oxygenated blood flows into the left ventricle through the mitral (bicuspid) valve. The mitral valve is connected to papillary muscles by chordae tendineae. There are two papillary muscles in the left ventricle—the anterior and posterior—as opposed to three papillary muscles in the right ventricle. When the myocardium of the left ventricle contracts, it pushes blood up and through the aortic valve and into the aorta.
Although the ventricles on the right and left sides of the heart pump the same volume of blood per contraction, the myocardium of the left ventricle is much thicker and well-developed than the myocardium in the right ventricle. This is because the left ventricle has to generate more pressure to pump blood through the entire body (systemic circulation). The right ventricle does not need to generate as much pressure, as it only has to pump blood to the lungs and back (pulmonary circulation). See Figure 11.7[8] for an illustration of the difference in thickness between the right and left ventricles.
Heart Valve Structure and Function
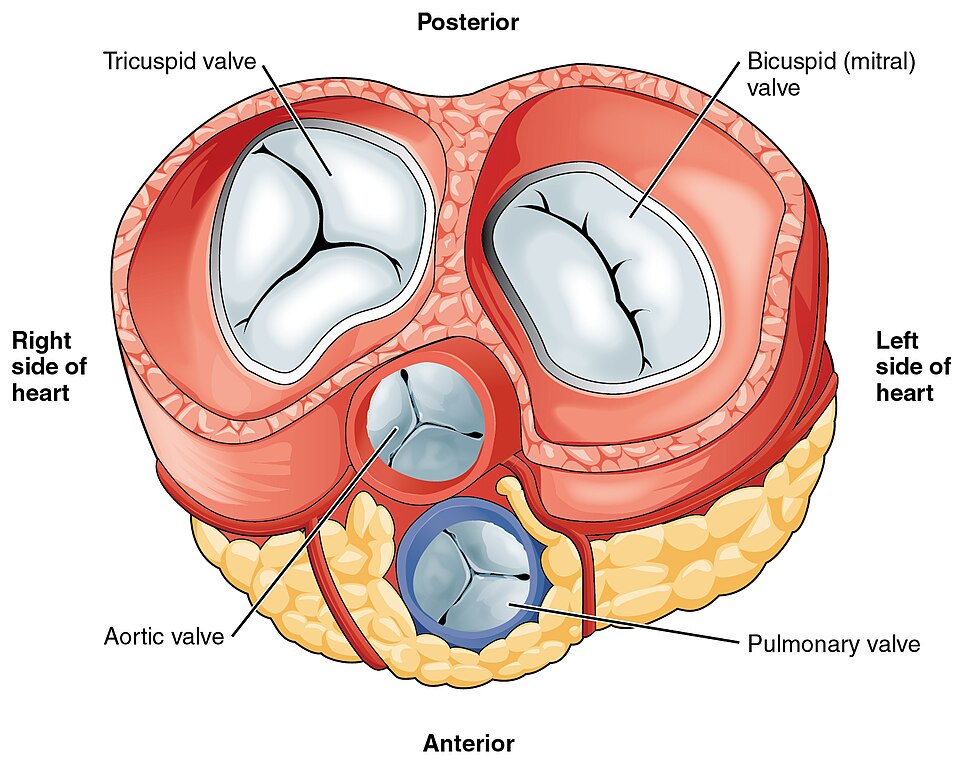
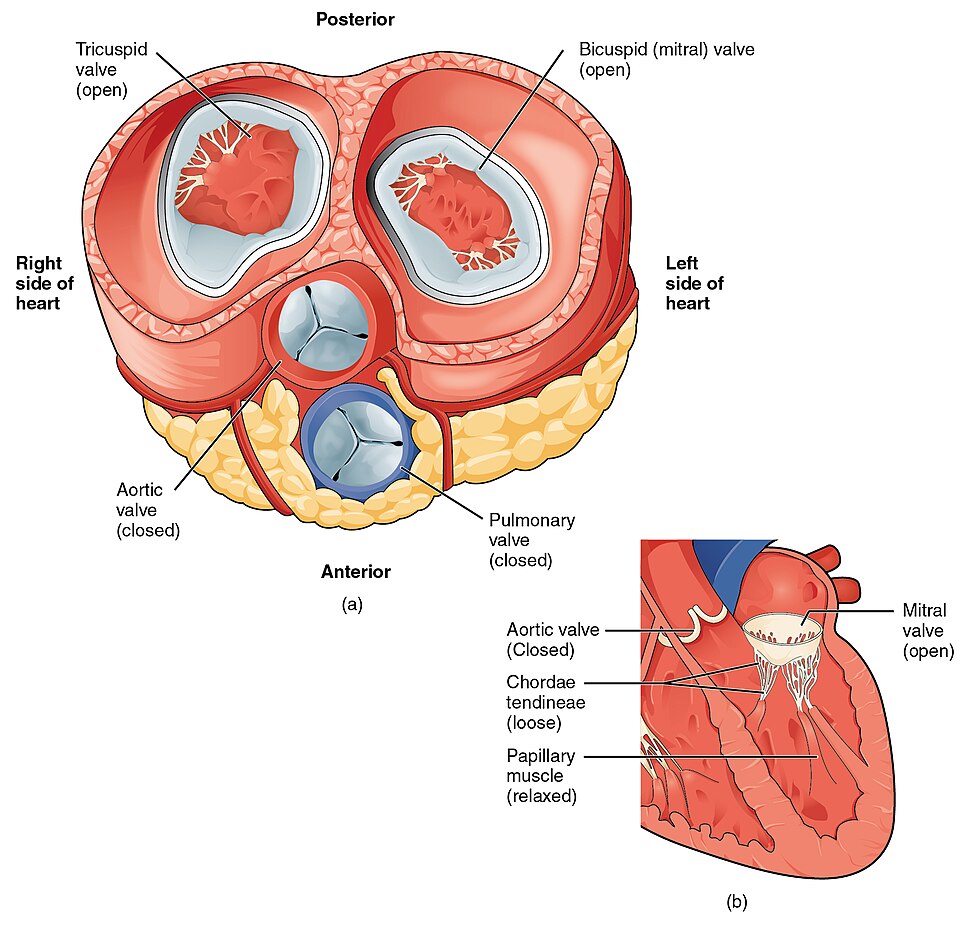
There are two sets of valves found in the heart, the atrioventricular (AV) valves and the semilunar valves. The valves ensure that blood flows in one direction through the heart. See Figure 11.8[9] for an illustration of the heart valves.
Atrioventricular (AV) Valves
The two one-way valves between the atria and ventricles are known as atrioventricular valves. The AV valve on the right side of the heart is called the tricuspid valve, and the one on the left side is the mitral (bicuspid) valve. The first heartbeat sound (“lub”) is caused by the closing of the AV valves.
When the ventricles begin to contract, pressure within the ventricles rises and blood flows toward the area of lowest pressure, which is initially in the atria. This backflow causes the cusps of the tricuspid and mitral (bicuspid) valves to close.
Tricuspid Valve
The tricuspid valve is located between the right atrium and the right ventricle and is also known as the right atrioventricular valve. It consists of three leaflets (flaps) made of endocardium reinforced with additional connective tissue. The flaps are connected by chordae tendineae to the papillary muscles, which control the opening and closing of the valves.
Mitral (Bicuspid) Valve
The mitral valve, also called the bicuspid valve or the left atrioventricular valve, is located between the left atrium and left ventricle. Structurally, this valve consists of two cusps, compared to the three cusps of the tricuspid valve. The two cusps of the mitral valve are attached by chordae tendineae to two papillary muscles that project from the wall of the ventricle.
Semilunar Valves
The valves at the openings in the heart that lead to the pulmonary trunk and the aorta are known generically as semilunar valves. The semilunar valves are composed of three flaps of endothelium reinforced with connective tissue but lack the chordae tendineae and papillary muscles associated with the atrioventricular valves. Instead, they consist of pocket-like folds of endocardium reinforced with additional connective tissue. These flaps resemble a half-moon and that is why they’re called semilunar (semi = half, lunar = moon) valves. When the ventricles relax and the change in pressure forces the blood toward the ventricles, the blood presses against these cusps and seals the openings. The two semilunar valves are the pulmonary valve and the aortic valve.
Pulmonary Valve
The pulmonary valve, also known as the pulmonic valve, pulmonary semilunar valve, or the right semilunar valve, emerges from the right ventricle at the base of the pulmonary trunk. When the right ventricle relaxes, the pressure differential causes blood to flow backward from the pulmonary trunk. This flow of blood fills the pocket-like flaps of the pulmonary valve, causing the valve to close and produce an audible sound that can be heard as the second sound in the heartbeat (“dub”).
Aortic Valve
The aortic valve, also called the aortic semilunar valve or the left semilunar valve, is at the base of the aorta and prevents backflow of blood from the aorta. When the ventricle relaxes and blood attempts to flow back into the left ventricle from the aorta, blood will fill the cusps of the valve, causing it to close and produce an audible sound that is also part of the “dub” sound in the heartbeat.
See Figure 11.9[10] for an illustration of blood flow from the left atrium to the left ventricle. When the mitral valve is open, it allows blood to move from the left atrium to the left ventricle. The aortic valve is closed to prevent backflow of blood from the aorta to the left ventricle.
View this supplementary Wisc-Online learning activity[11] on the anatomy of the heart:
The Anatomy of the Heart (Video)
View this supplementary YouTube video[12] on heart contraction and blood flow:
Heart Contraction and Blood Flow Video Animation
Cardiac Muscle Cells
Cardiomyocytes (cardiac muscle cells) share a few characteristics with both skeletal muscle and smooth muscle, but they also have some unique properties of their own. One of these unique characteristics is its ability to initiate an electrical impulse that spreads rapidly from cell to cell to trigger contraction. This property is known as autorhythmicity. However, even though cardiac muscle has autorhythmicity, heart rate is influenced by the endocrine and nervous systems.
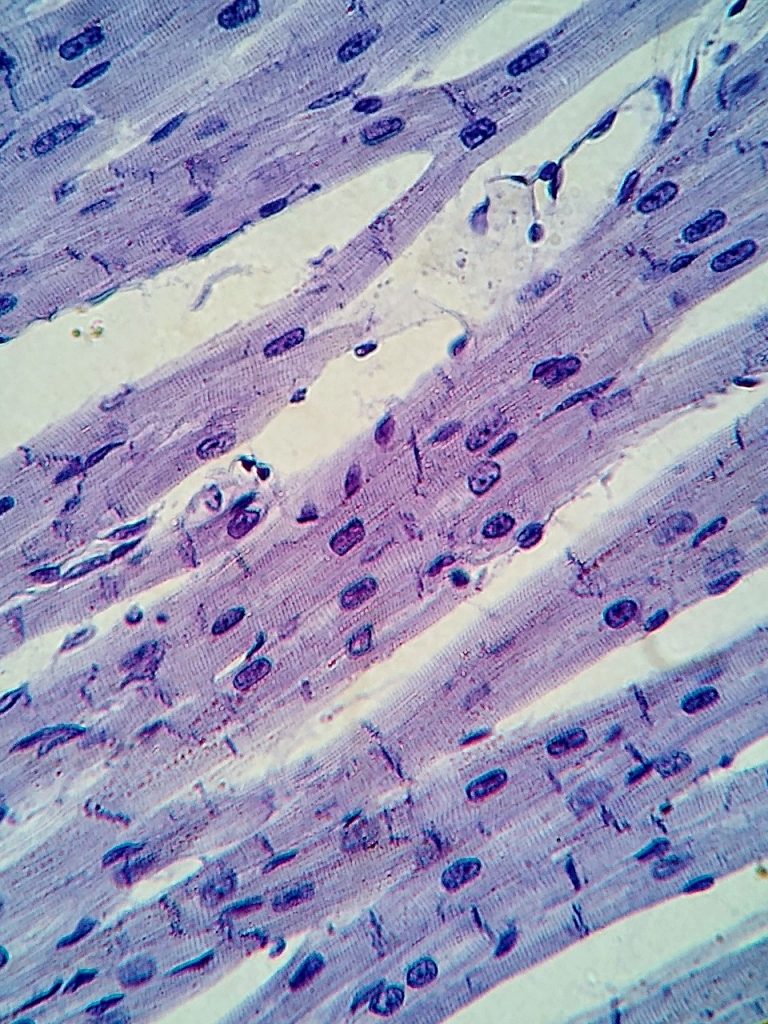
Structure of Cardiac Muscle
Cardiomyocytes are considerably shorter with much smaller diameters compared to the long cylinders of skeletal muscle fibers. Like skeletal muscle, cardiac muscle is also striated. Mitochondria are plentiful, providing energy for the continuous contractions of the heart. Typically, cardiomyocytes have a single, central nucleus, but two or more nuclei may be found in some cells.
Cardiomyocytes branch freely. A junction between two adjoining cells is marked by a structure called an intercalated disc, which helps coordinate the synchronized contraction of the heart muscle so that cells contract together to pump the blood. See Figure 11.10[13] for an illustration of cardiac muscle cells.
Repair and Replacement of Cardiac Muscle Cells
If an individual has a myocardial infarction (commonly known as a heart attack), cardiac muscle cells are damaged and can die from lack of oxygenated blood flow. Damaged cardiac muscle cells have extremely limited abilities to repair or replace themselves. Dead cardiac muscle cells are replaced by patches of scar tissue. Research indicates that some stem cells remain within the heart that continue to divide and potentially replace dead cells, but these newly formed cells are rarely as functional as the original cells, which reduces cardiac function. If future research can unlock the mechanism that generates new cardiac muscle cells and restores full mitotic capabilities, the prognosis for heart attack survivors will be greatly enhanced.[14]
Pulmonary and Systemic Circulation of Blood
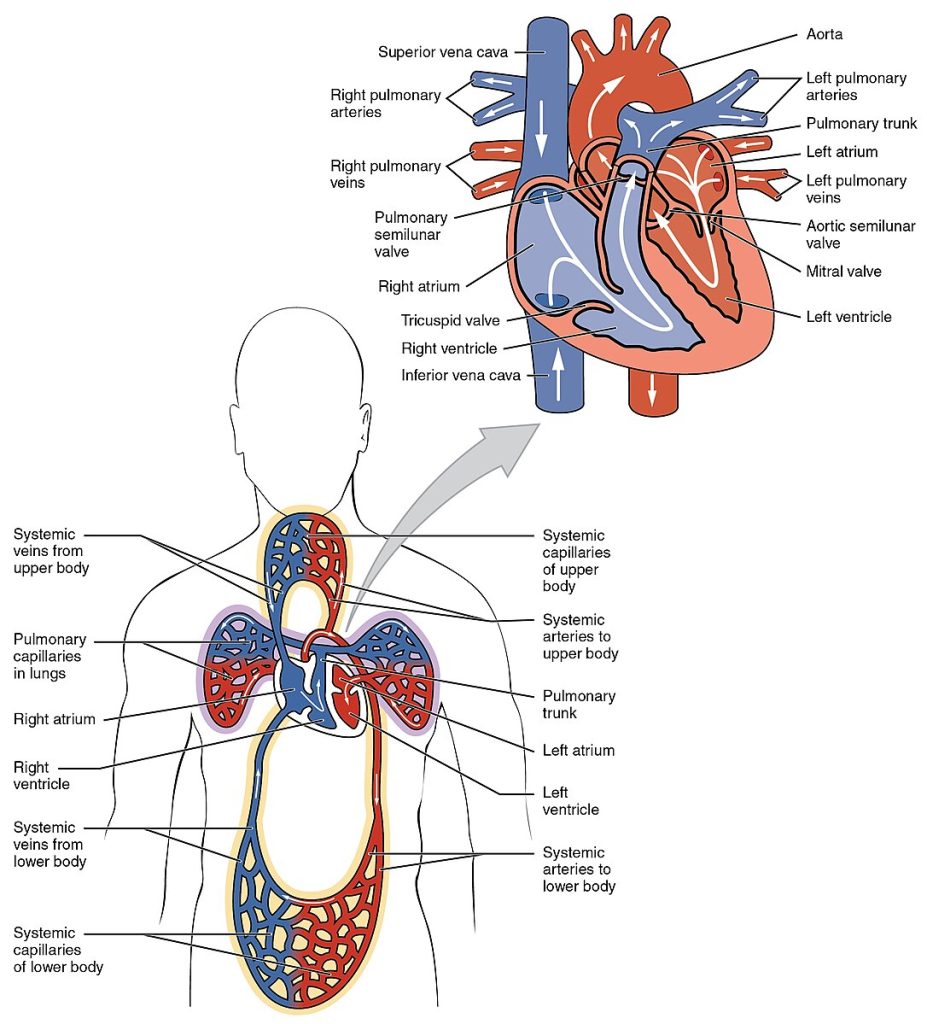
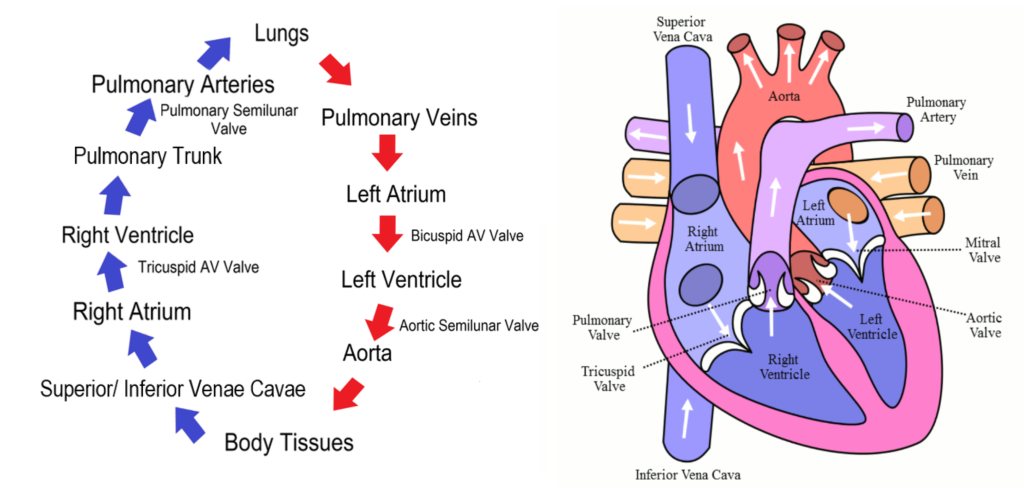
The heart acts as a double pump, simultaneously pumping blood to and from the lungs (pulmonary) and to and from the remainder of the body tissues (systemic). There are two distinct but connected circuits of blood circulation called pulmonary and systemic circulation. When learning about circulation, it is important to understand the function of arteries, vessels that carry blood away from the heart, and veins, vessels that bring blood back to the heart.
Pulmonary circulation transports deoxygenated blood to the lungs to pick up oxygen and drop off carbon dioxide for exhalation. Pulmonary circulation begins when the right ventricle pumps deoxygenated blood through the pulmonary trunk, which splits into the right and left pulmonary arteries to take the blood to each lung. (Note: The pulmonary trunk and the left and right pulmonary arteries and their branches are the only arteries in the body after birth that carry deoxygenated blood). These pulmonary arteries divide many times before reaching the pulmonary capillaries where oxygen is picked up and carbon dioxide is dropped off and exhaled. Freshly oxygenated blood then travels back to the left side of the heart via two right and two left pulmonary veins, which all carry blood to the left atrium. (Note: The pulmonary veins are the only veins in the body after birth that carry highly oxygenated blood). Additional information about the pulmonary circulation is described in the “Pulmonary Circulation” subsection of the “Blood Vessels” section.
Systemic circulation transports oxygenated blood to almost all tissues of the body and returns deoxygenated blood to the heart to be sent through the pulmonary circulation. Systemic circulation begins when the left ventricle pumps oxygenated blood through the aortic valve and into the aorta. Blood then travels through numerous systemic arteries to systemic arterioles (tiny arteries) and then to systemic capillaries where oxygen is dropped off for the tissues to use and carbon dioxide (a cellular waste product) is picked up. The now deoxygenated blood makes its way back to the heart via systemic venules (tiny veins), which merge together into larger systemic veins, and eventually flow into the superior and inferior venae cavae that return the deoxygenated blood back to the right atrium of the heart. Additional information about arteries and veins in the systemic circulation is described in the “Systemic Circulation” subsection of the “Blood Vessels” section.
See Figure 11.11[15] for an illustration showing pulmonary and systemic circulation. Note that the color blue is used to show deoxygenated blood, and the color red is used to show oxygenated blood.
See Figure 11.12[16] for an illustration of the circulation of blood flow.
Coronary Circulation
The heart is composed of cardiac muscle cells (cardiomyocytes) that are constantly active throughout life. Like all other cells, a cardiomyocyte requires a constant supply of oxygen and nutrients and a way to remove wastes.
Coronary Arteries and Veins
Coronary arteries supply oxygenated blood to the myocardium of the heart. The left and right coronary arteries originate from the base or root of the aorta as it leaves the left ventricle. The left coronary artery divides into smaller arteries and feeds the left atrium, left ventricle, and the interventricular septum. The right coronary artery also divides into smaller arteries and feeds the right atrium, portions of both ventricles, and the cardiac conduction system. Additional information will be discussed in the “Conduction System of the Heart” section.
Coronary veins collect deoxygenated blood from the myocardium. These veins are generally found parallel to the coronary arteries. Most of the coronary veins send blood to a large vein called the coronary sinus. The coronary sinus is a large, thin-walled vein on the posterior surface of the heart lying within the atrioventricular sulcus that empties blood directly into the right atrium. A sinus’ walls can’t change diameter to vasoconstrict or vasodilate like other vessels.
See Figure 11.13[17] for an illustration of the arteries and veins involved in coronary circulation from both the anterior and posterior views.
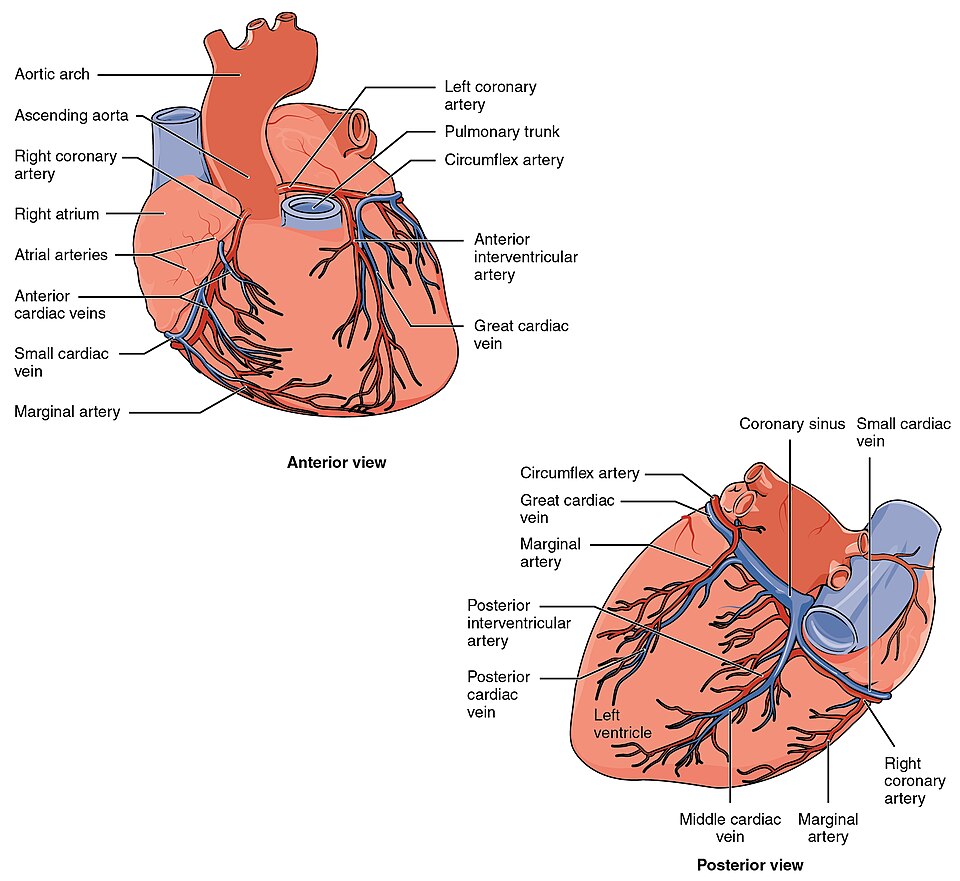
The left and right coronary arteries branch into smaller vessels that interconnect with other branches forming anastomoses. An anastomosis is a connection between two vessels that both supply the same region. It allows blood flow to a region even if there is a partial blockage in another branch.
View a supplementary YouTube video[18] overview of the cardiovascular system:
Cardiovascular System Overview, Animation
View a supplementary YouTube video[19] on the heart and circulation of blood:
Circulatory System and Pathway of Blood Through the Heart
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2001_Heart_Position_in_ThoraxN” by OpenStax College is licensed under CC BY 3.0 ↵
- “2004_Heart_Wall” by OpenStax College is licensed under CC BY 3.0 ↵
- “2006_Heart_Musculature” by OpenStax College is licensed under CC BY 3.0 ↵
- “Blausen_0451_Heart_Anterior” by Blausen Medical Communications, Inc. is licensed under CC BY 3.0 ↵
- “2008_Internal_Anatomy_of_the_HeartN” by OpenStax College is licensed under CC BY 3.0 ↵
- This image is a derivative of “Papillary muscle. 220/365” by PK VS and is licensed under CC BY 2.0 ↵
- “2007_Ventricular_Muscle_Thickness” by OpenStax College is licensed under CC BY 3.0 ↵
- “2011_Heart_Valves” by OpenStax College is licensed under CC BY 3.0 ↵
- “2012_Blood_Flow_Relaxed_Ventricles” by OpenStax College is licensed under CC BY 3.0 ↵
- Polk-Pohlman, B. (n.d.). The anatomy of the heart [Video]. Wisc-Online. CC BY 4.0. https://www.wisc-online.com/learn/general-education/anatomy-and-physiology1/ap16016/the-anatomy-of-the-heart-video ↵
- eastsidearrhythmia. (2013, February 26). Heart contraction and blood flow video animation [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=zJXAlh9VDDU ↵
- “Cardiac_muscle_histology_400x” by Alexander G. Cheroske is licensed under CC BY-SA 4.0 ↵
- Terashvil, M., & Bosnjak, Z. J. (2019). Stem cell therapies in cardiovascular disease. Journal of Cardiothoracic Vascular Anesthesia, 33(1), 209-222. https://doi.org/10.1053/j.jvca.2018.04.048 ↵
- “2003_Dual_System_of_Human_Circulation” by OpenStax College is licensed under CC BY 3.0 ↵
- This image is derived from “Circulation_of_blood_through_the_heart” by Christinelmiller and licensed under CC BY-SA 4.0 ↵
- “2014ab_Coronary_Blood_Vessels” by OpenStax College is licensed under CC BY 3.0 ↵
- Alila Medical Media. (2019, May 13). Cardiovascular system overview, animation [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=28CYhgjrBLA ↵
- Ameoba Sisters. (2020, August 26). Circulatory system and pathway of blood through the heart [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=_vZ0lefPg_0 ↵
Central portion of the thoracic cavity.
The pointed, inferior tip of the heart, located just left of the sternum.
The serous membrane that surrounds the heart, reducing friction caused by the beating of the heart.
The space between the heart and the pericardium, filled with serous fluid to reduce friction during heart contractions.
The tough outer layer of the pericardium made of dense connective tissue that protects the heart and anchors it in the chest.
A thin, double-layered membrane around the heart that reduces friction. It includes the parietal layer (outer) and the visceral layer (inner, also called the epicardium).
The outer layer of the serous pericardium that lines the inner surface of the fibrous pericardium.
Also known as the visceral pericardium, it is the inner layer of the serous pericardium that is fused to the surface of the heart and forms part of the heart wall.
The middle and thickest layer of the heart wall, composed mainly of cardiac muscle cells responsible for the heart’s contractions.
Dense connective tissue that reinforces the heart muscle. It includes four rings surrounding the openings between the atria and ventricles, and the openings to the pulmonary trunk and aorta.
The innermost layer of the heart wall, connected to the myocardium by a thin layer of connective tissue.
Simple squamous epithelium tissue that lines blood vessels.
Flaplike, thin-walled structures that can slightly expand to increase the volume of the atria, the upper chambers of the heart.
A groove or depression found on body surfaces, such as the fat-filled grooves on the heart that contain blood vessels or the shallow grooves in the brain's surface that create its folded appearance (plural = sulci).
A deep groove located between the atria and ventricles of the heart.
A groove on the front (anterior) surface of the heart that marks the boundary between the left and right ventricles.
A groove on the back (posterior) surface of the heart that marks the boundary between the left and right ventricles.
The two upper chambers of the heart that receive blood returning to the heart and pump it into the ventricles.
Hollow chambers or cavities within organs, such as the four pumping chambers of the heart or the fluid-filled spaces within the brain where cerebrospinal fluid circulates (singular = ventricle).
A wall or partition that divides a structure into separate parts, such as the walls separating the chambers of the heart.
The wall or partition that separates the right and left ventricles of the heart.
The wall or partition that separates the atria (upper heart chambers) from the ventricles (lower heart chambers).
A specialized structure that ensures one-way flow of blood.
The heart’s chamber that receives deoxygenated blood from the body’s systemic circulation and directs it to the right ventricle.
A large vein that carries deoxygenated blood from the head, neck, upper limbs, and chest back to the right atrium of the heart.
A large vein that carries deoxygenated blood from the lower limbs and abdominopelvic region back to the right atrium of the heart.
A thin-walled vessel on the posterior surface of the right atrium that receives deoxygenated blood from the heart muscle and empties it into the right atrium.
Systemic veins that collect deoxygenated blood from the heart muscle and drain it into the coronary sinus.
A small oval-shaped depression on the interatrial septum, marking the spot of a fetal opening called the foramen ovale.
An opening in the fetal heart that allowed blood to flow directly from the right atrium to the left atrium, bypassing the lungs before birth.
Muscular ridges found on the inner surface of the anterior right atrium of the heart.
The valve between the right atrium and right ventricle that prevents backflow of blood when the ventricle contracts.
Tough, fibrous cords that connect the valve flaps (cusps) of the tricuspid and mitral valves to papillary muscles in the ventricles.
Small muscles inside the heart ventricles that attach to chordae tendineae and help prevent valve flaps from inverting during contraction.
A large artery that carries blood out away from the right ventricle.
Carry the deoxygenated blood to the lungs.
Irregular ridges of cardiac muscle lining the inner walls of the ventricles, helping to reduce suction and improve heart efficiency during contraction.
A muscular band of heart tissue found in the right ventricle that carries part of the conduction system (right bundle branch) to the anterior papillary muscle, helping coordinate ventricular contraction.
The valve between the left atrium and left ventricle; it has two flaps (cusps) and prevents backflow of blood into the left atrium during ventricular contraction. Also called the bicuspid valve.
Valves located between the atria and ventricles that prevent backflow of blood into the atria during ventricular contraction.
Valves located at the openings of the heart leading to the pulmonary trunk (pulmonary valve) and the aorta (aortic valve); they prevent backflow of blood into the ventricles after contraction.
A semilunar valve located at the base of the pulmonary trunk that prevents backflow of blood into the right ventricle after it contracts.
The heart's ability to generate its own electrical impulses without input from the nervous system, allowing it to contract in a regular, rhythmic pattern.
Allows the cardiac muscle cells to coordinate contraction so that the heart can work as a pump.
Blood vessels that carry blood away from the heart to the body's tissues. Most arteries carry oxygenated blood, except for the pulmonary arteries, which carry deoxygenated blood to the lungs.
Vessels that bring blood back to the heart.
The portion of the circulatory system that carries deoxygenated blood from the right side of the heart to the lungs to pick up oxygen and release carbon dioxide, and then returns oxygenated blood to the left side of the heart.
Transports oxygenated blood to almost all tissues of the body and returns deoxygenated blood to the heart to be sent through the pulmonary circulation.
A connection between two blood vessels that supply the same area, providing an alternate pathway for blood flow.

