10.8 Blood Disorders
Blood Disorders[1]
Anemia
The size, shape, and number of erythrocytes and the number of hemoglobin molecules can have a major impact on a person’s oxygenation status and overall health. Anemia is a general condition involving a deficient number of red blood cells (RBCs) or hemoglobin. More than 3.5 million Americans suffer from over 400 types of anemia. The effects of the various anemias are widespread across body systems because deficient numbers of RBCs or hemoglobin result in lower levels of oxygen being delivered to body tissues. Because oxygen is required for tissue functioning, anemia produces shortness of breath, fatigue, lethargy, and an increased risk for infection. An oxygen deficit in the brain impairs the ability to think clearly and may prompt headaches and irritability.
Anemia can be categorized into three major types: those caused by blood loss, those caused by faulty or decreased RBC production, and those caused by excessive destruction of RBCs:
- Anemia caused by blood loss can be the result of excessive menstruation; excessive blood loss during childbirth; bleeding from wounds, ulcers, or hemorrhoids; inflammation of the stomach (gastritis); and cancer of the gastrointestinal tract. Excessive use of aspirin or other nonsteroidal anti-inflammatory drugs such as ibuprofen can trigger ulceration and gastritis.
- Anemias caused by faulty or decreased RBC production include iron-deficiency anemia, vitamin-deficiency anemia, and diseases of the bone marrow and stem cells. Chronic kidney disease is often associated with a decreased production of erythropoietin (EPO), resulting in decreased production of RBC.
- Anemia caused by destruction of RBC includes sickle cell anemia and hemolytic anemia.
Examples of common types of anemias are discussed in the following subsections.
Iron-Deficiency Anemia
Iron-deficiency anemia is the most common type of anemia that results from an insufficient amount of iron to produce heme, the oxygen-binding component of hemoglobin. This condition can occur due to a deficiency of iron in the diet that is common in vegans, vegetarians, children, adolescents, and older adults. Iron-deficiency anemia can also be caused by an inability to absorb iron in the gastrointestinal tract or slow, chronic bleeding.
Vitamin-Deficiency Anemia
Vitamin-deficiency anemias often involve insufficient vitamin B12 and folate, also referred to as megaloblastic anemia. It is typically caused by diets deficient in these essential nutrients. Lack of meat or eating insufficient amounts of vegetables may lead to a lack of folate or vitamin B12. Vitamin-deficiency anemia can be caused by pregnancy, side effects of certain medications, excessive alcohol consumption, gastrointestinal bypass surgery, or gastrointestinal disease such as celiac disease. It is essential to provide sufficient folic acid during the early stages of pregnancy to reduce the risk of neural tube defects, such as spina bifida, in the newborn.
Sickle Cell Anemia
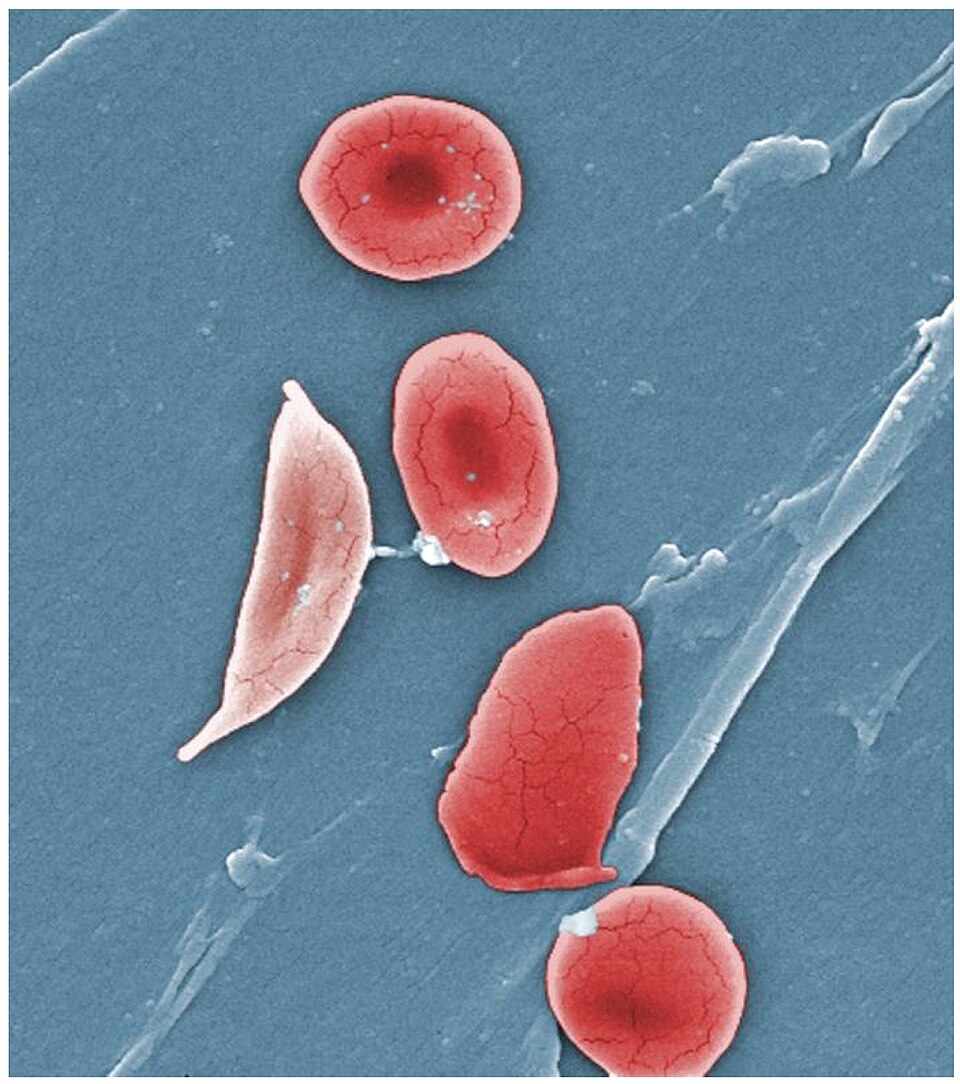
Sickle cell disease is a genetic disorder commonly found in individuals of African descent that causes production of an abnormal type of hemoglobin, called hemoglobin S. In sickle cell anemia, abnormal hemoglobin causes red blood cells to become crescent-shaped, reducing their ability to carry oxygen, especially during episodes triggered by low oxygen levels or dehydration. These abnormally shaped cells can then become lodged in narrow capillaries and block blood flow to tissues and organs, causing a variety of complications. See Figure 10.11[2] for an illustration of sickled red blood cells.
Aplastic Anemia
Aplastic anemia is a rare condition caused by stem cells in the bone marrow not producing enough RBCs, WBCs, and platelets. Aplastic anemia is often inherited or can be triggered by radiation, medication, chemotherapy, or infection.
Anemia of Chronic Disease
Anemia of chronic disease occurs as a result of other long-term conditions, particularly those that cause inflammation. Long-term inflammation can make it difficult for the body to make sufficient red blood cells, which leads to anemia. Some diseases that can cause anemia of chronic disease are cancer, chronic kidney disease, congestive heart failure, and autoimmune conditions such as rheumatoid arthritis or lupus. Treatment of anemia of chronic disease consists of managing the underlying condition that led to anemia in the first place. Other treatments may include blood transfusions, synthetic erythropoietin, or iron supplements.[3]
Leukocyte Disorders
Leukopenia is a condition in which not enough leukocytes are produced, increasing the risk of infection. Conversely, excessive leukocyte production, known as leukocytosis, often results in nonfunctional WBCs that also increases the risk for infection.
Leukemia is a blood cancer involving an abundance of leukocytes. In chronic leukemia, mature leukocytes accumulate and fail to die. In acute leukemia, there is an overproduction of young, immature leukocytes. In both conditions, the white blood cells do not function properly and increase the risk for infection. They also crowd out the production of erythrocytes and platelets, which causes anemia and bleeding problems too.
Hemophilia
Hemophilia is a genetic bleeding disorder in which blood doesn’t clot properly that can lead to hemorrhage from injuries, surgery, or spontaneous bleeding (bleeding that occurs for no known reason). Blood contains many proteins called clotting factors that help stop bleeding. The severity of hemophilia that a person has is determined by the amount of factor in the blood. The lower the amount of the factor, the more likely it is that bleeding will occur, which can lead to serious health problems.[4] Inherited hemophilia occurs in about 1 of every 5,000 male births. About 33,000 males in the United States are living with the disorder.
Hemorrhage
Minor blood loss is managed by hemostasis and repair. Hemorrhage is a loss of blood that cannot be controlled by hemostatic mechanisms. Initially, the body responds to hemorrhage by initiating mechanisms aimed at increasing blood pressure and maintaining blood flow. Ultimately, however, blood volume will need to be restored, either through physiological processes or through medical intervention.
Polycythemia
An elevated RBC count is called polycythemia and is detected in a patient’s elevated hematocrit (percentage of red blood cells). It can occur transiently in a person who is dehydrated; when water intake is inadequate or water losses are excessive, the plasma volume decreases. As a result, the hematocrit rises.
A mild form of polycythemia is chronic but normal in people living at high altitudes. Some elite athletes train at high elevations specifically to induce this phenomenon.
A type of bone marrow disease called polycythemia vera (from the Greek vera = “true”) causes an excessive production of immature RBCs, WBCs, and platelets. Polycythemia vera can dangerously elevate the viscosity of blood, raising blood pressure and making it more difficult for the heart to pump blood throughout the body. Polycythemia occurs more often in males than in females and is more likely to be present in elderly patients over 60 years of age.
Thrombosis and Embolism
A thrombus (plural = thrombi) is a blood clot. While the formation of a clot is normal following hemostasis triggered by a vessel injury, development of an abnormal thrombus can seriously impede blood flow. An excessive production of platelets can lead to severe disease or death. Thrombocytosis is a condition in which too many platelets are produced and may trigger the formation of unwanted blood clots, causing a potentially life-threatening condition known as thrombosis. When a portion of a thrombus breaks free from the vessel wall and enters the circulation, it is referred to as an embolus. An embolus that is carried through the bloodstream can be large enough to block a vessel to a major organ. When this happens, it is called an embolism. An embolism may affect the heart, brain, or lungs.
When the inner lining of blood vessels is damaged, thrombi can form. Vessel damage can be caused by conditions such as venous stasis, when blood in the veins, particularly in the legs, remains still for long periods. For example, venous stasis during long airplane flights can cause deep vein thrombosis (DVT).
Thrombophilia, also called hypercoagulation, is a condition in which there is a tendency to form thrombi. This may be familial (genetic) or acquired. Acquired forms include the autoimmune disease lupus, immune reactions to heparin, polycythemia vera, thrombocytosis, sickle cell disease, pregnancy, and even obesity.
Thrombocytopenia[5]
An insufficient number of platelets is called thrombocytopenia and can result in excessive bleeding if the blood does not clot properly.
Thrombocytopenia can be caused by either an increased destruction of platelets or a reduction in platelet production. Thrombocytopenia has been linked to autoimmune conditions, certain medications, infections, and cancer.
Treatment of thrombocytopenia depends on the specific cause of the disorder. Potential treatment options are managing underlying conditions, monitoring platelet counts, stopping medications that affect platelet production, and transfusing platelets in severe cases.
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “1911_Sickle_Cells” by OpenStax College is licensed under CC BY 3.0 ↵
- Cleveland Clinic. (2022). Anemia of chronic disease. https://my.clevelandclinic.org/health/diseases/14477-anemia-of-chronic-disease ↵
- Centers for Disease Control and Prevention. (2025). About hemophilia. https://www.cdc.gov/hemophilia/about/index.html ↵
- Jinna, S., & Khandhar, P. B. (2023). Thrombocytopenia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK542208/ ↵
A general condition characterized by a deficient number of red blood cells (RBCs) or low hemoglobin levels.
A condition where too few leukocytes (white blood cells) are produced, increasing the risk of infection.
Excessive production of leukocytes (white blood cells), often resulting in nonfunctional WBCs and an increased risk of infection.
A blood cancer characterized by an excessive number of leukocytes (white blood cells).
A genetic bleeding disorder in which blood does not clot properly, leading to hemorrhage from injuries, surgery, or spontaneous bleeding (bleeding with no known cause).
Excessive or uncontrolled bleeding.
An elevated red blood cell (RBC) count, often detected by an increased hematocrit (the percentage of red blood cells in the blood).
A type of bone marrow disease that causes excessive production of immature red blood cells (RBCs), white blood cells (WBCs), and platelets.
A blood clot.
A condition in which too many platelets are produced, potentially triggering unwanted blood clots that can be life-threatening.
A potentially life-threatening condition caused by the formation of unwanted blood clots inside blood vessels.
A portion of a thrombus that breaks free from the vessel wall and enters the circulation.
A condition that occurs when an embolus travels through the bloodstream and blocks a blood vessel supplying a major organ.
A condition in which blood in the veins, especially in the legs, remains still or flows very slowly for long periods, increasing the risk of vessel damage.
A condition characterized by an increased tendency to form blood clots (thrombi).
An insufficient number of platelets in the blood, which can lead to excessive bleeding due to impaired clotting.

