10.7 Blood Types
Blood Types[1]
ABO Blood Groups
The major human blood groups were discovered in 1900 by Karl Landsteiner, an Austrian biologist and physician. Blood groups are determined by the presence or absence of specific carbohydrate marker molecules on the plasma membranes of erythrocytes. With their discovery, it became possible to match patient-donor blood types and prevent transfusion reactions and deaths. Until that point, physicians did not understand why death sometimes followed blood transfusions.
Although the ABO blood group name consists of three letters, ABO blood typing designates the presence or absence of just two antigens called A and B. Antigens are substances that may trigger a defensive response from leukocytes of the immune system if the body does not recognize the antigen as belonging to “self.”
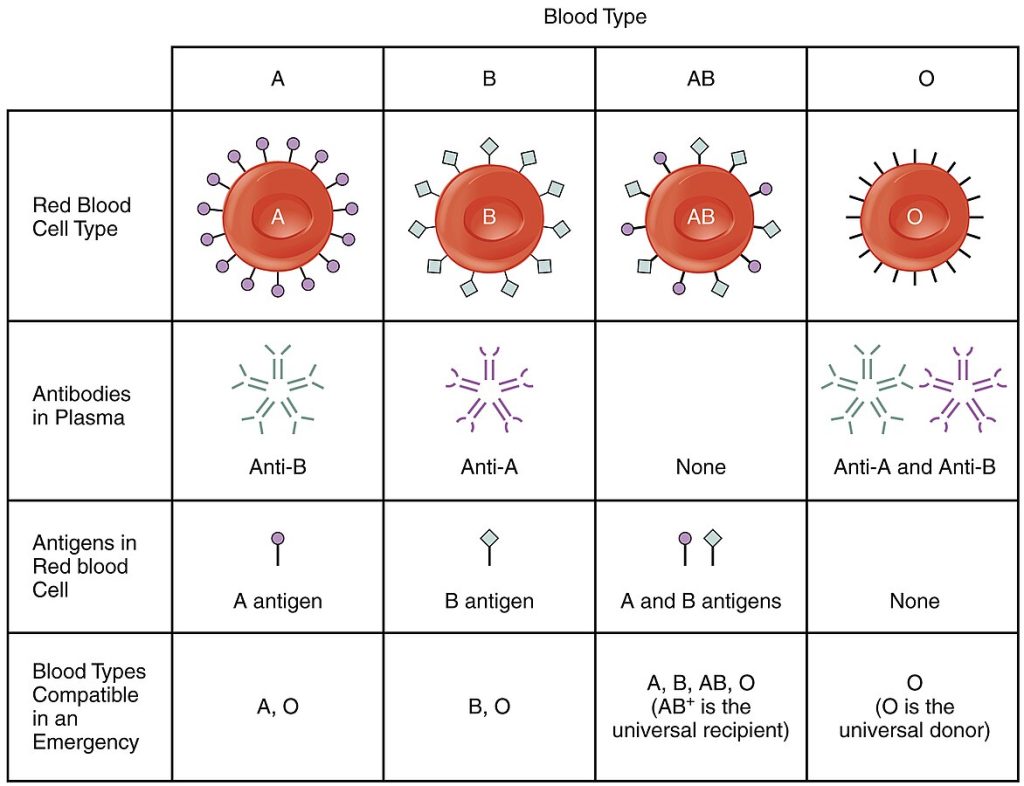
ABO blood types are genetically determined. People whose erythrocytes have A antigens on their membrane surfaces are designated blood type A, and people whose erythrocytes have B antigens are designated blood type B. Some people have both A and B antigens on their erythrocytes, in which case they are designated blood type AB. Some people don’t have A or B antigens on their red blood cells and are designated blood type O.
When a person’s body is exposed to a foreign antigen, an antibody is produced by their immune system that labels that antigen as “foreign.” ABO blood group antigens are found in foods and microbes throughout nature, so individuals’ immune systems are exposed to A and B antigens at an early age, and antibodies are formed naturally. Because of this natural exposure, individuals with blood type A have naturally formed antibodies to the B antigen circulating in their blood plasma. These antibodies, referred to as anti-B antibodies, will cause agglutination and hemolysis if they are exposed to erythrocytes with B antigens. Similarly, an individual with type B blood has naturally formed anti-A antibodies that will cause agglutination and hemolysis if they are exposed to erythrocytes with A antigens. People with blood type O do not have A or B antigens on their erythrocytes, so they have anti-A and anti-B antibodies circulating in their blood plasma that will cause agglutination and hemolysis if they are exposed to erythrocytes with A or B antigens. However, individuals with blood type AB have both A and B antigens and do not have naturally formed antibodies to either of these antigens, so they can receive a transfusion of blood type A, B, AB, or O.
Read additional information about blood types:
Rh Factor
The Rh factor is classified according to the presence or absence of another erythrocyte antigen identified as Rh. Although dozens of Rh antigens have been identified, only one, designated D, is clinically important. Those who have the Rh D antigen present on their erythrocytes—about 85 percent of Americans—are described as Rh positive (Rh+), and those who lack it are Rh negative (Rh−).
The Rh factor is separate from the ABO group, so any individual, no matter their ABO blood type, may have or lack this Rh antigen. When identifying a patient’s blood type, the Rh factor is designated by adding the word positive or negative to the ABO type. For example, A positive (A+) means ABO group A blood with the Rh antigen present, and AB negative (AB−) means ABO group AB blood without the Rh antigen. See Table 10.7 for a summary of the distribution of the ABO and Rh blood types within the United States.
Table 10.7. Summary of ABO and Rh Blood Types Within the United States[2]
| Blood Type | Asian | Black non-Hispanic | Hispanic | North American Indian | White non-Hispanic |
| A+ | 27.3 | 24.0 | 28.7 | 31.3 | 33.0 |
| A− | 0.5 | 1.9 | 2.4 | 3.8 | 6.8 |
| B+ | 25.0 | 18.4 | 9.2 | 7.0 | 9.1 |
| B− | 0.4 | 1.3 | 0.7 | 0.9 | 1.8 |
| AB+ | 7.0 | 4.0 | 2.3 | 2.2 | 3.4 |
| AB− | 0.1 | 0.3 | 0.2 | 0.3 | 0.7 |
| O+ | 39.0 | 46.6 | 52.6 | 50.0 | 37.2 |
| O− | 0.7 | 3.6 | 3.9 | 4.7 | 8.0 |
Antibodies to the Rh antigen are produced only in Rh− individuals after they are exposed to the antigen. This process, called sensitization, occurs following a transfusion with Rh-incompatible blood or, more commonly, with the birth of an Rh+ baby to a mother who is Rh−. The baby’s Rh+ cells rarely cross the placenta during pregnancy, but during or immediately after childbirth, the Rh− mother is often exposed to the baby’s Rh+ cells. After exposure, the mother’s immune system begins to generate anti-Rh antibodies. If the mother later becomes pregnant with another Rh+ baby, the Rh antibodies can cross the placenta into the fetal bloodstream and destroy the fetal RBCs. This condition, known as hemolytic disease of the newborn (HDN) or erythroblastosis fetalis, can cause wide-ranging effects in the baby if left untreated, ranging from anemia to death. See Figure 10.9[3] for an illustration of hemolytic disease of the newborn.
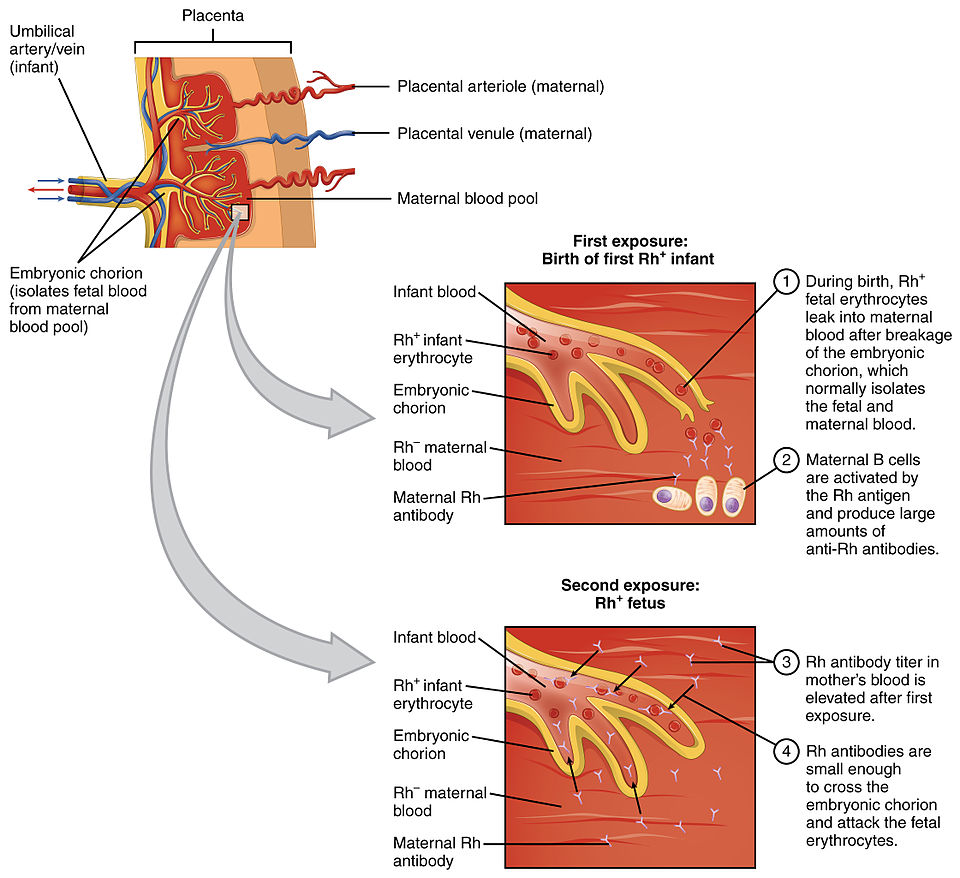
A drug known as RhoGAM, short for Rh immune globulin, can prevent the development of Rh antibodies in the Rh− mother, thereby avoiding this potentially serious disease for the fetus. RhoGAM antibodies destroy any fetal Rh+ erythrocytes that may cross the placental barrier. RhoGAM is typically administered to Rh− pregnant women during weeks 26−28 of pregnancy and within 72 hours following birth of an Rh+ baby and effectively decreases the incidence of HDN.
ABO Transfusion Protocols
To avoid incompatibility reactions, matching blood types are typically transfused. For example, a patient with blood type B+ receives blood from a donor with blood type B+. In emergency situations where a patient could die from massive blood loss, blood from a universal donor (i.e., an individual with type O− blood) may be transfused because no antigens are present to trigger a reaction. Recall that type O erythrocytes do not display A or B antigens, and, therefore, have nothing to provoke an immune response.
However, if the donor with blood type O− had prior exposure to the Rh antigen, Rh antibodies may be present in the donated blood and trigger agglutination to some degree. Also, donated O- blood has antibodies present against A and B antigens, which may cause some problems for the recipient, but because the volume of blood transfused is much lower than the volume of the patient’s own blood, the adverse effects of the relatively few infused plasma antibodies are typically limited.
A patient with blood type AB+ is known as the universal recipient. This patient can theoretically receive any type of blood because the patient’s own blood—having both A and B antigens on the erythrocyte surface—does not produce anti-A or anti-B antibodies. In addition, an Rh+ patient can receive both Rh+ and Rh− blood. However, keep in mind that the donor’s blood will contain circulating antibodies that can cause negative implications. See Figure 10.10[4] for a summary of ABO blood types and compatibilities.
Complete this supplementary learning activity[5] about blood groups: Wisc-Online Blood Groups
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “1910_Erythroblastosis_Fetalis” by OpenStax College is licensed under CC BY 3.0 ↵
- “1913_ABO_Blood_Groups” by OpenStax College is licensed under CC BY 3.0 ↵
- Liang, B. (n.d.). Blood groups [Video]. Wisc-Online. CC BY 4.0. https://www.wisc-online.com/learn/general-education/anatomy-and-physiology1/ap17318/blood-groups ↵
Substances that may trigger a defensive response from leukocytes of the immune system if the body does not recognize the antigen as belonging to "self."
A blood type classification for individuals whose erythrocytes (red blood cells) have A antigens on their membrane surface.
A blood type classification for individuals whose erythrocytes (red blood cells) have B antigens on their surface.
A blood type classification for individuals whose erythrocytes (red blood cells) have both A and B antigens on their surfaces.
A blood type classification for individuals whose red blood cells lack both A and B antigens.
The process by which an Rh− individual produces antibodies against the Rh antigen after exposure, such as through an Rh-incompatible transfusion or pregnancy with an Rh+ baby.
A condition that occurs when an Rh− mother has developed antibodies against Rh+ red blood cells, which cross the placenta and destroy the red blood cells of her Rh+ fetus.
A condition that occurs when an Rh− mother has developed antibodies against Rh+ red blood cells, which cross the placenta and destroy the red blood cells of her Rh+ fetus.
Short for Rh immune globulin, this medication prevents an Rh− mother from developing antibodies against Rh+ red blood cells, helping to avoid hemolytic disease of the newborn.
An individual with type O− blood who can donate blood to anyone because their red blood cells lack A, B, and Rh antigens, reducing the risk of an immune reaction.
A patient with blood type AB+ who can receive red blood cells from any blood type because their blood contains all A, B, and Rh antigens, so they do not produce antibodies against these antigens.

