10.4 Components of Blood
Components of Blood[1]
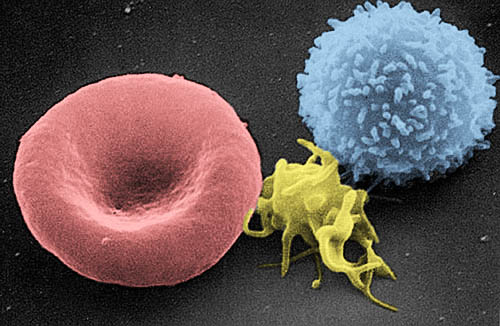
As mentioned previously, the major components of the blood are plasma and formed elements. Formed elements are the cellular components of blood that include erythrocytes (red blood cells), leukocytes (white blood cells), and thrombocytes (platelets). See Figure 10.1[2] for an image of a red blood cell, platelet, and white blood cell.
See Table 10.4a for an overview of blood components.
Table 10.4a. Blood Components[3]
| Component and % of Blood | Subcomponent and % of Component | Type and % (where appropriate) | Site of Production | Major Functions |
|---|---|---|---|---|
| Plasma 46-63 percent |
Water 92 percent |
Fluid | Absorbed by intestinal tract or produced by metabolism | Transport medium |
| Plasma proteins 7 percent |
Albumin 54-60 percent |
Liver | Maintain osmotic concentration; transport lipid molecules |
|
| Globulins 35-36 percent |
Alpha globulins – liver | Transport and maintain osmotic concentration |
||
| Beta globulins – liver | Transport and maintain osmotic concentration |
|||
| Gamma globulins (immunoglobulins) – plasma cells | Immune responses | |||
| Fibrinogen 4-7 percent |
Liber | Blood clotting in hemostasis | ||
| Regulatory proteins < 1 percent |
Hormones and enzymes | Various sources | Regulate various body functions | |
| Other solutes 1 percent |
Nutrients, gases, and wastes | Absorbed by intestinal tract, exchanged in respiratory system, or produced by cells | Numerous and varied | |
| Formed elements 37-54 percent | Erythrocytes 99 percent |
Erythrocytes | Red bone marrow | Transports gases, primarily oxygen and some carbon dioxide |
| Leukocytes < 1 percent |
Granular leukocytes: neutrophils eosinophils basophils | Red bone marrow | Nonspecific immunity | |
| Agranular leukocytes: lymphocytes monocytes | Lymphocytes: bone marrow and lymphatic tissue |
Lymphocytes: nonspecific and specific immunity | ||
| Monocytes: red bone marrow |
Monocytes: nonspecific immunity | |||
| Platelets < 1 percent |
Megakaryocytes: red bone marrow |
Hemostasis |
See Table 10.4b for a summary of the functions of the formed elements found in the blood.
Table 10.4b. Formed Elements in the Blood[4]
| Formed Element | Major Subtypes | Numbers Present Per Microliter (ul) and Mean (range) | Appearance in Standard Blood Smear | Summary of Functions | Comments |
|---|---|---|---|---|---|
| Erythrocytes (red blood cells) | 5.3 million (4.4-6.0 million) | Flattened biconcave desk, no nucleus, and pale red color | Transport oxygen and some carbon dioxide between tissues and lungs | Life span of approximately 120 days | |
| Leukocytes (white blood cells) | 7,000 (5,000-10,000) | Obvious dark-staining nucleus | All function in body defenses | Exit capillaries and move into tissues; life span of usually a few hours or days | |
| Leukocytes (white blood cells) | Granulocytes, including neutrophils, eosinophils, and basophils | 4,360 (1,800-9,950) | Abundant granules in cytoplasm; nucleus normally lobed | Nonspecific (innate) resistance to disease | Classified according to membrane-bound granules in cytoplasm |
| Neutrophils | 4,150 (1,800-7,300) | Nuclear lobes increase with age; pale lilac granules | Phagocytic; particularly effective against bacteria. Release cytotoxic chemicals from granules | Most common leukocyte; life span of minutes to days | |
| Eosinophils | 165 (0-700) | Nucleus generally two-lobed; bright red-orange granules | Phagocyte cells; particularly effective with antigen-antibody complexes. Release antihistamines. Increase in allergies and parasitic infections | Life span of minutes to days | |
| Basophils | 44 (0-150) | Nucleus generally two-lobed but difficult to see due to presence of heavy, dense, dark purple granules | Promotes inflammation | Least common leukocyte; life span unknown | |
| Agranulocytes, including lymphocytes and monocytes | 2,640 (1,700-4,950) | Lacks abundant granules in cytoplasm; have a simple-shaped nucleus that may be indented | Body defenses | Group consists of two major cell types from different lineages | |
| Lymphocytes | 2,185 (1,500-4,000) | Spherical cells with a single often large nucleus occupying much of the cell’s volume; stains purple; seen in large (natural killer cells) and small (B and T cells) variants | Primarily specific (adaptive) immunity: T cells directly attach other cells (cellular immunity); B cells release antibodies (humoral immunity); natural killer cells are similar to T cells but non-specific | Initial cells originate in bone marrow, but secondary production occurs in lymphatic tissue; several distinct subtypes; memory cells form after exposure to a pathogen and rapidly increase responses to subsequent exposure; life span of many years | |
| Monocytes | 455 (200-950) | Largest leukocyte with an indented or horseshoe-shaped nucleus | Very effective phagocytic cells engulfing pathogens or worn-out cells; also serve as antigen-presenting cells (APCs) for other components of the immune system | Produced in red bone marrow; referred to as macrophages after leaving circulation | |
| Platelets | 350,000 (150,000-500,000) |
Cellular fragments surrounded by a plasma membrane and containing granules; purple stain | Hemostasis; release growth factors for repair and healing of tissue | Formed from megakaryocytes that remain in the red blood marrow and shed platelets into circulation | |
Each blood component is discussed in more detail in the following subsections.
Plasma
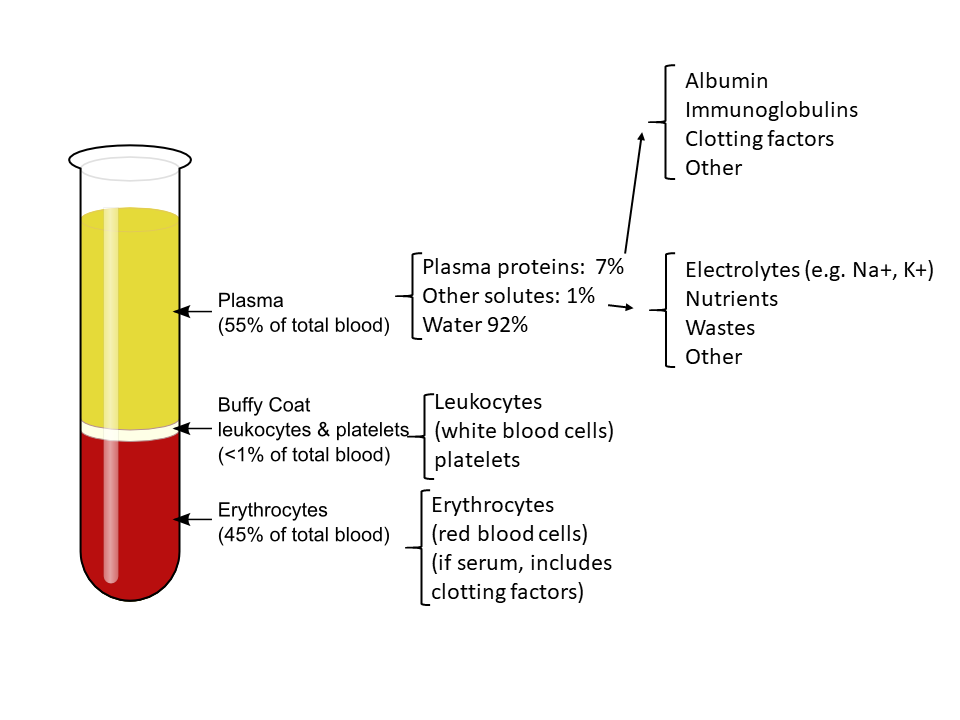
Plasma is a straw-colored fluid that transports a mixture of substances, most of which are proteins. Plasma is composed of about 92 percent water.
Plasma Proteins
About 7 percent of the volume of plasma – nearly all that is not water – is made of proteins. These include several plasma proteins (proteins that are unique to the plasma), plus a much smaller number of regulatory proteins, including enzymes and some hormones.
The three major groups of plasma proteins are as follows:
- Albumin: Albumin is the most abundant of the plasma proteins. Albumin normally accounts for approximately 54 percent of the total plasma protein content, with a normal blood sample level of 3.5–5.0 g/dL. Manufactured by the liver, albumin molecules serve as binding proteins that transport fatty acids and steroid hormones. Lipids are hydrophobic, so binding to albumin enables their transport in the watery plasma. Albumin also contributes to the osmotic pressure of blood, meaning its presence holds water inside the blood vessels and also draws water from the tissues into the bloodstream. Osmotic pressure helps to maintain blood volume and blood pressure.
- Globulins: Globulins are the second most common type of plasma proteins and make up approximately 38 percent of the total plasma protein volume, with a normal blood sample level of 1.0–1.5 g/dL. There are three main subgroups known as alpha, beta, and gamma globulins. The alpha and beta globulins transport iron, lipids, and the fat-soluble vitamins A, D, E, and K to the cells, and like albumin, they also contribute to osmotic pressure. The gamma globulins are proteins involved in immunity and are commonly known as antibodies (Ab) or immunoglobulins (Ig). Although other plasma proteins are produced by the liver, immunoglobulins are produced by specialized leukocytes known as plasma cells.
- Fibrinogen: Fibrinogen is the third major plasma protein and accounts for about 7 percent of the total plasma protein volume, with a normal blood sample level of 0.2–0.45 g/dL. Fibrinogen is essential for blood clotting. Like albumin and the alpha and beta globulins, fibrinogen is produced by the liver.
Other Plasma Solutes
In addition to proteins, plasma contains a wide variety of other substances that make up approximately 1 percent of the total volume of plasma. These substances include various electrolytes, such as sodium, potassium, and calcium ions; dissolved gases, such as oxygen, carbon dioxide, and nitrogen; various organic nutrients, such as vitamins, lipids, glucose, and amino acids; and metabolic wastes.
See Figure 10.2[5] for an illustration of the components of blood and plasma after a blood sample was centrifuged in a test tube.
Erythrocytes (Red Blood Cells)
The erythrocyte, commonly known as a red blood cell (RBC), is the most abundant formed element. A single drop of blood contains millions of erythrocytes and only thousands of leukocytes. Specifically, males have about 5.4 million erythrocytes per microliter (µL) of blood, and females have approximately 4.8 million per µL. In fact, erythrocytes are estimated to make up about 25 percent of the total cells in the body. As you can imagine, they are quite small cells, with a mean diameter of only about 7–8 micrometers (µm).
Functions of Erythrocytes
The primary function of erythrocytes is to carry oxygen from the lungs to the body’s tissues, but they also pick up some carbon dioxide from the tissues and transport it to the lungs for exhalation. Erythrocytes can release a chemical called nitric oxide to dilate blood vessels (vasodilation) to decrease blood pressure. Erythrocytes remain within blood vessels.
Anatomy of Erythrocytes
As an erythrocyte matures, the nucleus and most of its other organelles are ejected. During the first day or two that it is in circulation, an immature erythrocyte, known as a reticulocyte, often contains remnants of organelles that are quickly shed as it matures. Reticulocytes make up about 1–2 percent of the erythrocyte count and provide a rough estimate of the rate of RBC production.
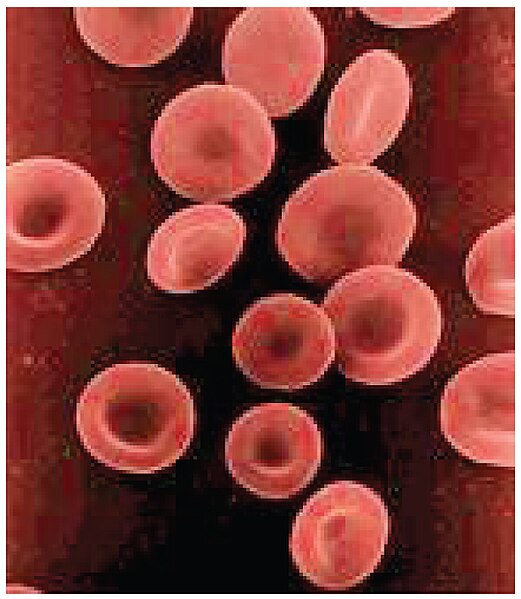
Erythrocytes are biconcave disks, meaning they are plump around the edge and very thin in the center. See Figure 10.3[6] for an image of erythrocytes. Because they lack most organelles, there is more interior space for hemoglobin molecules to transport gases. The biconcave shape also provides a greater surface area for gas exchange to occur.
Capillary beds are extremely narrow, which slows the passage of the erythrocytes and provides an extended opportunity for gas exchange to occur. However, the space within capillaries can be so small that erythrocytes may have to fold in on themselves to make it through. Fortunately, their structural proteins are flexible, allowing them to bend and then spring back again when they enter a wider vessel.
Hemoglobin
Hemoglobin is a large molecule made up of four protein chains. Each chain holds an iron atom capable of binding to an oxygen molecule. Each hemoglobin molecule can transport four oxygen molecules. An individual erythrocyte contains about 300 million hemoglobin molecules, and, therefore, can bind to and transport up to 1.2 billion oxygen molecules.
Hematocrit
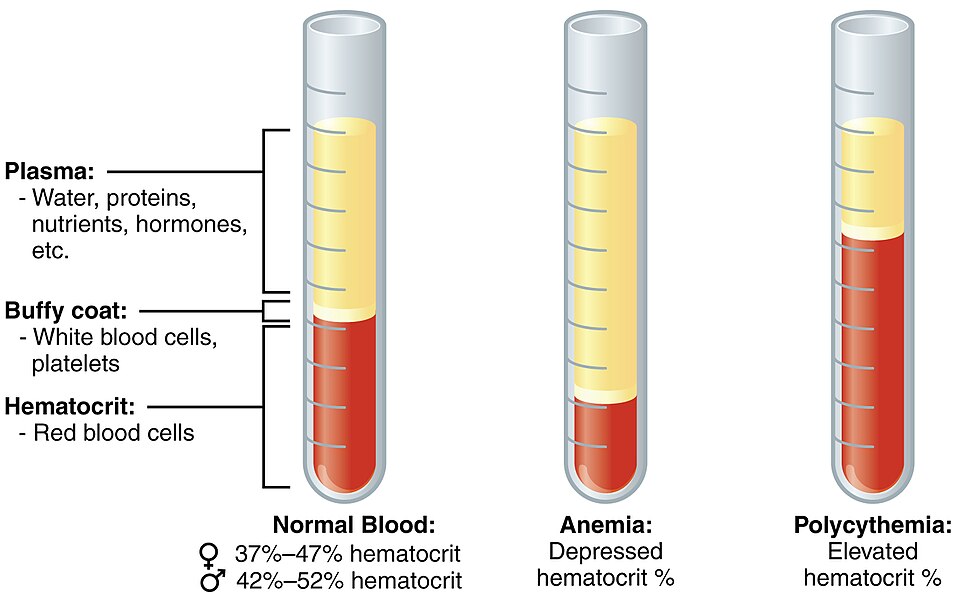
A hematocrit is a blood test that measures the percentage of erythrocytes (RBCs) in a blood sample. A hematocrit is performed by spinning a blood sample in a centrifuge, a process that causes the heavier elements in the blood sample to separate from the lightweight liquid plasma. Because the RBCs are the heaviest components of blood, they settle at the bottom of the test tube. Located above the RBCs in the test tube is a pale, thin layer composed of the remaining formed elements, including the WBCs (leukocytes) and the platelets (thrombocytes). This thin layer is referred to as the buffy coat because of its color and normally makes up less than 1 percent of a blood sample. Above the buffy coat is the blood plasma, a pale, straw-colored fluid. See Figure 10.4[7] for an illustration of the hematocrit blood test. Depressed and elevated hematocrit levels associated with anemia and polycythemia are shown for comparison to normal hematocrit levels.
Life Cycle of Erythrocytes
Erythropoiesis is the production of erythrocytes. It is stimulated by erythropoietin, a hormone made by the kidneys, and occurs in the red bone marrow at the staggering rate of more than 2 million cells produced per second. Erythrocytes live up to 120 days in the circulation, after which the worn-out cells are removed by a phagocytic cell called a macrophage in the bone marrow, liver, and spleen.
RBC Disorders
Anemia
Anemia is a condition where either an insufficient number of erythrocytes or hemoglobin is produced, which can significantly affect the body’s ability to deliver oxygen to the tissues and results in symptoms of fatigue and shortness of breath. There are several types of anemia, each with different causes, ranging from blood loss, iron deficiency, damaged red blood cells, or issues with red blood cell production.
Oxygen saturation is a common measurement performed in health care settings, referring to the percentage of hemoglobin sites in erythrocytes carrying oxygen. Oxygen saturation is monitored using a device known as a pulse oximeter, which is commonly applied to a patient’s fingertip. This device works by sending two different wavelengths of light (red and infrared) through the finger and measuring the light with a photodetector as it exits. Hemoglobin absorbs light differentially depending upon its saturation with oxygen and presents the data as oxygen saturation (SpO2). Normal oxygen saturation readings range from 95–100 percent, with lower percentages reflecting hypoxemia (low levels of oxygen in the blood).
See the “Blood Disorders” section for more information on common types of anemia.
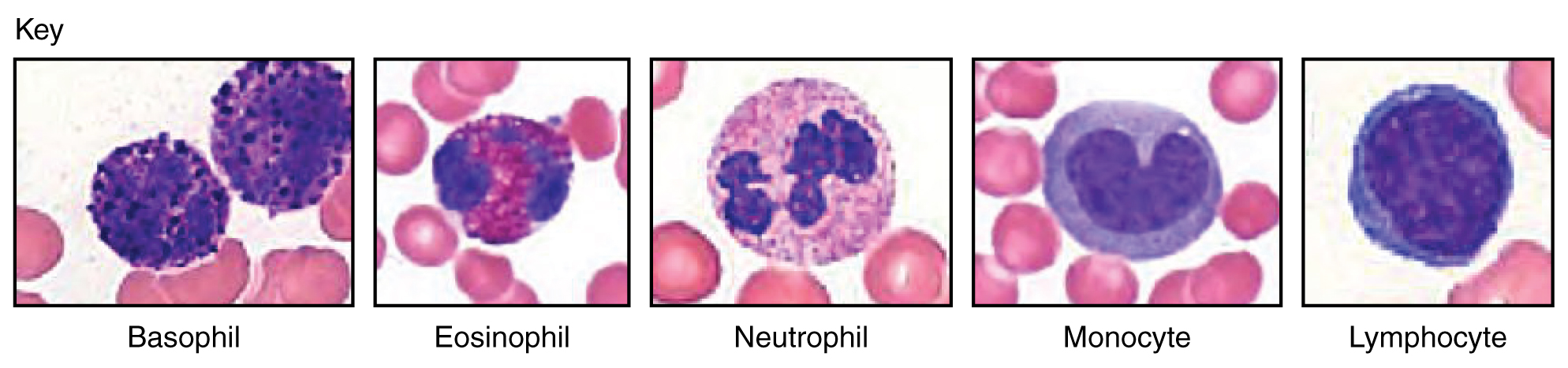
Leukocytes
Leukocytes, commonly known as white blood cells (WBCs), are essential components of the immune system. Leukocytes protect the body against invading microorganisms, as well as destroy cells with mutated DNA. There are several different types of leukocytes, including neutrophils, basophils, lymphocytes, monocytes, and eosinophils. See Figure 10.5[8] for an illustration of different types of leukocytes.
Characteristics of Leukocytes
Although leukocytes and erythrocytes both originate from hematopoietic stem cells in the red bone marrow, they are very different. Leukocytes are far less numerous but larger than erythrocytes. They are the only formed elements that are complete cells, meaning they possess a nucleus and organelles. Most leukocytes have a shorter life span than erythrocytes, some as short as a few hours or even a few minutes in cases of acute infection.
One of the most distinctive characteristics of leukocytes is their movement. While erythrocytes spend their days circulating within the blood vessels, leukocytes routinely leave the bloodstream to perform their defensive functions in the body’s tissues. For leukocytes, the vascular network is simply a highway they use to travel to and then exit at their destination. When they arrive, they are often given distinct names, such as macrophage or microglia, depending on their function.
After leukocytes have exited the capillaries, some take fixed positions in lymphatic tissue and bone marrow or the spleen, thymus, or other organs. Others will move about through the tissue spaces like amoebas, wandering freely or moving toward the direction in which they are drawn by chemical signals.
Classification of Leukocytes
Leukocytes can be divided into two groups based on whether their cytoplasm contains highly visible granules:
- Granular leukocytes contain abundant granules within their cytoplasm. They include neutrophils, eosinophils, and basophils.
- Agranular leukocytes have far fewer and less obvious granules. Agranular leukocytes include monocytes and lymphocytes.
Granular Leukocytes
Granulocytes are produced in the red bone marrow and have a short life span of hours to days. They typically have a lobed nucleus and are classified according to which type of stain best highlights their granules. See Figure 10.6[9] for an illustration of three types of granulocytes.
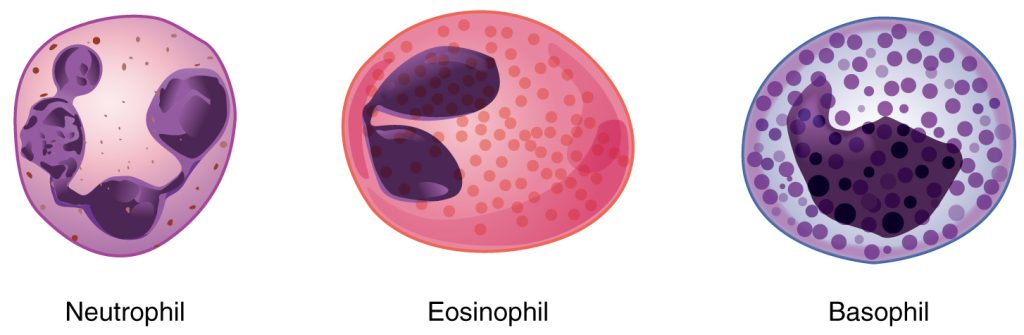
Neutrophils
The most common leukocytes are neutrophils, which comprise 50-70 percent of the total leukocyte count. They are 10–12 µm in diameter, much larger than erythrocytes. They are called neutrophils because their granules show up most clearly with stain that is chemically neutral (neither acidic nor basic).
Granules are present and numerous but have a fine, light lilac appearance. Their nuclei have a distinct lobed appearance and may have two to five lobes, with the number increasing based on the age of the cell. Older neutrophils have increasing numbers of lobes and are often referred to as polymorphonuclear (PMN), meaning a nucleus with many forms), or simply “polys.” Young and immature neutrophils begin to develop lobes and are known as “bands.”
Neutrophils are rapid responders to the site of infection and are efficient phagocytes with a preference for bacteria. Abnormally high counts of neutrophils indicate infection and/or inflammation, typically triggered by bacteria, but high counts are also found in patients with burns in order to fight off infection that can result from the destruction of the skin barrier. Low counts may be caused by high levels of stress and side effects of certain medications and increase an individual’s susceptibility to infection.
Eosinophils
Eosinophils typically make up about 2–4 percent of total leukocytes and are roughly 10–12 µm in diameter. The granules of eosinophils stain best with an acidic stain known as eosin, and if stained properly, the granules will have a distinct red to orange color. Their nucleus typically has two to three lobes.
The granules of eosinophils include enzymes that may counteract the activities of histamine, an inflammatory chemical produced by basophils and mast cells. Some eosinophil granules contain molecules that are toxic to parasitic worms that can enter the body through the skin or by consumption of raw or undercooked fish or meat. Eosinophils are also capable of phagocytosis. High eosinophil counts are typically caused by allergies, parasitic worm infestations, and some autoimmune diseases. Low counts may be due to drug toxicity and stress.
Basophils
Basophils are the least common leukocytes, typically making up less than one percent of the total leukocyte count. They are slightly smaller than neutrophils and eosinophils at 8–10 µm in diameter. The granules of basophils stain best with basic (alkaline) stain. Basophils contain large granules that pick up a dark blue stain and are so numerous they may make it difficult to see the two-lobed nucleus.
The granules of basophils release histamine that contributes to inflammation and heparin, which prevents blood clotting. High counts of basophils are associated with allergies, parasitic infections, and hypothyroidism. Low counts are associated with pregnancy, stress, and hyperthyroidism.
Agranular Leukocytes
Agranular leukocytes contain smaller, less-visible granules in their cytoplasm compared to granular leukocytes. The nucleus is simple in shape, sometimes with an indentation but without distinct lobes. There are two major types of agranulocytes: lymphocytes and monocytes.
Lymphocytes
Lymphocytes are the second most common type of leukocyte, accounting for about 20–30 percent of all leukocytes, and are essential for the immune response. The size range of lymphocytes is quite extensive, ranging from 6-17 µm. Refer back to Figure 10.6 for an illustration of lymphocytes.
The three major types of lymphocytes include natural killer cells, B cells, and T cells. Natural killer (NK) cells are capable of recognizing cells that do not express “self” proteins on their plasma membrane or that contain foreign or abnormal markers. These “nonself” cells include cancer cells, cells infected with a virus, and other cells with atypical surface proteins. Thus, they provide generalized, nonspecific immunity. NK cells are larger than other lymphocytes.
B cells and T cells, also called B lymphocytes and T lymphocytes, play prominent roles in defending the body against specific pathogens (disease-causing microorganisms) and are involved in specific immunity. One form of B cells (plasma cells) produces the antibodies or immunoglobulins that bind to specific foreign or abnormal components of plasma membranes. This is referred to as humoral immunity. Many types of T cells have been identified. One type of T cell (CD8 cell) provides cell-mediated immunity by physically attacking foreign or diseased cells. Another type of T cell (CD4) can either assist with cell-mediated immunity or humoral immunity. Other T cells serve as regulatory cells.
A memory cell is a variety of both B and T cells that forms after exposure to a pathogen to “remember” that pathogen and mount rapid responses during subsequent exposures. Unlike other leukocytes, memory cells live for many years.
B cells mature in the bone marrow, whereas T cells mature in the thymus. This site of maturation gives rise to the name B and T cells.
Abnormally high lymphocyte counts are characteristic of viral infections, as well as some types of cancer. Abnormally low lymphocyte counts are characteristic of prolonged (chronic) illness or immunosuppression, including that caused by HIV infection and drug therapies that often involve steroids.
Monocytes
Monocytes represent 2–8 percent of the total leukocyte count. They are typically easily recognized by their large size of 12–20 µm and indented or horseshoe-shaped nuclei. Refer back to Figure 10.6 for an illustration of monocytes.
Macrophages are monocytes that have left the circulation and phagocytize debris; foreign pathogens; worn-out erythrocytes; and many other dead, worn out, or damaged cells. Some macrophages stay in fixed locations, whereas others wander through the tissue fluid.
Abnormally high counts of monocytes are associated with viral or fungal infections, tuberculosis, and some forms of leukemia and other chronic diseases. Abnormally low counts are typically caused by suppression of the bone marrow.
View this learning activity[10] that contains images of different types of white blood cells with review questions: Wisc-Online White Blood Cells
Platelets
Platelets are referred to as thrombocytes. A platelet is not a whole cell, but rather a fragment of the cytoplasm of a cell called a megakaryocyte. Each megakaryocyte releases 2,000–3,000 platelets during its life span. Following platelet release, megakaryocyte remnants, which are little more than a cell nucleus, are consumed by macrophages. See Figure 10.7[11] for an illustration of platelet formation.
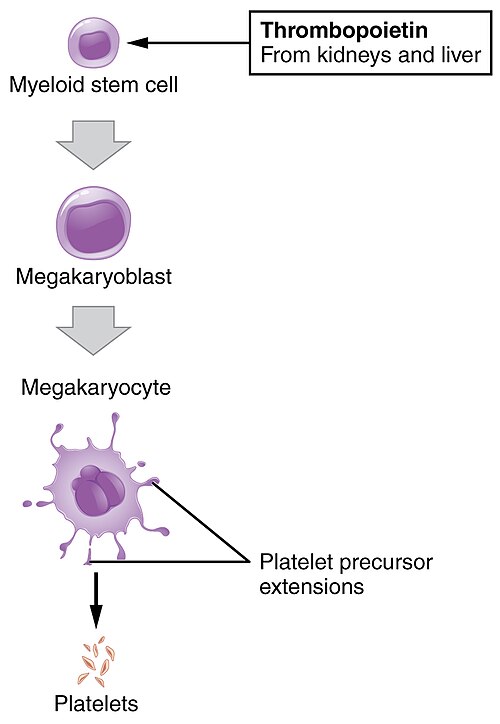
Platelets are relatively small, 2–4 µm in diameter, but numerous with typically 150,000–450,000 per µL of blood. After entering the circulation, approximately one third migrate to the spleen for storage for later release in response to any rupture in a blood vessel. When released, they become activated to perform their primary function, which is to limit blood loss. Platelets live only about ten days and then are phagocytized by macrophages.
Platelets are critical to hemostasis, the stoppage of blood loss following damage to a vessel. Hemostasis is further described in the following section. They also secrete a variety of growth factors essential for growth and repair of tissue, particularly connective tissue. Infusions of concentrated platelets are now being used in some therapies to stimulate healing.
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “Red_White_Blood_cells” by Electron Microscopy Facility at The National Cancer Institute at Frederick (NCI-Frederick) is in Public Domain. ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “Components_of_blood” by Alan Sved is licensed under CC BY -SA 4.0 ↵
- “1903_Shape_of_Red_Blood_Cells” by OpenStax College is licensed under CC BY 3.0 ↵
- “1901_Composition_of_Blood” by OpenStax College is licensed under CC BY 3.0 ↵
- “1916_Leukocyte_Key” by OpenStax College is licensed under CC BY 3.0 ↵
- “1907_Granular_Leukocytes” by OpenStax College is licensed under CC BY 3.0 ↵
- Liang, B. (n.d.). White blood cells [Video]. Wisc-Online. CC BY-NC 4.0. https://www.wisc-online.com/learn/general-education/anatomy-and-physiology1/ap17718/white-blood-cells ↵
- “1908_Platelet_Development” by OpenStax College is licensed under CC BY 3.0 ↵
Proteins that are unique to the plasma.
The most abundant plasma protein, made by the liver. It helps transport fatty acids and steroid hormones in the blood and maintains fluid balance.
The second most common type of plasma protein, making up about 38% of the total plasma protein volume.
Also called immunoglobulins, these are proteins that recognize and bind to specific antigens to help defend the body against pathogens.
Also called antibodies, these are proteins made by B cells that help the immune system recognize and fight antigens like bacteria and viruses.
A plasma protein produced by the liver that is essential for blood clotting, making up about 7% of plasma proteins.
Red blood cells responsible for oxygen transport.
An immature red blood cell that still contains some organelle remnants.
A protein in red blood cells that carries oxygen and contributes to skin color.
A blood test that measures the percentage of erythrocytes (RBCs) in a blood sample.
A thin, light-colored layer in a blood sample that contains white blood cells and platelets, usually less than 1% of the total blood volume.
The production of red blood cells (erythrocytes), stimulated by the hormone erythropoietin from the kidneys, occurring in red bone marrow at over 2 million cells per second.
A phagocytic cell in the bone marrow, liver, and spleen that removes worn-out red blood cells from circulation.
A device placed on the fingertip that measures oxygen saturation by using red and infrared light to detect how much oxygen is in the blood.
A condition where there are low levels of oxygen in the blood.
White blood cells involved in immune response.
White blood cells with many granules in their cytoplasm, including neutrophils, eosinophils, and basophils.
White blood cells with few or no visible granules, including monocytes and lymphocytes.
The most common white blood cells, making up 50–70% of all leukocytes.
Older neutrophils with a nucleus that has many lobes or shapes; often called “polys.”
White blood cells that make up about 2–4% of all leukocytes.
The least common leukocytes, typically making up less than one percent of the total leukocyte count.
The second most common type of leukocyte, accounting for about 20–30 percent of all leukocytes, and are essential for the immune response.
White blood cells that recognize and destroy cells lacking “self” proteins or containing foreign or abnormal markers, providing a rapid response to infected or cancerous cells.
White blood cells that defend the body against specific pathogens. A form of B cells called plasma cells produces antibodies.
White blood cells that help coordinate immune responses and play a key role in specific immunity.
A variety of both B and T cells that forms after exposure to a pathogen to “remember” that pathogen and mount rapid responses during subsequent exposures.
Large agranular white blood cells that circulate in the blood and migrate into tissues, where they mature into macrophages to engulf and digest pathogens and debris.
Platelets involved in blood clotting.
A large bone marrow cell that produces thrombocytes (platelets) by breaking off small fragments of its cytoplasm.
The process that stops bleeding by forming a blood clot at the site of a damaged blood vessel.

