15.3 Anatomy of the Urinary System
Anatomy of the Urinary System[1]
Kidneys
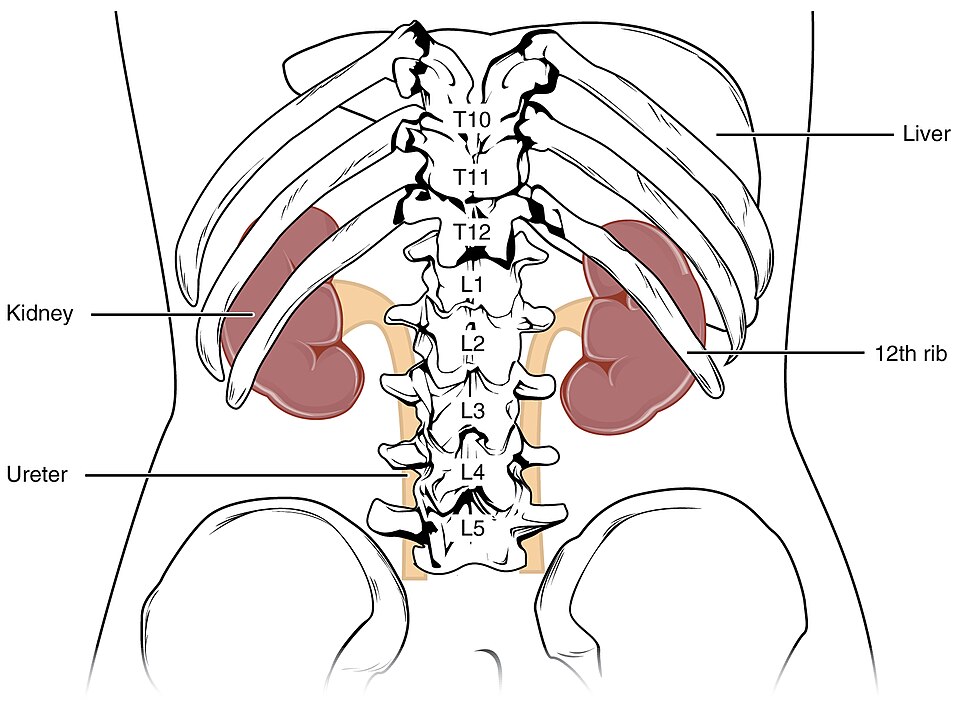
The urinary system has two kidneys, one on each side of the vertebral column in the retroperitoneal space. Each kidney is well-protected by muscle, fat, and ribs. The kidneys are roughly the size of a fist, with the male kidneys typically a bit larger than the female kidneys, weighing about 125–175 grams in males and 115–155 grams in females. They are about 11–14 centimeters (cm) in length, 6 cm wide, and 4 cm thick. The kidneys are well-vascularized, receiving about 25 percent of the cardiac output when a person is at rest. See Figure 15.3[2] for an illustration of the location of the kidneys.
The kidney is a complex organ with several external and internal features. These features will be discussed in more detail in the following subsections.
External Anatomy of the Kidneys
Renal Hilum
The renal hilum is the slight indentation on the medial side of each kidney where blood vessels, nerves, lymphatic vessels, and the ureters connect.
Layers Surrounding the Kidney
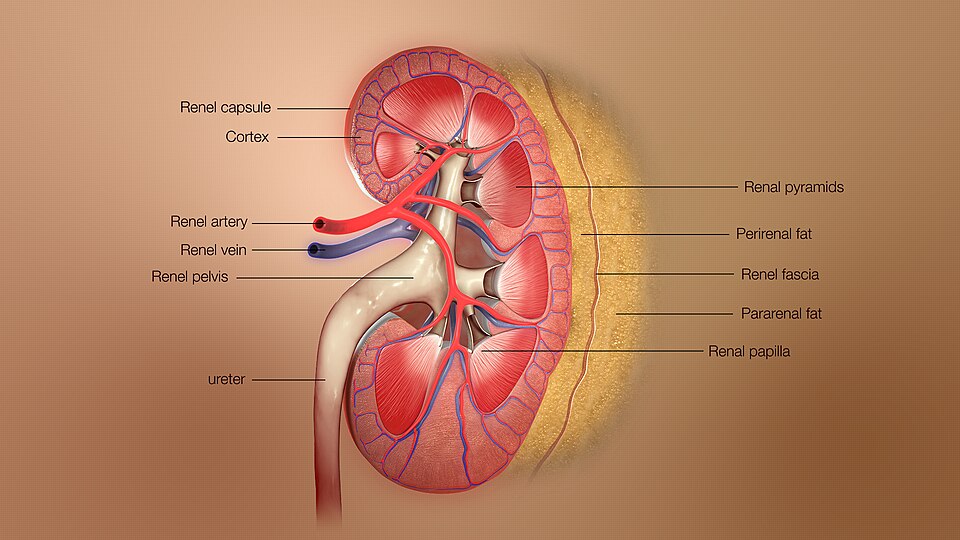
There are three layers of tissue surrounding each kidney. From deepest to superficial, the layers are the renal capsule, the adipose capsule, and the renal fascia.
The deepest layer is the renal capsule, a fibrous covering composed of dense, irregular connective tissue that protects the kidney and maintains its shape. This capsule is covered by a shock-absorbing layer of adipose tissue called the adipose capsule (renal fat pad), which is covered by a tough renal fascia. The fascia and the overlying peritoneum firmly anchor the kidneys to the posterior abdominal wall. See Figure 15.4[3] for an illustration of the layers around the kidneys.
Internal Anatomy of the Kidney
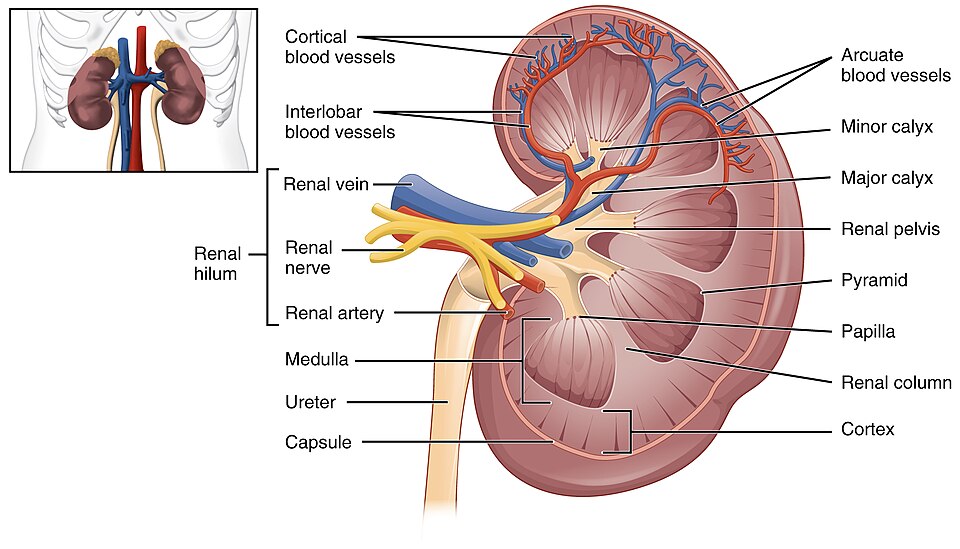
The internal anatomy of the kidney can be divided into an outer portion called the renal cortex and an inner portion called the renal medulla.
Renal Cortex
The outer region of the kidney is called the renal cortex. In a dissected kidney, it is easy to identify the cortex; it appears lighter in color compared to the rest of the kidney.
Renal Medulla
The inner region of the kidney is called the renal medulla. The renal medulla contains several important renal structures, including the renal columns, renal pyramids, and the renal papillae.
The renal columns are extensions of the renal cortex into the medulla to separate the most characteristic features of the medulla, the renal pyramids. The renal columns also divide the kidney into six to eight lobes and provide a supportive framework for vessels that enter and exit the cortex. The pyramids and renal columns together make up the kidney lobes.
The renal pyramids are six to eight cone-shaped tissues in the medulla of each kidney. The renal pyramids contain collecting ducts and some nephron loops, both of which will be described below.
At the medial tip of the pyramids are the renal papillae. The renal papillae are bundles of collecting ducts that transport urine to the calyces (collecting tubes) of the kidney to be excreted.
See Figure 15.5[4] for an illustration of the anatomy of the kidney.
Nephrons
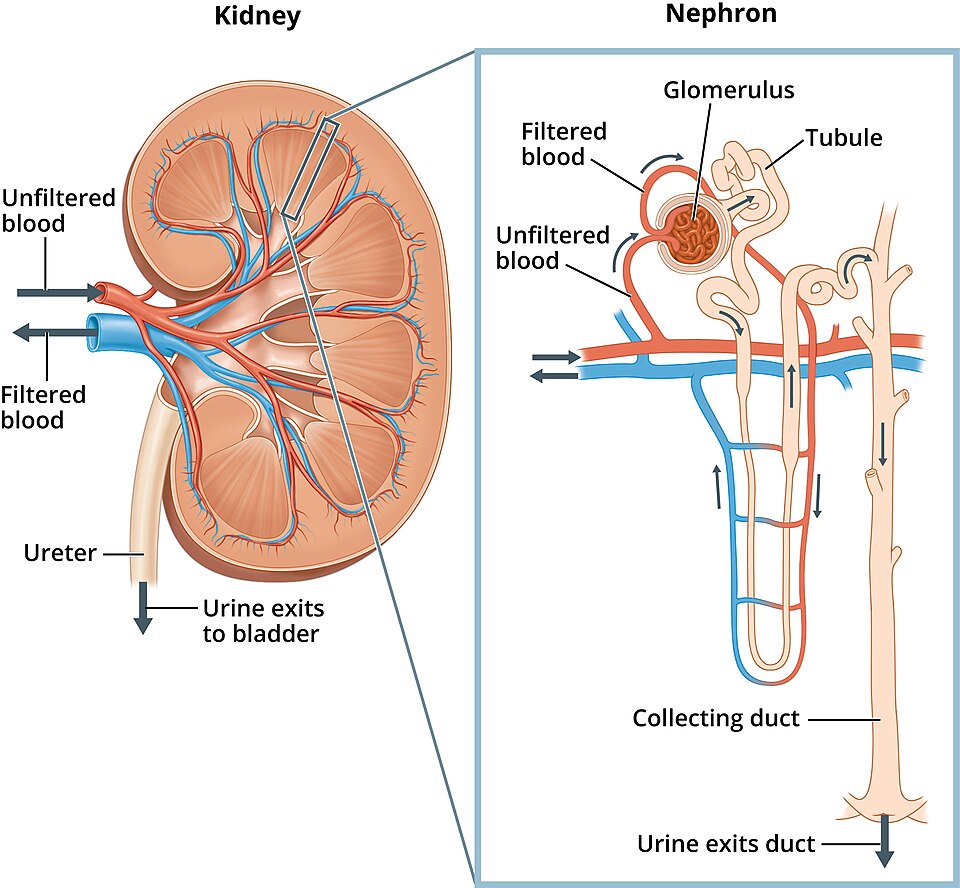
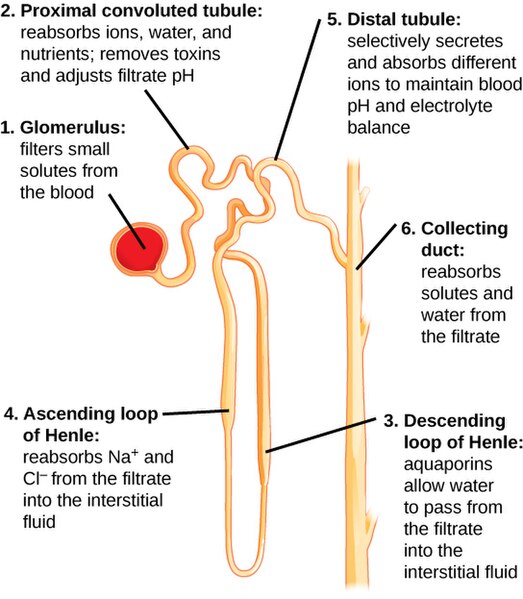
Nephrons are the “functional units” of the kidney. There are over 1.3 million nephrons in each kidney that clean and balance the blood. Nephrons take a simple filtrate from the blood and make it into urine. Many changes take place in the different parts of the nephron before urine is ready to leave the body. The nephron is divided into two main portions: the renal corpuscle and the renal tubule.
Renal Corpuscle
The renal corpuscle is a structure composed of two parts: the glomerulus and the glomerular capsule.
The glomerulus (plural = glomeruli) is a ball of capillaries at the beginning of each nephron that begins the filtration of blood. Blood pressure inside the glomerulus forces small substances out of the blood during a process called glomerular filtration. Blood enters the glomerulus through a very small afferent arteriole. This blood then flows through the glomerular capillaries, which have numerous holes called fenestrations. Water, wastes, and other small solutes that can fit through the fenestrations are pushed out of the glomerular capillaries and into the glomerular capsule forming filtrate.
The glomerular capsule (also known as Bowman’s capsule) surrounds the glomerulus and captures the filtrate being pushed out of the glomerular capillaries. The efferent arteriole carries the filtered blood away from the glomerulus.
See Figure 15.6[5] for an illustration of blood flow into and out of the kidney, nephron, and glomerulus.
Renal Tubule
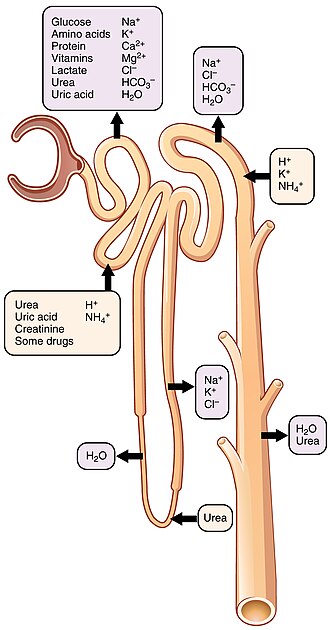
The renal tubule carries filtrate from the glomerular capsule to the collecting duct. It includes the proximal convoluted tubule (PCT), the nephron loop (loop of Henle), and the distal convoluted tubule (DCT). With up to 180 liters of filtrate per day passing through the nephrons of the kidney, most of that fluid and its solutes must be reabsorbed into the blood during a process called tubular reabsorption. This reabsorption occurs throughout the renal tubule. In addition, other substances need to be secreted into the renal tubule from the blood during a process called tubular secretion. See Figure 15.7[6] for an illustration of the reabsorption and secretion that occur throughout this tubule. Each portion of the nephron has a different capacity to reabsorb and secrete water and specific solutes.
Proximal Convoluted Tubule
The proximal convoluted tubule (PCT) is the first part of the renal tubule. It is called “convoluted” due to its coiled tube. Filtrate or filtered fluid collected by the glomerular capsule enters into the proximal convoluted tubule where some substances are reabsorbed and others are secreted. (Note that substances in the kidneys are “reabsorbed,” compared to being initially “absorbed” in the digestive tract.) About 99 percent of the water and most of the solutes filtered by the nephron are reabsorbed. Water and substances are reabsorbed into the blood of the peritubular and vasa recta capillaries surrounding the nephron.
Nephron Loop (Loop of Henle)
The nephron loop (also known as the loop of Henle) is a long single loop divided into descending and ascending portions. The descending and ascending portions of the loop are highly specialized to reabsorb much of the Na+ and water that were filtered out by the glomerulus. Some nephrons have short nephron loops that do not dip down beyond the cortex. These nephrons are called cortical nephrons. About 15 percent of nephrons have long nephron loops that extend deep into the medulla and are called juxtamedullary nephrons.
Distal Convoluted Tubule
The distal convoluted tubule (DCT) is the last part of the renal tubule. It connects the ascending nephron loop with the collecting duct. Approximately 80 percent of filtered water has been recovered by the time the filtrate enters the distal convoluted tubule. The distal convoluted tubule will recover another 10–15 percent before the filtrate enters the collecting ducts.
See Figure 15.8[7] for an illustration of the nephron structure, including the proximal convoluted tubule, the loop of Henle, and the distal convoluted tubule.
Juxtaglomerular Apparatus
Lying just outside the renal corpuscle is the juxtaglomerular apparatus (JGA). See Figure 15.9[8] for an illustration of the juxtaglomerular apparatus. At the junction where the afferent and efferent arterioles enter and leave the glomerular capsule, the first part of the distal convoluted tubule (DCT) comes into direct contact with the arterioles. The juxtaglomerular cells produce an enzyme called renin in response to decreased blood pressure or sympathetic nervous activity, which is an important part of a pathway called the renin-angiotensin-aldosterone system that increases blood pressure.

Collecting Ducts
The collecting ducts are continuous with the nephron but not technically part of it. Each collecting duct collects filtrate from several nephrons. Collecting ducts merge as they descend deeper into the medulla to empty at a renal papilla. Refer back to Figure 15.8 for an illustration of the collecting duct of a nephron.
Renal Calyces and Renal Pelvis
Filtrate drains from the collecting ducts into hollow tubelike cavities called minor calyces (singular = calyx), which merge together to form larger cavities called the major calyces. The major calyces then merge together to form the funnel-shaped renal pelvis. The renal pelvis narrows to become the ureter of each kidney. Refer back to Figure 15.5 for an illustration of the calyces and the renal pelvis.
Pathway of Urine (Formation to Excretion)
The pathway of urine after it is formed from filtrate in the nephron is it drains into the collecting duct and then into the renal papillae. From there, it drains into the minor and major calyces and then into the renal pelvis, the right and left ureters, the urinary bladder, the urethra, and eventually eliminated outside of body. See Figure 15.10 for an illustration of this pathway of urine from formation to excretion.
![Google. (2025) Gemini. [Artificial intelligence system]. https://gemini.google.com/app Urinary system pathway](https://wtcs.pressbooks.pub/app/uploads/sites/49/2025/06/Gemini_Generated_Image.png)
Blood Supply of the Kidney
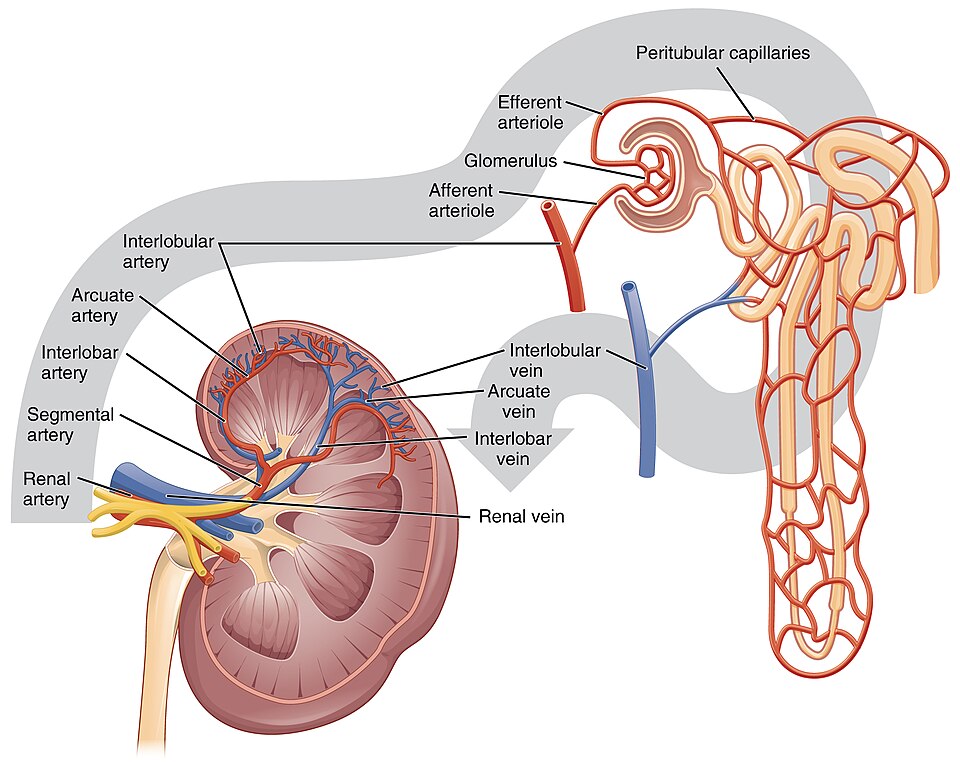
Oxygenated blood enters each kidney through the renal artery at the hilum. The renal artery divides into several branches of arteries that travel through the renal columns to reach the renal cortex. These arteries continue on to eventually branch into afferent arterioles that bring blood into the glomeruli of the 1.3 million nephrons in each kidney.
Blood leaves the glomeruli through the efferent arterioles and travels to the peritubular capillaries and vasa recta that surround the nephrons. Peritubular capillaries surround nephrons and parts of nephrons in the renal cortex, and vasa recta surrounds the nephron loop of juxtamedullary nephrons in the renal medulla. These capillaries connect to veins that continue to merge into the renal vein, which takes blood away from the kidney and back towards the heart.
See Figure 15.11[9] for an illustration of the blood supply to the kidney.
Steps of Urine Formation
Nephrons take a simple filtrate of the blood and modify it into urine. Different parts of the nephron utilize specific processes to produce urine. These processes include glomerular filtration, tubular reabsorption, and tubular secretion.
Glomerular Filtration
Blood pressure pushes blood through the glomerulus, filtering out water, wastes, and other small solutes that can fit through the fenestrations (holes) in the glomerular capillaries. These same fenestrations prevent filtration of blood cells and large plasma proteins, as they cannot fit through. The filtrate is then collected by the glomerular capsule and funneled to the proximal convoluted tubule. Filtrate is mostly water but also contains amino acids, glucose, various ions, and wastes.
Glomerular Filtration Rate
The volume of filtrate formed by both kidneys per minute is called the glomerular filtration rate (GFR). The heart pumps about 5 L blood per minute under resting conditions. Approximately 20 percent or one liter of this blood enters the kidneys to be filtered. On average, this liter results in the production of about 125 mL/min filtrate produced in males (range of 90 to 140 mL/min) and 105 mL/min filtrate produced in females (range of 80 to 125 mL/min). This amount equates to a volume of about 180 L/day in males and 150 L/day in females. Ninety-nine percent of this filtrate is returned to the circulation by reabsorption so that only about one to two liters of total urine are produced per day.
Estimated glomerular filtration rate (eGFR) is a blood test used to assess how well the kidneys are filtering waste and excess fluid from the blood. It is a calculated value based on creatinine level, age and sex of the patient, and other factors. Clinically, eGFR is used to diagnose and monitor chronic kidney disease (CKD), as well as to calculate appropriate drug dosages based on a patient’s kidney status.
Tubular Reabsorption
Many substances that were filtered out in the glomerulus are actually needed by the body. Most of these substances are reabsorbed into the blood from the proximal convoluted tubule. About 67 percent of the water, Na+, and K+ entering the nephron is reabsorbed in the PCT and returned to the circulation. Almost 100 percent of glucose, amino acids, and other organic substances such as vitamins are also reabsorbed here.
Water is reabsorbed by the process of osmosis and is directly affected by two hormones, aldosterone and ADH (antidiuretic hormone). Aldosterone, a hormone produced by the adrenal cortex, increases the reabsorption of Na+, which then increases the reabsorption of water. Antidiuretic hormone (ADH), a hormone released by the posterior pituitary gland, also increases the reabsorption of water. ADH exerts its effect farther along in the nephron at the distal collecting tubule and collecting duct. It influences how dilute or concentrated the final urine will be.
Tubular Secretion
Tubular secretion is the secretion of substances into the filtrate, which eventually becomes urine. For example, the cells of the proximal convoluted tubule actively secrete H+ into the urine to raise pH if the pH is too low. Other ions commonly secreted into the filtrate include potassium (K+) and ammonium (NH4+). Furthermore, some substances that need to leave the body may have been attached to proteins. Because proteins are too big to pass through the glomerular filtration membrane, they wouldn’t have been removed from the blood yet.
Other Organs of the Urinary System
Ureters
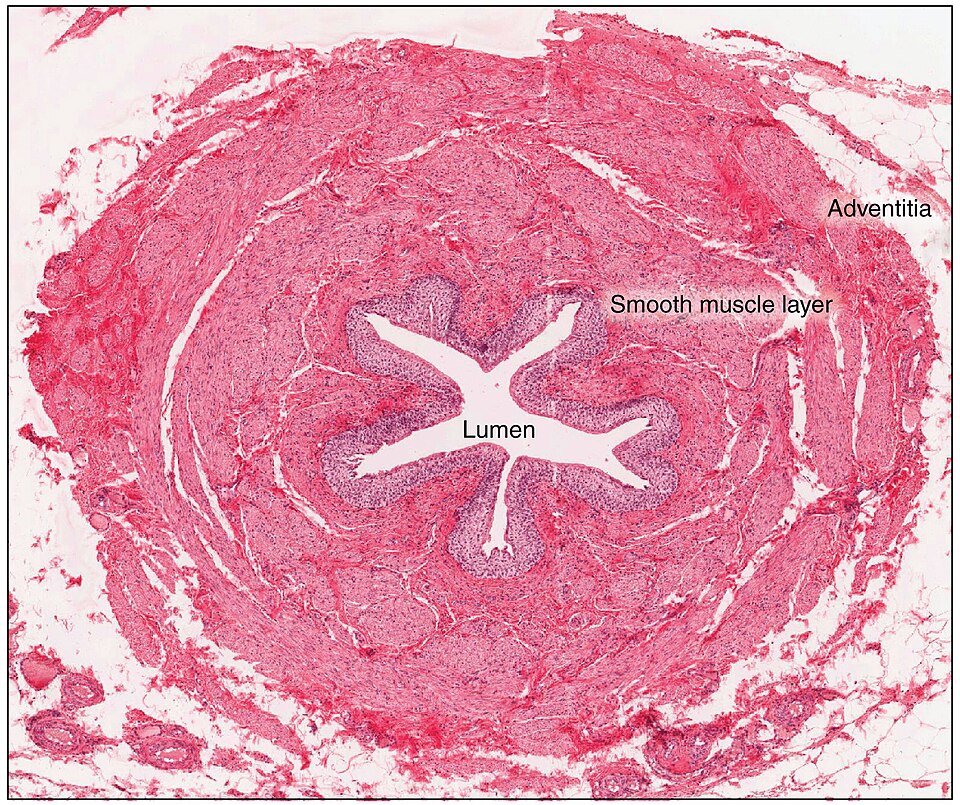
The ureters are long tubular structures that connect the renal pelvis of the kidney to the urinary bladder. Urine moves through the ureters by waves of peristalsis. The ureters enter the bladder obliquely or at an angle. This is important because it creates a one-way valve that allows urine into the bladder but prevents it from backing up into the ureter. The ureters are approximately 11 inches (30 cm) long.
The ureter’s inner mucosa is lined with transitional epithelium and scattered goblet cells that secrete protective mucus. The muscular layer of the ureter consists of smooth muscle cells that generate peristaltic contractions, moving urine toward the bladder independently of gravity. Finally, a loose adventitial layer composed of collagen and fat anchors the ureters between the parietal peritoneum and the posterior abdominal wall. See Figure 15.12[10] for an illustration of the walls of the ureters.
Urinary Bladder
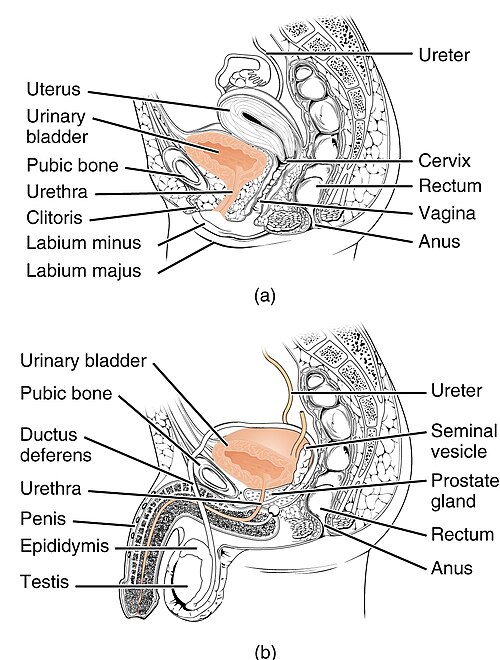
The urinary bladder collects urine from both ureters. The bladder lies anterior to the uterus in females and posterior to the pubic bone. During late pregnancy, its capacity is reduced due to compression by the enlarging uterus, resulting in increased frequency of urination. In males, the anatomy is similar, minus the uterus, and with the addition of the prostate inferior to the bladder. The bladder’s “dome” distends superiorly when the bladder is filled with urine.
The bladder is a highly expandable organ. The interior surface is made of a transitional epithelium that is ideal for the large volume fluctuations of the bladder. When empty, it resembles columnar epithelia, but when stretched, it “transitions” to a squamous appearance. Bladder volumes in adults can range from nearly zero to 500–600 mL.
See Figure 15.13[11] for an illustration of the urinary bladder and the bladder wall.
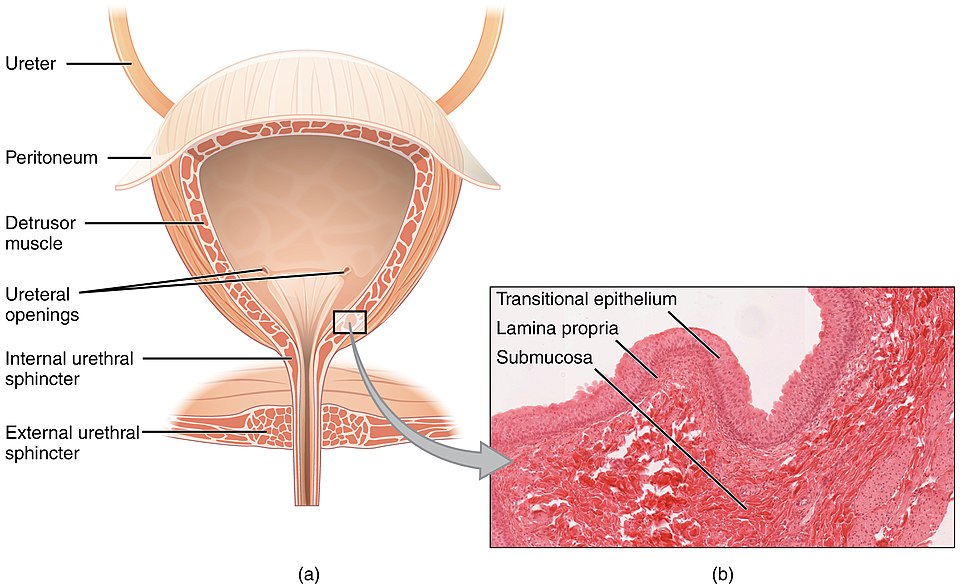
Urethra
The urethra transports urine from the bladder to the outside of the body. The urethra is the only organ of the urinary system that shows any significant difference between males and females; all other urine transport structures are identical. In the female, the external urethral orifice (opening) is anterior to the vaginal opening. Because the female urethra is relatively short – approximately 1.5 inches (4 cm) – it provides less of a barrier to bacteria compared to the longer male urethra, which helps explain the higher incidence of urinary tract infections (UTIs) in females. The male urethra passes through the prostate gland immediately inferior to the bladder before passing through the penis. The length of the male urethra varies among individuals but averages 7.8 inches (20 cm) in length. See Figure 15.14[12] for an illustration of the female and male urethras.
Urinating (voiding) is regulated by an involuntary internal urethral sphincter, consisting of smooth muscle and a voluntary skeletal muscle that forms the external urethral sphincter inferior to it. Control over the external urethral sphincter is learned with toilet training.
Urine
Blood is filtered through the glomeruli of the nephrons producing filtrate, which is transformed into urine at a relatively constant rate throughout the day. The amount of urine produced varies considerably, with the normal range from one to two liters per day. The kidneys must produce a minimum urine volume of about 500 mL/day to rid the body of wastes.
The characteristics of urine are influenced by water intake, exercise, environmental temperature, nutrient intake, and other factors. Urine is mostly water, so some of the characteristics such as color and odor are rough indicators of the state of hydration. Typically, the darker in color that urine is, the less water it contains. For example, after exercise or working outside and sweating, urine may turn darker and produce a slight odor, even if plenty of water has been consumed. Urine also contains ions like sodium and chloride, waste products such as urea and creatinine, and a pigment called urobilinogen. See Table 15.1 for a summary of urine characteristics.
Table 15.1. Normal Urine Characteristics[13]
| Characteristic | Normal Values |
|---|---|
| Color | Pale yellow to deep amber |
| Odor | Odorless |
| Volume | 750–2000 mL/24 hour |
| pH | 4.5–8.0 |
| Specific Gravity | 1.003–1.032 |
| Osmolarity | 40–1350 mOsmol/kg |
| Urobilinogen | 0.2–1.0 mg/100 mL |
| White Blood Cells | 0–2 HPF (per high-power field of microscope) |
| Leukocyte Esterase | None |
| Protein | None or trace |
| Bilirubin | <0.3 mg/100 mL |
| Ketones | None |
| Nitrites | None |
| Blood | None |
| Glucose | None |
There are also substances that urine should not contain, and their presence can indicate illness. The glomeruli filter blood based on particle size, so large elements like blood cells, platelets, antibodies, and albumin do not enter the filtrate and should not be present in the urine. Glucose and amino acids, while in filtrate, are reabsorbed in the proximal convoluted tubule and should not be present in urine. Some normal bacteria may be found in the urine from the natural biome of the body or contamination, but large amounts of bacteria should not be present.
The presence of leukocytes (white blood cells) in urine may indicate a urinary tract infection (UTI). Furthermore, leukocyte esterase is released by leukocytes, and if detected in the urine, it can be evidence of a UTI also. Protein does not normally leave the glomerular capillaries, so only trace amounts of protein should be found in the urine. If excessive protein is detected in the urine, it usually means that the glomerulus is damaged and is allowing protein to “leak” into the filtrate. The presence of red blood cells is abnormal in urine, although they may appear in female urine samples as a result of menstrual contamination. If red blood cells are present in urine, it can indicate a UTI or more serious conditions such as kidney stones, glomerulonephritis, or cancer.
Urine Color
The yellow color of urine is determined mostly by the breakdown products of red blood cell destruction and the hydration status of an individual. The “heme” of hemoglobin is converted by the liver and excreted indirectly into the urine, causing a yellow pigment called urochrome. If a person is well-hydrated, the diluted appearance may appear clear to light yellow, but as a person becomes more dehydrated and the urine is less dilute, this pigment causes a darker color of the urine. See Figure 15.15[14] for an illustration of a variety of urine colors.
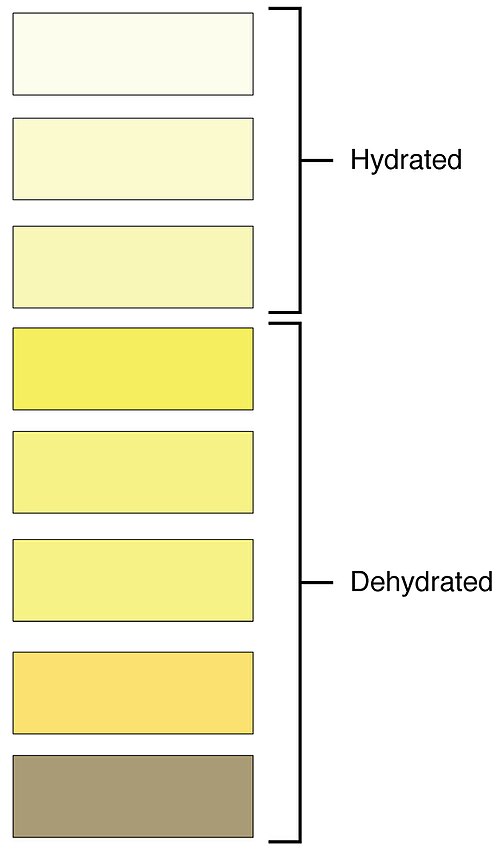
Urine color is also affected by a variety of other factors. Urine color can be affected by ingestion of certain foods like beets, berries, and fava beans. Bleeding from a kidney stone or cancer in the urinary tract may cause pink to bright red to brownish red urine. Small amounts of blood in the urine (called microscopic hematuria) won’t visibly change the color of the urine. Liver disease or obstruction of bile drainage from the liver can cause a dark orange or brown “tea” or “cola” hue to the urine.
Dehydration produces darker, concentrated urine that may also possess a slight odor of ammonia. Most of the ammonia produced from protein breakdown is converted into urea by the liver, so ammonia is rarely detected in fresh urine. However, if urine is exposed to the environment for a period of time, bacteria break down urea into ammonia. Interestingly, about one in five people detect a distinctive odor in their urine after consuming asparagus; other foods such as onions, garlic, and fish can pass on their own aromas. These food-caused odors are harmless.
pH of Urine
The pH of the urine can vary from a normal low of 4.5 to a maximum of 8.0. Dietary intake can influence urinary pH, with meats lowering pH but citrus fruits, vegetables, and dairy products raising the pH. Chronically high or low pH can lead to disorders, such as the development of kidney stones.
Specific Gravity of Urine
Specific gravity is a measure of the number of solutes per unit volume of a solution and is traditionally easier to measure than osmolarity. Urine will always have a specific gravity greater than pure water (water = 1.000) due to the presence of solutes. Laboratories can now measure urine osmolarity directly, which is a more accurate indicator of urinary solutes than specific gravity. Remember that osmolarity is the number of osmoles or milliosmoles per liter of fluid (mOsmol/L). Urine osmolarity ranges from a low of 50–100 mOsmol/L to as high as 1,200 mOsmol/L H2O.
Ketones
Ketones are produced when the body burns fat. Ketones in the urine suggests that the body is using fat as an energy source instead of glucose. For example, ketones may appear in the urine if a person has a severe lack of carbohydrate intake or is experiencing starvation. Individuals with type 1 diabetes mellitus may also have excessive ketones in their urine. When their pancreas does not produce insulin, their cells cannot use the glucose in their bloodstream. The cells are forced to use fat as their energy source, which produces ketones as a byproduct. Consequently, glucose will likely be present in the urine as well.
Urinalysis
Urinalysis is a diagnostic lab test used to analyze the composition of urine and check for abnormalities that could indicate infection or disease.
Micturition
Micturition is the medical term for urination (voiding) or emptying the bladder. The bladder can hold up to 500–600 mL of urine. When bladder volume reaches about 150 mL, an urge to void is sensed. As the bladder continues to fill, subsequent urges become harder to ignore. Voluntary control of urination relies on consciously preventing relaxation of the external urethral sphincter to maintain urinary continence. Incontinence is a loss of control of urination. Read more about incontinence in the “Disorders of the Urinary System” section.
View a supplementary YouTube video[15] on the excretory system and the nephron: Excretory System and the Nephron.
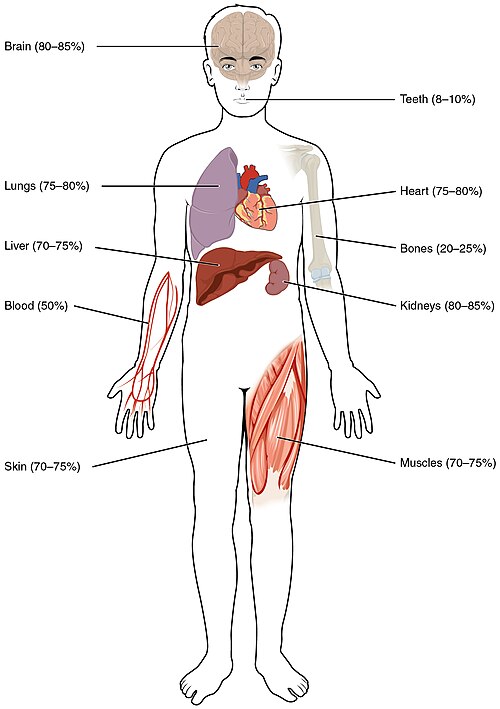
Body Fluid Balance
Our body composition is mostly water, ranging from about 75 percent of body mass in infants to about 50 to 60 percent in adults, to as low as 45 percent in older adults. The percent of body water changes with the body’s development because the proportions of the body given to each organ and to muscles, fat, bone, and other tissues change from infancy to adulthood. The brain and kidneys have the highest water content, with water making up 80–85 percent of their total mass. In contrast, teeth have the lowest proportion of water with about 8–10 percent of water. See Figure 15.16[16] for an illustration of the body’s water content.
Fluid Intake and Output
On a typical day, an average adult takes in about 2,500 milliliters (mL) of fluids (equal to about 3 quarts). Although most of the intake is absorbed from fluids and foods in the digestive tract, about 230 mL (8 ounces) per day is generated metabolically in the last step of aerobic respiration.
About the same volume (2,500 mL) of water leaves the body daily, with most eliminated as urine. This amount is called sensible water loss because a person is aware of it and the amount can be measured. Water is also lost through the skin by sweating, and a small amount is eliminated through feces and menstruation. Some water is also lost through water vapor in the air exhaled from the lungs. These types of water loss are called insensible water loss because a person is unaware of it.
To maintain homeostasis in the body, the amount of fluid intake must equal fluid output. If adequate fluids are not consumed or if too many fluids are lost from the body, dehydration can occur. A person who repeatedly vomits or has diarrhea may also become dehydrated. Infants, because their body mass is so low, can become dangerously dehydrated very quickly. Other populations at a higher risk of dehydration include the elderly, those with altered mental states, and individuals with significant medical conditions. Dehydration can be a medical emergency as blood volume and blood pressure decreases, impacting blood flow to vital organs. A severely dehydrated person may lose consciousness, become comatose, or die if their body is not rehydrated quickly.
Acid-Base Balance
The pH of human blood normally ranges from 7.35 to 7.45. Homeostatic mechanisms normally keep the pH of blood within this narrow range. This is critical, because fluctuations—either too acidic or too alkaline—can be life-threatening.
Buffers
Buffers in the human body maintain a normal range of pH of body fluids. A buffer is a substance that resists a change in pH when a small amount of acid or base is added to it. The three major buffers used by the body include proteins (hemoglobin and albumin), phosphates, and bicarbonate. The bicarbonate buffer is the primary buffering system of the blood and interstitial fluid in tissues throughout the body. It is a very powerful and fast-acting buffer that is produced and reabsorbed by the kidneys. Additionally, nearly all proteins can function as buffers and account for two thirds of the buffering power of the blood and most of the buffering within cells. Lastly, the phosphate buffer system has a high concentration of phosphates in the intracellular fluid to resist pH changes inside the cells.
Acidosis
A person whose blood pH is below 7.35 is considered to be in acidosis. Acidosis depresses the central nervous system and has several symptoms, including headache, confusion, lethargy, and fatigue. A sustained blood pH below 7.0 can be fatal.
Common causes of acidosis are respiratory disorders and situations that impair breathing, resulting in the buildup of CO2 (and H+) in the bloodstream. Acidosis can also be caused by metabolic problems that promote the production of acids or reduce the function of buffers that act as bases. For example, people with undiagnosed or poorly managed type 1 diabetes mellitus don’t have enough insulin for their cells to use glucose, and, therefore, produce ketones as their body breaks down fats for energy instead. As ketones build up in their blood, a life-threatening condition called diabetic ketoacidosis can develop. Kidney failure can also cause metabolic acidosis when the kidneys lose their ability to eliminate H+ ions and produce bicarbonate. People with severe diarrhea can lose excessive amounts of bicarbonate, allowing acids to build up in body fluids.
Alkalosis
A person with a blood pH above 7.45 is considered to be in alkalosis. Alkalosis overstimulates the nervous system and symptoms include cognitive impairment (which can progress to unconsciousness), tingling or numbness in the extremities, muscle twitching and spasm, and nausea and vomiting. A blood pH above 7.8 is fatal.
Respiratory alkalosis is commonly caused by hyperventilation, resulting in the excessive release of carbon dioxide by the lungs and reduced concentration of H+ ions in the blood. Metabolic alkalosis can be caused from prolonged, severe vomiting due to a loss of hydrogen ions (as components of HCl acid). Medications such as diuretics can also cause alkalosis as increased urination causes the body to lose excessive potassium ions. Antacids, too, can potentially cause alkalosis if a person takes them in excessive amounts for persistent heartburn or an ulcer.
See Figure 15.17[17] for an illustration of the symptoms of acidosis and alkalosis.

- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2608_Kidney_Position_in_Abdomen” by OpenStax College is licensed under CC BY 3.0 ↵
- “3D_Medical_Animation_depicting_Kidney_Layers.jpg” by https://www.scientificanimations.com is licensed under CC BY-SA 4.0 ↵
- “2610_The_Kidney” by OpenStax College is licensed under CC BY 3.0 ↵
- “Kidney_and_Nephron” by National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health is licensed under CC0, Public Domain ↵
- “2618_Nephron_Secretion_Reabsorption” by OpenStax College is licensed under CC BY 3.0 ↵
- “Figure 41 03 04.jpg” by CNX OpenStax is licensed under CC BY 4.0 ↵
- ”2615_Juxtaglomerular_Apparatus” by OpenStax Anatomy and Physiology is licensed under CC BY 4.0 ↵
- “2612_Blood_Flow_in_the_Kidneys” by OpenStax College is licensed under CC BY 3.0 ↵
- “2607_Ureter” by OpenStax College is licensed under CC BY 3.0 ↵
- “2605_The_Bladder” by OpenStax College is licensed under CC BY 3.0 ↵
- “Female_and_Male_Urethra.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “2601_Urine_Color_Chart.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Amoeba Sisters. (2022, August 10). Excretory system and the nephron [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=q5qaGHfdmYM ↵
- “2701_Water_Content_in_the_Body-01” by OpenStax College is licensed under CC BY 3.0 ↵
- “2716_Symptoms_of_Acidosis_Alkalosis” by OpenStax College is licensed under CC BY 3.0 ↵
The slight indentation on the medial side of each kidney where blood vessels, nerves, lymphatic vessels, and the ureters connect.
A tough, fibrous outer covering of the kidney that protects it from trauma and infection.
A shock-absorbing layer of adipose tissue.
A layer of connective tissue that anchors the kidneys to surrounding structures and helps maintain their position in the abdominal cavity.
The outer region of the kidney.
Extensions of cortical tissue that separate renal pyramids in the medulla, divide the kidney into lobes, and support blood vessels entering and exiting the cortex.
Six to eight cone-shaped tissues in the medulla of each kidney.
Functional units of the kidney that filter blood and convert the filtrate into urine.
A structure composed of two parts: the glomerulus and the glomerular capsule.
A ball of capillaries at the beginning of each nephron that begins the filtration of blood.
Surrounds the glomerulus and captures the filtrate being pushed out of the glomerular capillaries (Also known as Bowman’s capsule).
Carries the filtered blood away from the glomerulus.
The process by which the nephron returns water and solutes from the filtrate back into the blood.
The process by which substances are moved from the blood into the filtrate in the kidney tubules to be eliminated in urine.
The first, coiled section of the kidney's renal tubule where initial filtration and reabsorption of substances from urine occurs.
A U-shaped portion of the kidney tubule with descending and ascending parts that reabsorbs sodium and water from filtered urine.
The final coiled section of the kidney tubule that connects the nephron loop to the collecting duct and fine-tunes urine composition.
A specialized structure in the kidney where blood vessels and tubules meet that produces renin to help regulate blood pressure.
A blood vessel that branches off from the abdominal aorta and supplies oxygen-rich blood to the kidneys.
Small blood vessels that carry blood into the glomeruli (filtering units) of the kidney's nephrons.
Small blood vessels that carry blood away from the glomeruli to capillaries surrounding the nephrons.
Tiny blood vessels that surround nephrons in the kidney's outer region (cortex) for exchange of substances.
Straight blood vessels that surround the nephron loops in the kidney's inner region (medulla).
The volume of filtrate produced by both kidneys per minute, normally about 125 mL/min in males and 105 mL/min in females.
A blood test that calculates how well the kidneys are filtering waste based on creatinine levels, age, and sex to diagnose kidney disease.
The main mineralocorticoid hormone that helps balance sodium and potassium levels and controls blood pressure and volume.
A hormone released by the posterior pituitary that helps the body retain water when blood osmolality is high, such as during dehydration.
A type of epithelium that can stretch and change shape.
The tube that carries urine from the bladder to the outside of the body, with structural differences between males and females.
An involuntary smooth muscle that automatically controls the release of urine from the bladder.
A voluntary skeletal muscle below the internal sphincter that provides conscious control over urination.
A measure of the concentration of dissolved substances in urine compared to pure water, indicating how concentrated the urine is.
Substances produced when the body burns fat for energy instead of glucose, detected in urine during conditions like diabetes or fasting.
A diagnostic laboratory test that examines urine composition to detect infections, diseases, or other health abnormalities.
The medical term for urination or emptying the bladder, which begins when bladder volume reaches about 150 mL.
Water loss from the body that a person is aware of and can measure, mainly through urine production.
Water loss from the body that a person is unaware of, such as through breathing, sweating, and skin evaporation.
A condition in which the body loses more water than it takes in, affecting skin elasticity.
A solution that resists changes in its pH when small amounts of an acid or base are added to it.
Low pH.
Elevated pH.

