13.4 Pulmonary Ventilation (Breathing)
Pulmonary Ventilation (Breathing)[1]
Pulmonary ventilation is the act of breathing. It consists of inhalation (also called inspiration), which is the movement of air into the lungs, and exhalation (also called expiration) or movement of air out of the lungs.
Mechanism of Breathing
The ability to breathe—to have air enter the lungs during inspiration and air leave the lungs during expiration—is dependent on the air pressure of the atmosphere and the air pressure within the lungs. Air always moves from an area of higher pressure to an area of lower pressure.
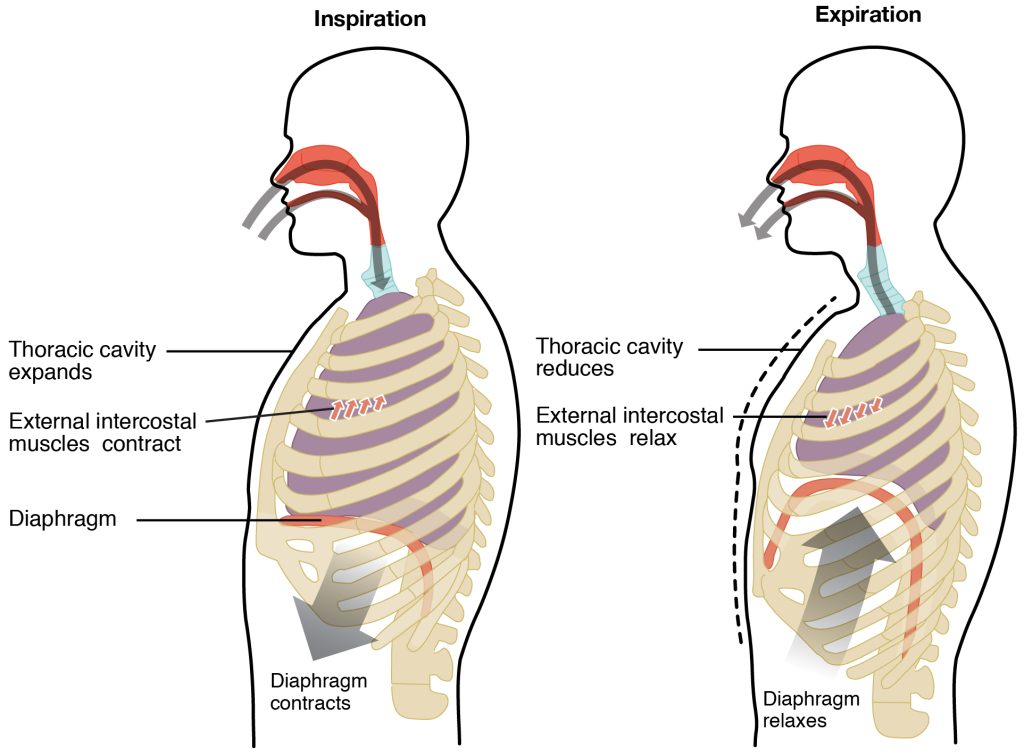
Atmospheric pressure remains constant, but the air pressure within the lungs changes with every breath. During inhalation, the body creates a pressure difference, making the air pressure inside the alveoli less than atmospheric pressure, so that air flows into the lungs. In general, two muscle groups are used during normal inspiration: the diaphragm and the external intercostal muscles. Additional muscles can be used if a bigger breath is required. When the diaphragm contracts during inspiration, it flattens, creating a larger volume in the thoracic cavity and more space for the lungs. Contraction of the external intercostal muscles elevates the rib cage, moving the ribs upward and outward, causing the rib cage to expand, which also increases the volume of the thoracic cavity. The increasing size of the thoracic cavity forces the lungs to stretch and expand as well. This increase in volume leads to a decrease in the pressure inside the alveoli, creating a pressure lower than atmospheric pressure. As a result, air flows into the lungs. Air will flow into the lungs until the air pressure equalizes, and then the muscles will begin to relax with expiration.
Air flows out of the lungs during exhalation based on the same principle. Pressure in the lungs becomes higher than the atmospheric pressure, so air flows out. The process of normal expiration is passive; therefore, no energy is required to push air out of the lungs. Instead, the elasticity of the lung tissue causes the lung to recoil as the diaphragm and intercostal muscles relax following inspiration. This relaxation causes the thoracic cavity and lungs to decrease in volume, causing an increase in the pressure higher than atmospheric pressure. Air then flows out of the lungs. See Figure 13.13[2] for an illustration of inspiration and expiration.
Ventilation Control Centers
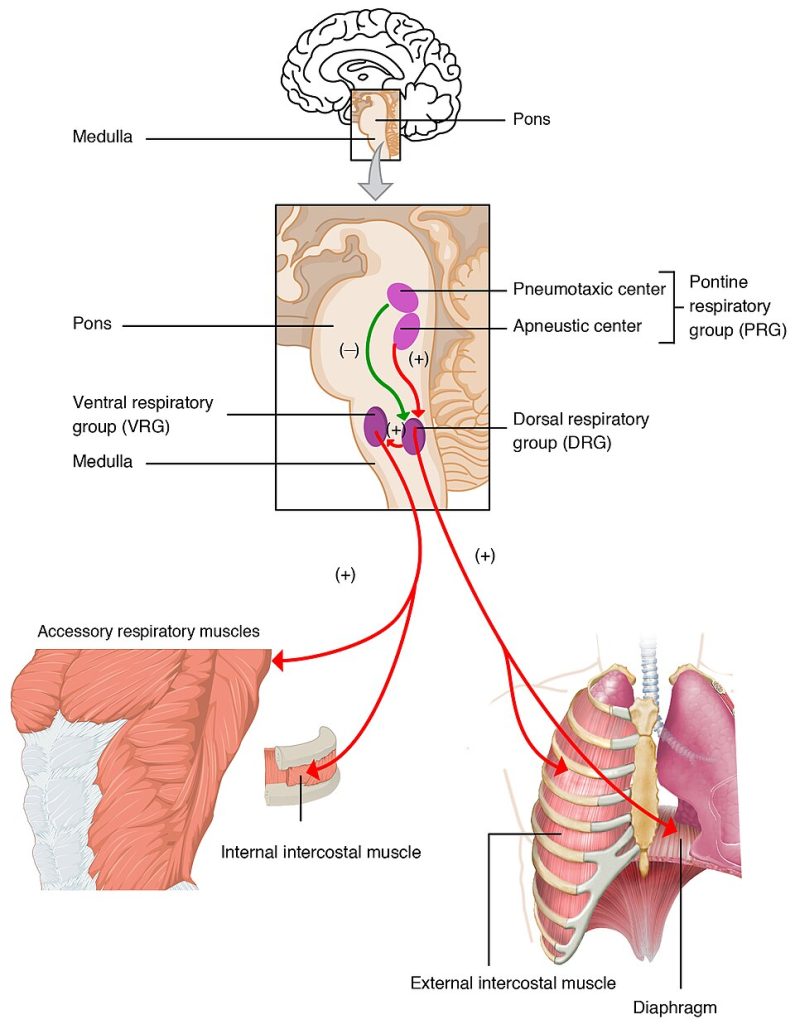
The control of ventilation is complex and relies on multiple regions of the brain to coordinate the activation of respiratory muscles to initiate contraction. The result is typically a rhythmic, consistent respiratory rate that provides the body with sufficient amounts of oxygen, while adequately removing carbon dioxide.
The major brain centers involved in pulmonary ventilation are the medulla oblongata and the pons. See Figure 13.14[5] for an illustration of the respiratory centers in the brain.
Respiratory Rate
The respiratory rate is the total number of breaths that occur each minute. The normal respiratory rate in adults is 12 to 20 breaths per minute. The normal respiratory rate for children under 1 year of age is 30 to 60 breaths per minute, but by the time a child is about 10 years old, the normal rate is closer to 18 to 30.
Respiratory rate can be an important indicator of health, as the rate may increase or decrease during illness. The respiratory rate is regulated by the respiratory center located within the medulla oblongata and pons in the brain, which respond primarily to changes in carbon dioxide and pH levels in the blood. There is also some voluntary control over breathing such as holding one’s breath or taking a big breath before diving into a pool.
Breathing Patterns
A normal breathing pattern in adults follows rhythmic inhalations and exhalations of 12-20 breaths per minute. There are several medical terms for patterns of breathing:
- Apnea: Temporary pauses in breathing
- Bradypnea: Slow breathing
- Dyspnea: Shortness of breath
- Eupnea: Normal, effortless breathing
- Tachypnea: Rapid breathing
Lung Volumes and Capacities
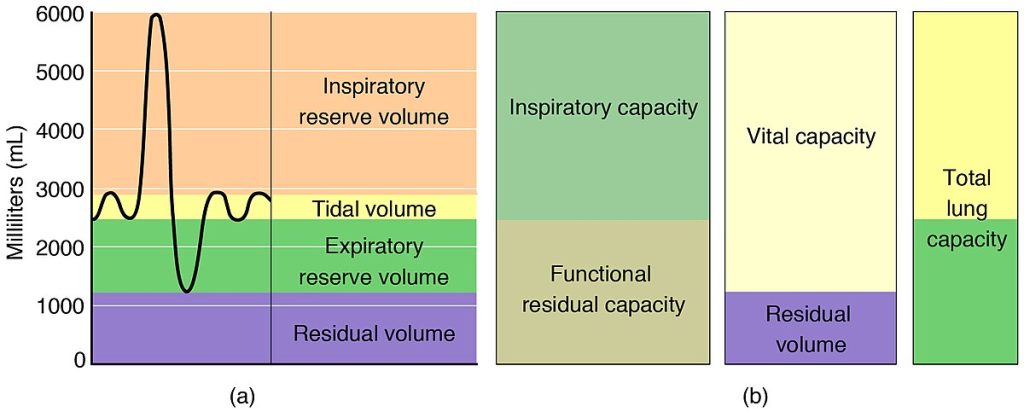
Lung volume is a medical term used for various volumes of air moved by the lungs at a given point of the respiratory cycle, including the following:
- Tidal volume (TV) is the amount of air inhaled or exhaled in a normal quiet breath, which averages about 500 milliliters (mL) for a healthy male adult and 400 mL for a healthy female adult.[6]
- Inspiratory reserve volume (IRV) is the extra volume of air that can be forcibly inhaled after a normal inhalation, about 3,100 mL.
- Expiratory reserve volume (ERV) is the extra amount of air that can be forcibly exhaled after a normal exhalation, about 12 mL.
- Residual volume (RV) is the air left in the lungs after exhaling as much air as possible, averaging about 1,200 mL. Residual volume prevents alveoli from collapsing and makes breathing easier. For example, consider the effort it takes to blow up a new balloon compared to a balloon that already has some air inside of it. In the second scenario, it is easier to inflate the balloon.
- Total lung capacity (TLC) is the sum of all lung volumes (TV ERV IRV RV), which represents the total amount of air a person can hold in their lungs after a forceful inhalation. TLC is about 6,000 mL of air for males, and about 4,200 mL for females.
- Vital capacity (VC) is the amount of air a person can move into or out of their lungs, which is the sum of all the previous volumes described except residual volume (TV ERV IRV) and is between 4,000 and 5,000 milliliters for adults.
See Figure 13.15[7] for an illustration of respiratory volumes and capacities.
Gas Exchange
Gas exchange occurs in two main locations in the body: the lungs, where oxygen diffuses into the blood and carbon dioxide diffuses out of the blood and is exhaled; and in the tissues, where oxygen diffuses out of the blood into the tissues and carbon dioxide diffuses out of the tissues and into the blood. External respiration (or alveolar gas exchange) is the exchange of gases between the alveoli and the pulmonary capillaries. Internal respiration (or systemic gas exchange) is the exchange of gases between the systemic capillaries and the tissues.
The actual exchange of gases occurs due to simple diffusion. Energy is not required to move oxygen or carbon dioxide across membranes. Instead, these gases follow pressure gradients that allow them to diffuse from higher concentration to lower concentration.
Oxygen Transport in the Blood
Although oxygen is transported in the blood, it has limited solubility in plasma. A small amount of oxygen dissolves in the blood and is transported in the blood plasma, but this amount represents only about 1.5% of the total amount. The majority of oxygen molecules are carried from the lungs to the body’s tissues by hemoglobin in erythrocytes (red blood cells).
Heme is the portion of hemoglobin that contains iron and binds oxygen. Each hemoglobin molecule contains four iron-containing heme molecules, so one hemoglobin molecule can carry four molecules of oxygen. If a hemoglobin molecule is carrying four molecules of oxygen, it is considered saturated. A hemoglobin saturation of 100 percent means that every heme unit in all erythrocytes of the body is bound to oxygen. In a healthy individual with normal hemoglobin levels, hemoglobin saturation generally ranges from 95 percent to 99 percent.
See Figure 13.16[8] for an illustration of an erythrocyte and hemoglobin.
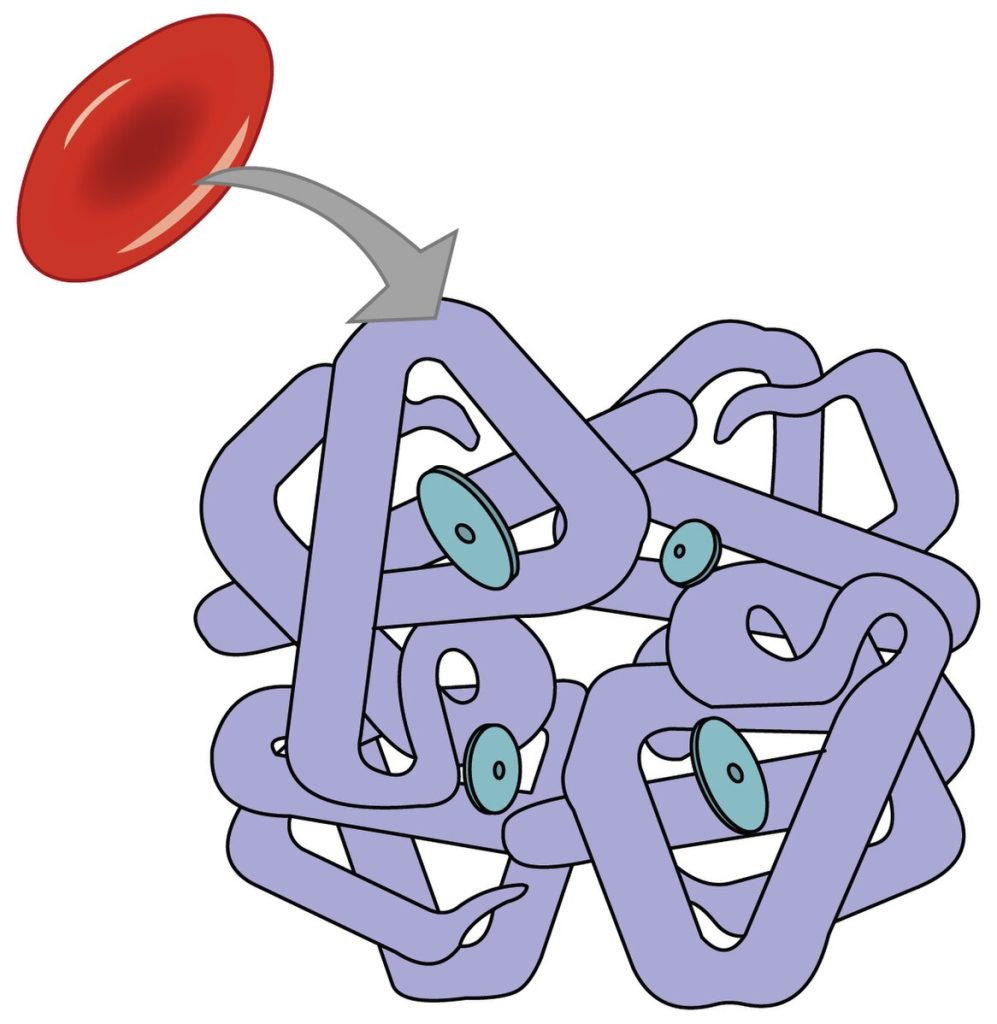
When oxygen diffuses from the alveoli into the pulmonary capillaries, it diffuses into the red blood cell and binds to hemoglobin forming oxyhemoglobin (HbO2). Oxyhemoglobin is a bright, red-colored molecule that contributes to the bright red color of oxygenated blood.
Oxygen is transported in the bloodstream and released in tissues based on their metabolic demand. For example, during exercise, more oxygen is needed by the skeletal muscles, so more oxygen is released by the hemoglobin.
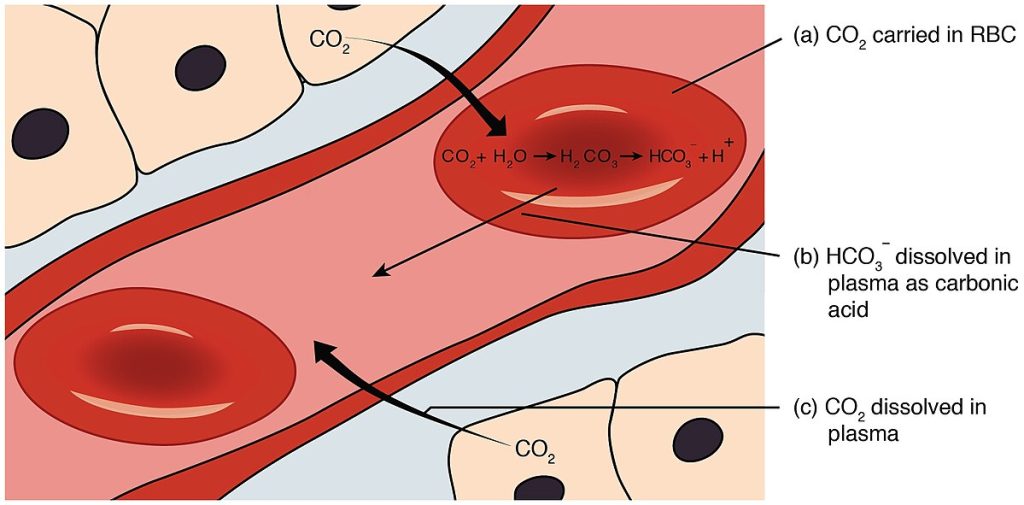
Carbon Dioxide Transport in the Blood
Carbon dioxide (CO2) is transported in the blood in three different ways: converted to bicarbonate ions, bound to hemoglobin as carbaminohemoglobin, and dissolved directly in the plasma.
- Bicarbonate: The majority of carbon dioxide (about 75%) is transported in the blood as bicarbonate (HCO3–) ions. CO2 diffuses into red blood cells, where a chemical reaction converts it to bicarbonate. Bicarbonate is transported in the bloodstream to the lungs, where a reverse reaction occurs in the red blood cells and CO2 is exhaled.
- Carbaminohemoglobin: About 20% of carbon dioxide binds to hemoglobin in red blood cells, forming carbaminohemoglobin. Carbon dioxide does not bind to iron as oxygen does but instead binds on the globin portions of hemoglobin. The red blood cells are transported in blood to the pulmonary capillaries, where carbon dioxide dissociates from hemoglobin and diffuses into the alveoli and is exhaled.
- Dissolved in Plasma: A small amount of carbon dioxide (about 5%) dissolves directly in the plasma and travels to the pulmonary capillaries where it diffuses into the alveoli and is exhaled.
See Figure 13.17[9] for an illustration of the three methods of carbon dioxide transport in the blood.
View a supplementary YouTube video[10] review of the respiratory system: Respiratory System
- Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2022). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction ↵
- “5ae96ca57ec74c0100efe6d029917e51d981c5e2” by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/22-3-the-process-of-breathing ↵
- A.D.A.M.. (2025, January 1). Breathing [Video]. MedlinePlus. All rights reserved. https://medlineplus.gov/ency/anatomyvideos/000018.htm ↵
- Educational Videos. (2010, May 4). Breathing movements - inspiration, expiration, mechanism of breathing [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=Mf8xTqfspp4 ↵
- “2327_Respiratory_Centers_of_the_Brain” by OpenStax College is licensed under CC BY 3.0 ↵
- Hallett, S., Toro, F., & Ashurst, J. V. (2025). Physiology, tidal volume. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482502/ ↵
- “2317_Spirometry_and_Respiratory_Volumes” by OpenStax College is licensed under CC BY 3.0 ↵
- “2322_Fig_23.22-a” by OpenStax College is licensed under CC BY 3.0 ↵
- “2325_Carbon_Dioxide_Transport” by OpenStax College is licensed under CC BY 3.0 ↵
- Amoeba Sisters. (2022, February 28). Respiratory system [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=v_j-LD2YEqg ↵
The act of breathing.
The movement of air into the lungs (also called inspiration).
Movement of air out of the lungs (also called expiration).
The total number of breaths that occur each minute.
A medical term used for various volumes of air moved by the lungs at a given point of the respiratory cycle.
The amount of air inhaled or exhaled in a normal quiet breath, which averages about 500 milliliters (mL) for a healthy male adult and 400 mL for a healthy female adult.
The extra volume of air that can be forcibly inhaled after a normal inhalation, about 3100 mL.
The extra amount of air that can be forcibly exhaled after a normal exhalation, about 12 mL.
The air left in the lungs after exhaling as much air as possible, averaging about 1200 mL.
The sum of all lung volumes (TV+ ERV+ IRV+ RV), which represents the total amount of air a person can hold in their lungs after a forceful inhalation.
The amount of air a person can move into or out of their lungs, which is the sum of all of the previous volumes described except residual volume (TV+ ERV+ IRV) and is between 4,000 and 5,000 milliliters for adults.
The exchange of gases between the alveoli and pulmonary capillaries.
The exchange of gases between the systemic capillaries and the tissues.
A bright red molecule formed when oxygen binds to hemoglobin in red blood cells, giving oxygenated blood its bright red color.
The majority of carbon dioxide (about 75%) is transported in the blood as bicarbonate (HCO₃⁻) ions.
A compound formed when carbon dioxide binds to hemoglobin in red blood cells, accounting for about 20% of CO₂ transport in the blood.
About 5% of carbon dioxide is transported directly in the blood plasma and diffuses into the alveoli for exhalation.

